Achilles tendon repair: Difference between revisions
m (added a video link) |
No edit summary |
||
| (32 intermediate revisions by 8 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Description< | == Description == | ||
The [[Achilles Tendon]] connects the calf muscles to the calcaneus (heel bone) and is one of the important tendons in the human body. The main action of the Achilles tendon is foot plantar flexion. Common pathologies include: [[tendinopathy]], tear or [[Achilles Rupture|rupture]]. Examples of mechanisms of injury for rupture includes: falling from a height, forceful plantar flexion of the ankle (as in jumping with an extended knee), or using the foot to break a fall if you stumble<ref name=":0" />. Clinically they present with a palpable gap on palpation, increased passive dorsiflexion, lack of heel raise and a positive [[Thompson Test]]<ref name=":0">Chiodo CP, Glazebrook M, Bluman EM, Cohen BE, Femino JE, Giza E, Watters III WC, Goldberg MJ, Keith M, Haralson III RH, Turkelson CM. [https://journals.lww.com/jbjsjournal/fulltext/2010/10200/american_academy_of_orthopaedic_surgeons_clinical.13.aspx American Academy of Orthopaedic Surgeons clinical practice guideline on the treatment of Achilles tendon rupture]. JBJS. 2010 Oct 20;92(14):2466-8.</ref>. Achilles tendon rupture is either managed conservatively with a cast or surgically with an '''Achilles tendon repair'''. | |||
[[ | [[Achilles Rupture|For more details on Achilles Tendon Rupture visit this page]]. | ||
= | {{#ev:youtube|Kr84-NEoYiE}} <ref>AAOSOnlinePubs. Achilles Tendon Rupture. Available from: https://www.youtube.com/watch?v=Kr84-NEoYiE [last accessed 10/6/2021]</ref> | ||
== Conservative vs Surgical Intervention == | |||
There is much debate in the literature about treatment for achilles tendon rupture with the two options comprising of a conservative or surgical approach. Many studies have shown that the re-rupture rates are higher in cases of non-operative management. More recently studies have demonstrated equivalent or improved rates of re-rupture compare with surgical intervention<ref>Gulati V, Jaggard M, Al-Nammari SS, Uzoigwe C, Gulati P, Ismail N, Gibbons C, Gupte C. [https://www.ncbi.nlm.nih.gov/pmc/articles/pmc4436906/ Management of achilles tendon injury: a current concepts systematic review.] World journal of orthopedics. 2015 May 18;6(4):380.</ref><ref>Willits K, Amendola A, Bryant D, Mohtadi NG, Giffin JR, Fowler P, Kean CO, Kirkley A. [https://journals.lww.com/jbjsjournal/fulltext/2010/12010/Operative_versus_Nonoperative_Treatment_of_Acute.1.aspx Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation.] JBJS. 2010 Dec 1;92(17):2767-75.</ref>. However, many people continue to be treated with surgical repair and physiotherapists will continue to see them for post-operative rehabilitation in their clinics. | |||
[[Achilles Rupture|Visit the achilles tendon rupture page for information on conservative management]]. | |||
== Pre-op == | == Pre-op == | ||
Prior to surgery general | Prior to surgery general oedema reduction interventions should be utilised ([[RICE|Rest, Ice, Compression, Elevation]]). The surgery will ideally occur within one week of the rupture. | ||
== Surgery Description == | == Surgery Description == | ||
[[File:RMP1.jpg|right|frameless]] | |||
Many techniques exist for this surgery, including transverse, medial and longitudinal incisions. The ankle is placed in a neutral position and the severed ends of the tendon are sutured together. The surgeon will then take the ankle through complete range of motion to look at the integrity of the repair. A cast is often applied, with the surgical technique determining how long the cast stays on<ref name="Dutton" />. Many surgeons are now focusing on early weight-bearing and passive motion to improve tendon healing. A new minimally-invasive technique involves the utilisation of the peroneus brevis via two para-midline incisions. The technique reportedly preserves skin integrity over the site most prone to breakdown in a vertical incision, open reconstruction.<ref>Carmont MR, Maffulli N. [https://link.springer.com/article/10.1186/1471-2474-8-100 Less invasive Achilles tendon reconstruction.] BMC Musculoskeletal Disorders. 2007 Dec;8(1):1-7.</ref> Another study recommended percutaneous repair in the recreational athlete and in patients concerned with cosmesis, and open repair for all high-caliber athletes who cannot afford any chance of re-rupture."<ref>Bradley JP, Tibone JE. [https://journals.sagepub.com/doi/abs/10.1177/036354659001800213 Percutaneous and open surgical repairs of Achilles tendon ruptures: a comparative study.] The American journal of sports medicine. 1990 Mar;18(2):188-95.</ref>{{#ev:youtube|0DNeeGuHKGU|300}} | |||
[[ | == Post-Op == | ||
Early mobilisation following achilles tendon repair has been reported to be beneficial in terms of postoperative recovery and improved tendon vascularity. Despite the increasing support for accelerated rehabilitation regimes, there is still no consensus regarding the most preferable protocol. Protocols have been developed by Brumann et al<ref>Brumann M, Baumbach SF, Mutschler W, Polzer H. [https://www.sciencedirect.com/science/article/pii/S0020138314003155 Accelerated rehabilitation following Achilles tendon repair after acute rupture–development of an evidence-based treatment protocol.] Injury. 2014 Nov 1;45(11):1782-90.</ref> and Braunstein et al<ref>Braunstein M, Baumbach SF, Boecker W, Carmont MR, Polzer H. [https://link.springer.com/article/10.1007/s00167-015-3795-1 Development of an accelerated functional rehabilitation protocol following minimal invasive Achilles tendon repair.] Knee Surgery, Sports Traumatology, Arthroscopy. 2018 Mar;26(3):846-53.</ref> | |||
See the following clinic protocols: | |||
*[http://fowlerkennedy.com/wp-content/uploads/2015/11/ACHILLES-TENDON-RUPTURE-ACCELERATED-REHAB-PROTOCOL.pdf Fowler Kennedy] | |||
*[http://indianatotaltherapy.com/wp/wp-content/uploads/2016/05/accelerated_achilles_protocol.pdf Indiana Total Therapy] | |||
*[https://www.ballaratosm.com.au/wp-content/uploads/2017/05/ls_achilles_tendon_rehab_program.pdf Ballart orthopaedics] | |||
Dutton<ref name="Dutton">Dutton M. Orthopaedic Examination, Evaluation, and Intervention. New York, NY:McGraw-Hill:2004.</ref> describes three phases of post-surgical rehabilitation following achilles tendon repair. | |||
====Phase I==== | |||
==== Phase I | |||
Phase I typically lasts three weeks. | Phase I typically lasts three weeks. | ||
Goals of this phase are as follows: | Goals of this phase are as follows: | ||
* | *Control oedema and protect the repair site | ||
* | *Minimise scar adhesion and detrimental effects of immobilisation | ||
* | *Progress to full weight bearing as tolerated/indicated | ||
* | *Pain 5/10 or less, strength 4/5 all lower extremity muscles except plantar flexors | ||
Phase I interventions include: | Phase I interventions include: | ||
* | *Modalities for pain and oedema | ||
* | *Stretching of large lower extremity muscle groups, gastrocnemius/soleus added at week 3 | ||
* | *AROM: plantar and dorsiflexion 3x5; 3 times daily; add inversion and eversion at week 2 | ||
*Foot/ankle isometrics at week 2; band exercises week 3 | |||
* | *Proprioceptive training for lower extremities; Gait training | ||
* | *Upper extremity cardiovascular exercise | ||
* | *Joint mobilisation and soft tissue work, as indicated | ||
* | |||
==== Phase II | ====Phase II==== | ||
Phase II typically lasts from post op week 4-6. | Phase II typically lasts from post-op week 4-6. | ||
Goals for this phase are as follows: | Goals for this phase are as follows: | ||
* | *Normalized gait pattern | ||
* | *Full ankle ROM | ||
* | *5/5 lower extremity strength | ||
* | *Return to full ADL ability | ||
* | *Pain reported to be <2/10 | ||
* | *Proprioceptive reactions equal to non-surgical side | ||
Phase II interventions include: | Phase II interventions include: | ||
* | *Ankle flexibility at various knee angles | ||
* | *Progressive closed kinetic chain lower extremity strengthening | ||
* | *Cardiovascular progression | ||
* | *Proprioceptive training on variety of surfaces | ||
* | *Manual resisted exercises and joint mobilization, as indicated | ||
==== Phase III | ====Phase III==== | ||
Phase III typically lasts from post op week 6-15. | Phase III typically lasts from post op week 6-15. | ||
Goals for this phase are as follows: | Goals for this phase are as follows: | ||
* | *Initiate running program | ||
* | *Improve balance and coordination | ||
* | *Increase velocity of activity | ||
* | *Return to sport | ||
Phase III interventions include: | Phase III interventions include: | ||
* Progressive ankle and lower extremity strengthening | |||
* Agility exercises | |||
* Double heel raise/lower progressing to single leg heel raise at various speeds | |||
A recent systematic review by Brumann and colleagues (2014)<ref name="brumann">Brumann M, Baumbach SF, Mutschler W, Polzer H. [https://www.sciencedirect.com/science/article/pii/S0020138314003155 Accelerated rehabilitation following Achilles tendon repair after acute rupture–development of an evidence-based treatment protocol.] Injury. 2014 Nov 1;45(11):1782-90.</ref> identified the most up-to-date rehabilitation protocol for an achilles tendon repair. They summarised their findings with the following guidelines; | |||
Orthosis fixed at 30° of PF | ==== Week 0 - 2 ==== | ||
* Nil ankle RoM | |||
Progress to full weight bearing (FWB) | * Orthosis fixed at 30° of PF | ||
* Progress to full weight bearing (FWB) | |||
==== Week 3 - 6 ==== | ==== Week 3 - 6 ==== | ||
* FWB | |||
FWB | * Active ankle RoM 0-30° | ||
* Orthosis limited to plantargrade (0° DF) to 30° PF | |||
Active ankle RoM 0-30° | |||
Orthosis limited to plantargrade (0° DF) to 30° PF | |||
==== Week 7+ ==== | ==== Week 7+ ==== | ||
* Full ROM | |||
* Nil orthosis | |||
== References == | |||
<references /> | |||
[[Category:Orthopaedic_Surgical_Procedures]] | |||
[ | |||
[ | |||
Latest revision as of 11:00, 6 October 2021
Original Editor - Matt Anderson.
Top Contributors - Admin, Ben Kasehagen, Darine Mohieldeen, Rachael Lowe, Kim Jackson, Aminat Abolade, WikiSysop, Matt Anderson, Johnathan Fahrner, 127.0.0.1, Tony Lowe, George Prudden, Tobias Meerts and Kai A. Sigel
Description[edit | edit source]
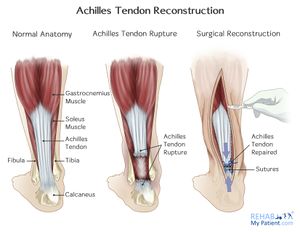
The Achilles Tendon connects the calf muscles to the calcaneus (heel bone) and is one of the important tendons in the human body. The main action of the Achilles tendon is foot plantar flexion. Common pathologies include: tendinopathy, tear or rupture. Examples of mechanisms of injury for rupture includes: falling from a height, forceful plantar flexion of the ankle (as in jumping with an extended knee), or using the foot to break a fall if you stumble[1]. Clinically they present with a palpable gap on palpation, increased passive dorsiflexion, lack of heel raise and a positive Thompson Test[1]. Achilles tendon rupture is either managed conservatively with a cast or surgically with an Achilles tendon repair.
For more details on Achilles Tendon Rupture visit this page.
Conservative vs Surgical Intervention[edit | edit source]
There is much debate in the literature about treatment for achilles tendon rupture with the two options comprising of a conservative or surgical approach. Many studies have shown that the re-rupture rates are higher in cases of non-operative management. More recently studies have demonstrated equivalent or improved rates of re-rupture compare with surgical intervention[3][4]. However, many people continue to be treated with surgical repair and physiotherapists will continue to see them for post-operative rehabilitation in their clinics.
Visit the achilles tendon rupture page for information on conservative management.
Pre-op[edit | edit source]
Prior to surgery general oedema reduction interventions should be utilised (Rest, Ice, Compression, Elevation). The surgery will ideally occur within one week of the rupture.
Surgery Description[edit | edit source]
Many techniques exist for this surgery, including transverse, medial and longitudinal incisions. The ankle is placed in a neutral position and the severed ends of the tendon are sutured together. The surgeon will then take the ankle through complete range of motion to look at the integrity of the repair. A cast is often applied, with the surgical technique determining how long the cast stays on[5]. Many surgeons are now focusing on early weight-bearing and passive motion to improve tendon healing. A new minimally-invasive technique involves the utilisation of the peroneus brevis via two para-midline incisions. The technique reportedly preserves skin integrity over the site most prone to breakdown in a vertical incision, open reconstruction.[6] Another study recommended percutaneous repair in the recreational athlete and in patients concerned with cosmesis, and open repair for all high-caliber athletes who cannot afford any chance of re-rupture."[7]
Post-Op[edit | edit source]
Early mobilisation following achilles tendon repair has been reported to be beneficial in terms of postoperative recovery and improved tendon vascularity. Despite the increasing support for accelerated rehabilitation regimes, there is still no consensus regarding the most preferable protocol. Protocols have been developed by Brumann et al[8] and Braunstein et al[9]
See the following clinic protocols:
Dutton[5] describes three phases of post-surgical rehabilitation following achilles tendon repair.
Phase I[edit | edit source]
Phase I typically lasts three weeks.
Goals of this phase are as follows:
- Control oedema and protect the repair site
- Minimise scar adhesion and detrimental effects of immobilisation
- Progress to full weight bearing as tolerated/indicated
- Pain 5/10 or less, strength 4/5 all lower extremity muscles except plantar flexors
Phase I interventions include:
- Modalities for pain and oedema
- Stretching of large lower extremity muscle groups, gastrocnemius/soleus added at week 3
- AROM: plantar and dorsiflexion 3x5; 3 times daily; add inversion and eversion at week 2
- Foot/ankle isometrics at week 2; band exercises week 3
- Proprioceptive training for lower extremities; Gait training
- Upper extremity cardiovascular exercise
- Joint mobilisation and soft tissue work, as indicated
Phase II[edit | edit source]
Phase II typically lasts from post-op week 4-6.
Goals for this phase are as follows:
- Normalized gait pattern
- Full ankle ROM
- 5/5 lower extremity strength
- Return to full ADL ability
- Pain reported to be <2/10
- Proprioceptive reactions equal to non-surgical side
Phase II interventions include:
- Ankle flexibility at various knee angles
- Progressive closed kinetic chain lower extremity strengthening
- Cardiovascular progression
- Proprioceptive training on variety of surfaces
- Manual resisted exercises and joint mobilization, as indicated
Phase III[edit | edit source]
Phase III typically lasts from post op week 6-15.
Goals for this phase are as follows:
- Initiate running program
- Improve balance and coordination
- Increase velocity of activity
- Return to sport
Phase III interventions include:
- Progressive ankle and lower extremity strengthening
- Agility exercises
- Double heel raise/lower progressing to single leg heel raise at various speeds
A recent systematic review by Brumann and colleagues (2014)[10] identified the most up-to-date rehabilitation protocol for an achilles tendon repair. They summarised their findings with the following guidelines;
Week 0 - 2[edit | edit source]
- Nil ankle RoM
- Orthosis fixed at 30° of PF
- Progress to full weight bearing (FWB)
Week 3 - 6[edit | edit source]
- FWB
- Active ankle RoM 0-30°
- Orthosis limited to plantargrade (0° DF) to 30° PF
Week 7+[edit | edit source]
- Full ROM
- Nil orthosis
References[edit | edit source]
- ↑ 1.0 1.1 Chiodo CP, Glazebrook M, Bluman EM, Cohen BE, Femino JE, Giza E, Watters III WC, Goldberg MJ, Keith M, Haralson III RH, Turkelson CM. American Academy of Orthopaedic Surgeons clinical practice guideline on the treatment of Achilles tendon rupture. JBJS. 2010 Oct 20;92(14):2466-8.
- ↑ AAOSOnlinePubs. Achilles Tendon Rupture. Available from: https://www.youtube.com/watch?v=Kr84-NEoYiE [last accessed 10/6/2021]
- ↑ Gulati V, Jaggard M, Al-Nammari SS, Uzoigwe C, Gulati P, Ismail N, Gibbons C, Gupte C. Management of achilles tendon injury: a current concepts systematic review. World journal of orthopedics. 2015 May 18;6(4):380.
- ↑ Willits K, Amendola A, Bryant D, Mohtadi NG, Giffin JR, Fowler P, Kean CO, Kirkley A. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. JBJS. 2010 Dec 1;92(17):2767-75.
- ↑ 5.0 5.1 Dutton M. Orthopaedic Examination, Evaluation, and Intervention. New York, NY:McGraw-Hill:2004.
- ↑ Carmont MR, Maffulli N. Less invasive Achilles tendon reconstruction. BMC Musculoskeletal Disorders. 2007 Dec;8(1):1-7.
- ↑ Bradley JP, Tibone JE. Percutaneous and open surgical repairs of Achilles tendon ruptures: a comparative study. The American journal of sports medicine. 1990 Mar;18(2):188-95.
- ↑ Brumann M, Baumbach SF, Mutschler W, Polzer H. Accelerated rehabilitation following Achilles tendon repair after acute rupture–development of an evidence-based treatment protocol. Injury. 2014 Nov 1;45(11):1782-90.
- ↑ Braunstein M, Baumbach SF, Boecker W, Carmont MR, Polzer H. Development of an accelerated functional rehabilitation protocol following minimal invasive Achilles tendon repair. Knee Surgery, Sports Traumatology, Arthroscopy. 2018 Mar;26(3):846-53.
- ↑ Brumann M, Baumbach SF, Mutschler W, Polzer H. Accelerated rehabilitation following Achilles tendon repair after acute rupture–development of an evidence-based treatment protocol. Injury. 2014 Nov 1;45(11):1782-90.