Accessory Navicular Bone: Difference between revisions
No edit summary |
Oyemi Sillo (talk | contribs) mNo edit summary |
||
| (24 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors ''' - [[User:Carlos De Coster|Carlos De Coster]] | '''Original Editors ''' - [[User:Carlos De Coster|Carlos De Coster]] as part of the [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel Evidence-Based Practice Project]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
[[File:Normal-Navicular-and-Accessory-Navicular.jpg|alt=|right|241x241px]] | |||
An accessory navicular is a large accessory ossicle that can be present adjacent to the medial side of the [[Navicular|navicular bone]]. The accessory navicular [[bone]] presents as a [[sesamoid]] in the [[Tibialis Posterior|posterior tibial tendon]], in articulation with the navicular<ref name="p1">Raymond T., Morrissy and Stuart L.Weinstein .Lovell, Winter’s Padiatric Orthopaedics. United States: Lippincot William’s Wilkin Publication, 2005.</ref> or as an enlargement of the navicular itself. | |||
== Epidemiology == | |||
[[File:Foot superior.png|thumb|200x200px|Navicular bone green ]] | |||
The prevalence of an accessory navicular bone is ~10% (range 4-21%), although may be substantially higher (~45%) in Asian populations. | |||
* Appears first in adolescence | |||
* Is common in female patients | |||
* Bilateral prevalence is ~70% (range 50-90%)<ref name=":0">Radiopedia Accessory navicular Available:https://radiopaedia.org/articles/accessory-navicular-2?lang=us (accessed 8.6.2022)</ref> | |||
[[ | == Classification == | ||
[[File:Os-naviculare-diagrams-1.jpeg|right|frameless]] | |||
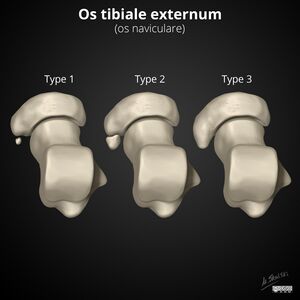
The Geist classification divides these into three types: | |||
# sesamoid bone in the posterior tibialis tendon. There is a small gap of approximately 3mm or less between the sesamoid and the navicular. | |||
# consists of an accessory bone, up to 1.2cm in diameter, where synchondrosis develops between it and the navicular. | |||
# is the fused accessory navicular resulting in a large cornuate shaped navicular<ref name=":0" />.<br> | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
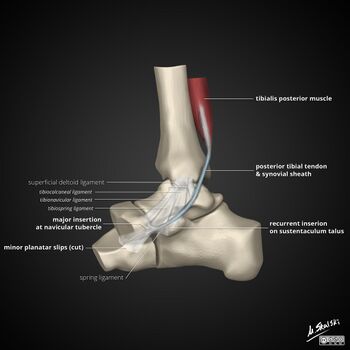
[[File:Tibialis-posterior-tendon-anatomy.jpg|right|frameless|350x350px]] | |||
An accessory navicular bone is located posterior to the posteromedial tuberosity of the tarsal navicular bone. The tibialis posterior tendon inserts into the navicular bone. Tibialis posterior is an inverter of the foot, assists in the plantar flexion of the foot at the [[Ankle and Foot|ankle]] and also has a major role in supporting the medial [[Arches of the Foot|arch]] of the foot. This can be compromised where there exists an abnormal insertion of the tendon into the accessory navicular bone and result in a loss of suspension of the tibialis posterior tendon<ref name="p4">Golano P., ‘The anatomy of the navicular and periarticular structures.’ Foot Ankle Clinics, 2004, March, vol. 9, p. 1-23.</ref><ref name="p5">Kiter E., Erdan N., Karatosun V., Gunall I., ‘Tibialis posterior tendon abnormalities in feet with accessory navicular bone and flatfoot’. Acta orthopaedica Scandinavia, 1999, December, vol. 70, p. 618-621</ref><ref name="p6" /><ref name="p7">Kidner FC. The prehallux (accessory scaphoid) in its relation to flat-foot. J Bone Joint Surg 1929 : II : 831</ref>. <br>The presence of a type I or II accessory navicular is also a cause of [[Posterior Tibial Tendon Dysfunction|Posterior Tibial tendinopathy]] as the insertion of the tibialis posterior tendon onto the accessory navicular is more proximal. Leverage of the malleolus on the tibialis posterior tendon is reduced increasing stress on the tendon. <ref name="p9">A. Bernaerts, F.M. Vanhoenacker, S. Van de Perre, A.M. De Schepper, P.M. Parizel1 Accessory navicular bone: Not Such a normal variant. JBR–BTR, 2004, 87 (5) page 250-252</ref> The calcaneal pitch angle is also reduced in patients with a symptomatic accessory navicular than in normal subjects.<ref name="p0">Prichausuk S, Sinphurmsukskul O: Kinder Procedure for symptomatic accessory navicular and its relation to pes planus, Foot Ankle 16:500,1995</ref> | |||
[[ | == Clinical Presentation == | ||
[[File:Lateral_veiw_AN.jpg|alt=|thumb|179x179px|Lateral view AN]] | |||
Most of the time it is asymptomatic and found incidentally on radiographs, although medial side foot pain (accessory navicular syndrome) is the most common presenting feature of accessory navicular bone. The pain is aggravated by walking, running and weight-bearing activities. When large, it can protrude medially and cause friction against footwear<ref name=":0" />. | |||
== Differential Diagnosis == | |||
== Differential Diagnosis | |||
*Stress fracture | *Stress fracture | ||
* | *Tendinopathy | ||
*Medial tuberosity fracture <ref name="p5"/> | *Medial tuberosity fracture <ref name="p5" /> | ||
* | *Bone Tumor | ||
*Kohler’s disease <ref name="p6"/><br> | *Kohler’s disease <ref name="p6" /><br> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
[[File:AP_veiw_AN.jpg|alt=|thumb|337x337px|AP veiw AN]] | |||
Radiographs show a medial navicular eminence that is best visualized on the lateral-oblique view. Symptomatic accessory navicular bones may appear as a 'hot spot' on bone scan and on MRI bone marrow edema can be seen<ref name=":0" />. | |||
When examining the lateral weight bearing X-ray, alignment of the talonavicular cuneiform and first metatarsal dorsal should be carefully examined as well. [[Navicular Drop Test|“Sag”]] at this joint indicates structural integrity of the area. | |||
== Examination == | == Examination == | ||
[[File:Oblique_veiw_AN.jpg|alt=|thumb|Oblique view AN]] | |||
Patients with an accessory navicular may present with complex pain patterns requiring a thorough examination. <ref name="p7" /> The examination should include key assessments: | |||
*Differentiation of the navicular prominence from the [[Talus|talar]] head prominence in flat foot deformities by inverting and everting through the subtalar joint with a thumb over the bony prominence.<ref name="p8">Kidner FC. Pre-hallux in relation to flatfoot. JAMA 1933; 101: 1539-42.</ref> | |||
*Assessing for any loss of structural integrity of the longitudinal arch is important as this component of the deformity will not be corrected by surgical intervention. Surgery is performed to correct navicular deformity and is dependent on the severity of symptoms when conservative management has not been successful (see interventions below). <ref name="p9" /> | |||
*Differentiation of navicular prominence from talar head prominence in flat foot | *Thorough [[gait]] examination.<br> | ||
* | |||
* | |||
== Medical Management == | == Medical Management == | ||
Conservative: | |||
#Physical therapy | #Physical therapy | ||
# | #Acute pain can be managed by corticosteroid injection and immobilization of the foot for 2-3 weeks. For refractory cases.<ref name=":0" /> | ||
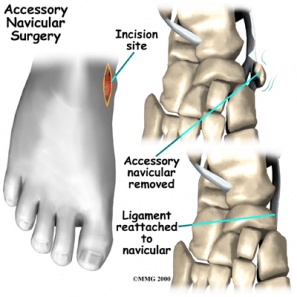
[[File:Accessory_navicular_surgery.jpg|alt=|right|297x297px]] | |||
Surgical management can be considered. There are 2 surgeries that can be performed depending upon the condition and symptoms | |||
# A simple surgical excision to remove the accessory navicular along with its prominence. In this procedure, the incision is made dorsally to the prominence of the accessory navicular. Symptoms are relieved in 90% of cases.<ref>Kulkarni. G.S. Textbook of orthopedics and trauma.India: Jaypee Brother Publication, 1999.&lt;/ref&gt;&lt;ref name="p7"&gt;Kidner FC. The prehallux (accessory scaphoid) in its relation to flat-foot. J Bone Joint Surg 1929 : II : 831</ref> | |||
There are 2 surgeries that can be performed depending upon the condition and symptoms | |||
# The 2nd procedure excising the boney prominence in conjunction with reattachment of the posterior tibial tendon. .<ref name="p6">Kulkarni. G.S. Textbook of orthopedics and trauma.India: Jaypee Brother Publication, 1999</ref><ref name="p7" /> The posterior tibial tendon is split and is reattached further up the medial side of foot to provide increased support to the longitudinal arch. | |||
After surgery the lower leg is put into a cast for 4 weeks, which is moulded into the shape of the arch, with the foot maintained in a plantigrade position. Partial weight bearing is indicated for 8 weeks after which full weight bearing is permitted.<ref name="p7" /><ref name="p9" />. Once the cast is removed, a strength and conditioning programme is highly recommended. <ref name="p8" /> | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
[[File:Download (2).jpg|thumb|Pes Plunus]] | |||
If the accessory navicular bone becomes problematic, physical therapy may be prescribed. This includes use of therapeutic modalities to relieve pain, increase strength and stability in the foot. An accessory navicular bone is often linked to posterior tibial dysfunction and [[Pes Planus|pes planus]]. In some cases orthotics may be indicated. | |||
*Well padded shoe orthotics should be worn for arch support. This decreases direct pressure over the navicular. | |||
*Strength and conditioning exercises for the [[Peroneus (Fibularis) Longus Muscle|fibularis]] and posterior tibialis muscles. | |||
*Strengthening of the intrinsic foot muscles and the lateral rotators of the pelvis.<ref name="p9" /> | |||
*Activity modification in the initial stages, such as limiting or stopping any strenuous activities which may cause the accessory navicular bone to become symptomatic.<ref name="p9" /> | |||
*Gait re-training and stability exercises.<br> | |||
Some examples of functional posterior tibialis strengthening: | |||
<div class="row"> | |||
<div class="col-md-6">{{#ev:youtube|zmh1FisBeeM|300}} <ref>ShaychiITA. Tibialis Posterior Basic Strengthening. Available from: http://www.youtube.com/watch?v=zmh1FisBeeM [last accessed 24/11/12]</ref> </div> | |||
<div class="col-md-6">{{#ev:youtube|qv76eBxGQXI|300}} <ref>ShaychiITA. Tibialis Posterior Basic Multiplanar Strengthening. Available from: http://www.youtube.com/watch?v=qv76eBxGQXI [last accessed 01/12/12]</ref></div> | |||
</div> | |||
<div class="row"> | |||
<div class="col-md-6">{{#ev:youtube|1C_C5N9reB8|300}}<ref>ShaychiITA. Tibialis Posterior Functional Strengthening: Full Body Weight Maintaining Supination. Available from: http://www.youtube.com/watch?v=1C_C5N9reB8[last accessed 01/12/12]|}</ref> </div> | |||
<div class="col-md-6">{{#ev:youtube|TdHgyFZbOPk|300}}<ref>ShaychiITA. Tibialis Posterior Functional Strengthening: Maintain Arch with Compass Squats. Available from: http://www.youtube.com/watch?v=TdHgyFZbOPk[last accessed 24/11/12]|}</ref></div> | |||
</div> | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
A type I accessory navicular is rarely symptomatic. Where symptoms do appear, type I usually responds well to conservative management. Patients with Type II have an increased risk of injury and onset is usually insidious or as a result of trauma. It fails to respond to conservative treatment when severe and fusion of the accessory navicular to the navicular may successfully relieve pain without disrupting the tibialis posterior tendon insertion.<ref name="p2">Shands AR Jr, Wentz IJ. Congenital anomalies, accessory bones and osteochondritis in the feet of 850 children. Surg.Clin.North Am 1953:97:1643-1666</ref> With Type III, excising the accessory navicular is indicated over excising the navicular prominence.<ref name="p9" /> | |||
Type III | |||
== References == | == References == | ||
| Line 155: | Line 94: | ||
<references /> | <references /> | ||
[[Category:Foot]][[Category:Bones]][[Category:Musculoskeletal/Orthopaedics|Orthopaedics]][[Category:Vrije_Universiteit_Brussel_Project]][[Category: | [[Category:Foot]] | ||
[[Category:Bones]] | |||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
[[Category:Anatomy]] | |||
[[Category:Vrije_Universiteit_Brussel_Project]] | |||
[[Category:Foot - Anatomy]] | |||
[[Category:Foot - Bones]] | |||
Latest revision as of 19:38, 21 April 2023
Original Editors - Carlos De Coster as part of the Vrije Universiteit Brussel Evidence-Based Practice Project
Top Contributors - Aarti Sareen, Admin, Carlos De Coster, Scott Cornish, Kim Jackson, Lucinda hampton, Laura Ritchie, WikiSysop, 127.0.0.1, Evan Thomas, Tony Lowe and Oyemi Sillo
Introduction[edit | edit source]
An accessory navicular is a large accessory ossicle that can be present adjacent to the medial side of the navicular bone. The accessory navicular bone presents as a sesamoid in the posterior tibial tendon, in articulation with the navicular[1] or as an enlargement of the navicular itself.
Epidemiology[edit | edit source]
The prevalence of an accessory navicular bone is ~10% (range 4-21%), although may be substantially higher (~45%) in Asian populations.
- Appears first in adolescence
- Is common in female patients
- Bilateral prevalence is ~70% (range 50-90%)[2]
Classification[edit | edit source]
The Geist classification divides these into three types:
- sesamoid bone in the posterior tibialis tendon. There is a small gap of approximately 3mm or less between the sesamoid and the navicular.
- consists of an accessory bone, up to 1.2cm in diameter, where synchondrosis develops between it and the navicular.
- is the fused accessory navicular resulting in a large cornuate shaped navicular[2].
Clinically Relevant Anatomy[edit | edit source]
An accessory navicular bone is located posterior to the posteromedial tuberosity of the tarsal navicular bone. The tibialis posterior tendon inserts into the navicular bone. Tibialis posterior is an inverter of the foot, assists in the plantar flexion of the foot at the ankle and also has a major role in supporting the medial arch of the foot. This can be compromised where there exists an abnormal insertion of the tendon into the accessory navicular bone and result in a loss of suspension of the tibialis posterior tendon[3][4][5][6].
The presence of a type I or II accessory navicular is also a cause of Posterior Tibial tendinopathy as the insertion of the tibialis posterior tendon onto the accessory navicular is more proximal. Leverage of the malleolus on the tibialis posterior tendon is reduced increasing stress on the tendon. [7] The calcaneal pitch angle is also reduced in patients with a symptomatic accessory navicular than in normal subjects.[8]
Clinical Presentation[edit | edit source]
Most of the time it is asymptomatic and found incidentally on radiographs, although medial side foot pain (accessory navicular syndrome) is the most common presenting feature of accessory navicular bone. The pain is aggravated by walking, running and weight-bearing activities. When large, it can protrude medially and cause friction against footwear[2].
Differential Diagnosis[edit | edit source]
Diagnostic Procedures[edit | edit source]
Radiographs show a medial navicular eminence that is best visualized on the lateral-oblique view. Symptomatic accessory navicular bones may appear as a 'hot spot' on bone scan and on MRI bone marrow edema can be seen[2].
When examining the lateral weight bearing X-ray, alignment of the talonavicular cuneiform and first metatarsal dorsal should be carefully examined as well. “Sag” at this joint indicates structural integrity of the area.
Examination[edit | edit source]
Patients with an accessory navicular may present with complex pain patterns requiring a thorough examination. [6] The examination should include key assessments:
- Differentiation of the navicular prominence from the talar head prominence in flat foot deformities by inverting and everting through the subtalar joint with a thumb over the bony prominence.[9]
- Assessing for any loss of structural integrity of the longitudinal arch is important as this component of the deformity will not be corrected by surgical intervention. Surgery is performed to correct navicular deformity and is dependent on the severity of symptoms when conservative management has not been successful (see interventions below). [7]
- Thorough gait examination.
Medical Management[edit | edit source]
Conservative:
- Physical therapy
- Acute pain can be managed by corticosteroid injection and immobilization of the foot for 2-3 weeks. For refractory cases.[2]
Surgical management can be considered. There are 2 surgeries that can be performed depending upon the condition and symptoms
- A simple surgical excision to remove the accessory navicular along with its prominence. In this procedure, the incision is made dorsally to the prominence of the accessory navicular. Symptoms are relieved in 90% of cases.[10]
- The 2nd procedure excising the boney prominence in conjunction with reattachment of the posterior tibial tendon. .[5][6] The posterior tibial tendon is split and is reattached further up the medial side of foot to provide increased support to the longitudinal arch.
After surgery the lower leg is put into a cast for 4 weeks, which is moulded into the shape of the arch, with the foot maintained in a plantigrade position. Partial weight bearing is indicated for 8 weeks after which full weight bearing is permitted.[6][7]. Once the cast is removed, a strength and conditioning programme is highly recommended. [9]
Physical Therapy Management[edit | edit source]
If the accessory navicular bone becomes problematic, physical therapy may be prescribed. This includes use of therapeutic modalities to relieve pain, increase strength and stability in the foot. An accessory navicular bone is often linked to posterior tibial dysfunction and pes planus. In some cases orthotics may be indicated.
- Well padded shoe orthotics should be worn for arch support. This decreases direct pressure over the navicular.
- Strength and conditioning exercises for the fibularis and posterior tibialis muscles.
- Strengthening of the intrinsic foot muscles and the lateral rotators of the pelvis.[7]
- Activity modification in the initial stages, such as limiting or stopping any strenuous activities which may cause the accessory navicular bone to become symptomatic.[7]
- Gait re-training and stability exercises.
Some examples of functional posterior tibialis strengthening:
Clinical Bottom Line[edit | edit source]
A type I accessory navicular is rarely symptomatic. Where symptoms do appear, type I usually responds well to conservative management. Patients with Type II have an increased risk of injury and onset is usually insidious or as a result of trauma. It fails to respond to conservative treatment when severe and fusion of the accessory navicular to the navicular may successfully relieve pain without disrupting the tibialis posterior tendon insertion.[15] With Type III, excising the accessory navicular is indicated over excising the navicular prominence.[7]
References[edit | edit source]
- ↑ Raymond T., Morrissy and Stuart L.Weinstein .Lovell, Winter’s Padiatric Orthopaedics. United States: Lippincot William’s Wilkin Publication, 2005.
- ↑ 2.0 2.1 2.2 2.3 2.4 Radiopedia Accessory navicular Available:https://radiopaedia.org/articles/accessory-navicular-2?lang=us (accessed 8.6.2022)
- ↑ Golano P., ‘The anatomy of the navicular and periarticular structures.’ Foot Ankle Clinics, 2004, March, vol. 9, p. 1-23.
- ↑ 4.0 4.1 Kiter E., Erdan N., Karatosun V., Gunall I., ‘Tibialis posterior tendon abnormalities in feet with accessory navicular bone and flatfoot’. Acta orthopaedica Scandinavia, 1999, December, vol. 70, p. 618-621
- ↑ 5.0 5.1 5.2 Kulkarni. G.S. Textbook of orthopedics and trauma.India: Jaypee Brother Publication, 1999
- ↑ 6.0 6.1 6.2 6.3 Kidner FC. The prehallux (accessory scaphoid) in its relation to flat-foot. J Bone Joint Surg 1929 : II : 831
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 A. Bernaerts, F.M. Vanhoenacker, S. Van de Perre, A.M. De Schepper, P.M. Parizel1 Accessory navicular bone: Not Such a normal variant. JBR–BTR, 2004, 87 (5) page 250-252
- ↑ Prichausuk S, Sinphurmsukskul O: Kinder Procedure for symptomatic accessory navicular and its relation to pes planus, Foot Ankle 16:500,1995
- ↑ 9.0 9.1 Kidner FC. Pre-hallux in relation to flatfoot. JAMA 1933; 101: 1539-42.
- ↑ Kulkarni. G.S. Textbook of orthopedics and trauma.India: Jaypee Brother Publication, 1999.</ref><ref name="p7">Kidner FC. The prehallux (accessory scaphoid) in its relation to flat-foot. J Bone Joint Surg 1929 : II : 831
- ↑ ShaychiITA. Tibialis Posterior Basic Strengthening. Available from: http://www.youtube.com/watch?v=zmh1FisBeeM [last accessed 24/11/12]
- ↑ ShaychiITA. Tibialis Posterior Basic Multiplanar Strengthening. Available from: http://www.youtube.com/watch?v=qv76eBxGQXI [last accessed 01/12/12]
- ↑ ShaychiITA. Tibialis Posterior Functional Strengthening: Full Body Weight Maintaining Supination. Available from: http://www.youtube.com/watch?v=1C_C5N9reB8[last accessed 01/12/12]|}
- ↑ ShaychiITA. Tibialis Posterior Functional Strengthening: Maintain Arch with Compass Squats. Available from: http://www.youtube.com/watch?v=TdHgyFZbOPk[last accessed 24/11/12]|}
- ↑ Shands AR Jr, Wentz IJ. Congenital anomalies, accessory bones and osteochondritis in the feet of 850 children. Surg.Clin.North Am 1953:97:1643-1666