Asthma: Difference between revisions
No edit summary |
No edit summary |
||
| (176 intermediate revisions by 18 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- | '''Original Editor '''- [[Open Physio]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}|Akano Oluwadara Tomisin=}} | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | </div> | ||
== | == Introduction == | ||
[[File:Asthma attack-illustration NIH.jpeg|right|frameless|451x451px]] | |||
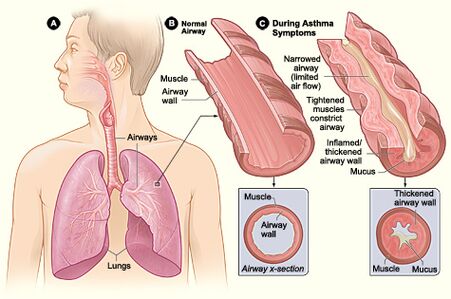
Asthma is a | Asthma is a relatively common condition characterised by at least partially reversible inflammation of the airways and reversible airway obstruction due to airway hyperreactivity. It can be acute, subacute or chronic<ref name=":2">Radiopedia Asthma Available from:https://radiopaedia.org/articles/asthma-1 (accessed 25.5.2021)</ref> and [[Exercise Induced Asthma|exercise induced]]. | ||
Asthma: | |||
== | * Is a major noncommunicable disease (NCD) affecting children and adults. | ||
* Affects an estimated 262 million people in 2019 and caused 461000 deaths.<ref name=":2" /> | |||
* Is the most common chronic disease among children. | |||
* Symptoms can be controlled by inhaled medication and allow people with asthma to lead a normal, active life. | |||
* Trigger avoidance can also help to reduce asthma symptoms. | |||
* Related deaths mostly occur in low- and lower-middle-income countries, where under-diagnosis and under-treatment is a challenge.<ref name=":3">WHO Asthma Available from: https://www.who.int/news-room/fact-sheets/detail/asthma<nowiki/>(accessed 25.5.2021)</ref> | |||
== Epidemiology == | |||
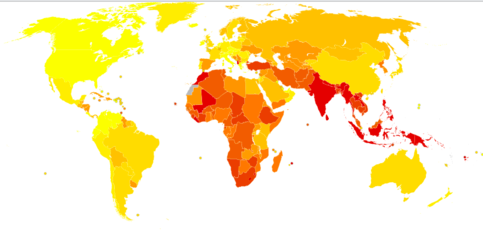
[[File:Asthma death 2012.png|483x483px|thumb|Deaths from Asthma in 2012 per million persons. Statistics from WHO grouped by deciles. Lightest yellow 0-10 through to red 96-251]] | |||
Asthma is one of the most common chronic diseases in the world. It is a common pathology, affecting around 15% to 20% of people in developed countries and around 2% to 4% in less developed countries. It is significantly more common in children.<ref name=":4">Hashmi MF, Tariq M, Cataletto ME, Hoover EL. [https://www.ncbi.nlm.nih.gov/books/NBK430901/ Asthma] 2020.Available from:https://www.ncbi.nlm.nih.gov/books/NBK430901/ (accessed 25.5.2021)</ref> | |||
Asthma: | |||
* Affected an estimated 262 million people in 2019 and caused 461000 deaths.<ref name=":3" /> | |||
* May occur at any age (significantly more common in children), most patients with asthma experience their first symptoms before the age of 5 years old and about 66% are diagnosed before the age of 18 years. | |||
* Almost 50% of children with asthma have a decrease in severity or disappearance of symptoms during early adulthood.<ref name=":2" /> | |||
* Prevalence is greater in extreme ages due to airway responsiveness and lower levels of lung function<ref name=":4" />. | |||
* In many countries, including the US, kills one out of every 100,000 persons. | |||
* Results in millions of school and workdays lost. In the US alone, approximately 2 million asthmatics seek regular care in the emergency department, which increases healthcare costs<ref name=":4" />. | |||
== Aetiology == | |||
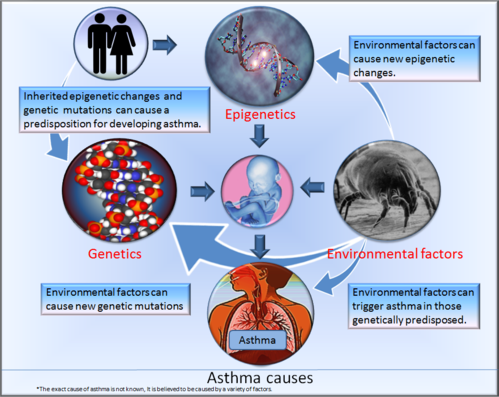
== | Inflammation plays a major role in asthma and involves multiple cell types and mediators. The factors that initiate the inflammatory process are complex and still under investigation. Genetic factors (e.g. [[Cytokines|cytokine]] response profiles) and environmental exposures (such as allergens, pollution, [[Communicable Diseases|infections]], microbes, [[Stress and Health|stress]]) at a crucial time in the development of the [[Immune System|immune system]] are known to be involved.<ref name=":2" /> | ||
== Risk Factors == | |||
[[File:Asthma causes.png|right|frameless|499x499px]] | |||
* | * Asthma is more likely if other family members also have asthma – particularly a close relative, such as a parent or sibling. | ||
* | * Asthma is more likely in people that have other allergic conditions, eczema and rhinitis (hay fever). | ||
* Urbanisation is associated with increased asthma prevalence, probably due to multiple lifestyle factors. | |||
* Events in early life affect the developing lungs and can increase the risk of asthma. E.g. low birth weight, prematurity, exposure to tobacco smoke and other sources of air pollution, and viral respiratory infections. | |||
* Exposures to a range of environmental allergens and irritants are also thought to increase the risk of asthma, eg indoor and outdoor air pollution, house dust mites, moulds, and occupational exposure to chemicals, fumes, or dust. | |||
* Children and adults who are overweight or obese are at a greater risk of asthma. | |||
== Pathophysiology == | |||
[[File:Pathology.jpg|alt=|right|frameless|399x399px]] | |||
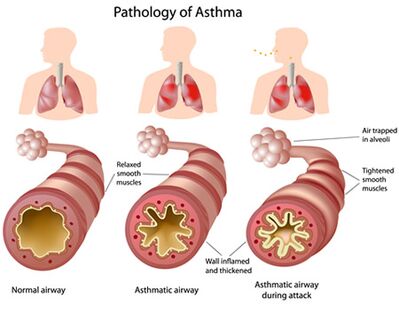
Asthma is a condition of acute, fully reversible airway inflammation, often following exposure to an environmental trigger. The pathological process begins with the inhalation of an irritant (e.g., cold air) or an allergen (e.g., pollen), which then, due to bronchial hypersensitivity, leads to airway inflammation and an increase in mucus production. This leads to a significant increase in airway resistance, which is most pronounced on expiration. | |||
Airway obstruction occurs due to the combination of: | |||
# Inflammatory cell infiltration. | |||
# Mucus hypersecretion with mucus plug formation. | |||
# Smooth muscle contraction. | |||
These reversible changes may become irreversible over time due to | |||
# Basement membrane thickening, collagen deposition, and epithelial desquamation. | |||
# Airway remodelling occurs in chronic disease with smooth muscle hypertrophy and hyperplasia. | |||
If not corrected rapidly, asthma may become more difficult to treat, as the mucus production prevents the inhaled medication from reaching the mucosa. The inflammation also becomes more edematous. This process is resolved (in theory complete resolution is required in asthma, but in practice, this is not checked or tested) with beta-2 agonists (e.g., salbutamol, salmeterol, albuterol) and can be aided by muscarinic receptor antagonists (e.g., ipratropium bromide), which act to reduce the inflammation and relax the bronchial musculature, as well as reducing mucus production.<ref name=":4" /> | |||
== Clinical Presentation == | |||
| | The classic symptoms of asthma are wheezing, [[Dyspnoea|shortness of breath]], chest tightness or difficulty [[Breathing Pattern Disorders|breathing]] and cough. These symptoms are typically variable and can be absent for long periods, with possible episodic exacerbations often triggered by factors such as exercise, allergen or irritant exposure, cold air or [[Viral Infections|viral]] respiratory infections. | ||
| | |||
The diagnosis of asthma is clinical and relies on characteristic patterns or respiratory symptoms recognition and signs in the absence of an alternative explanation. Features that increase the probability of asthma are: | |||
* More than one of the following symptoms: wheezing, cough, difficulty breathing and chest tightness. | |||
* Episodic symptoms that are worse at night and in the early morning, and occur in response to certain triggers, e.g. [[Exercise Induced Asthma|exercise]], allergen exposure, cold air. | |||
* Personal history of an atopic disorder or family history of an atopic (allergic) disorder and/or asthma | |||
* Widespread wheeze on [[auscultation]] | |||
* | * [[Pulmonary Function Test|Lung function tests]] are useful in the evaluation of a patient with asthma to assess the presence, severity and reversibility of the airflow obstruction. On [[spirometry]] an FEV1/FEV ratio less than 0.7 confirms obstruction. In asthmatic patients, there is usually a large bronchodilator response (typically an increase of at least 12-15% in FEV1) 3, and also typically an abnormally high variability of the peak expiratory flow. A normal spirometry, particularly if performed when the patient is asymptomatic, does not exclude the diagnosis of asthma<ref name=":2" /><br> | ||
'''When does asthma become life threatening?''' | '''When does asthma become life threatening?''' | ||
| Line 72: | Line 79: | ||
*Nasal flaring and constant wheeze | *Nasal flaring and constant wheeze | ||
When these signs and symptoms | When these signs and symptoms present, a person should be aware and advised to consult with their general practitioner as soon as possible. | ||
== Investigations and Diagnosis == | |||
Diagnosis of asthma is confirmed based upon various factors<ref>National heart, lung and blood institute. Asthma 2014. available from http://www.nhlbi.nih.gov/health/health-topics/topics/asthma/diagnosis</ref>: | |||
*'''Medical History''' | |||
*'''Family History:''' If the patient has a family history of asthma or allergies, they are more likely to suffer from asthmatic symptoms. | |||
*'''Physical Assessment:''' The patient’s nose, throat and [[Upper Respiratory Airways|upper airways]] will be examined for signs of asthma or allergies. Assessment of the patient’s respiratory rate and breathing pattern will be carried out in conjunction with [[auscultation]] S & S including Wheezing (high-pitched whistling sounds when the patient exhales) Coughing, chest tightness, Shortness of breath (SOB), A runny nose, Swollen nasal passages.<ref>Mayo Clinic. Asthma: steps in testing and diagnosis. available from | |||
http://www.mayoclinic.org/diseases-conditions/asthma/in-depth/asthma/art-20045198 | |||
</ref>. | |||
*It is important to assess symptom control and risk of future exacerbation at every clinical visit. According to the Global Initiative for Asthma(GINA) guideline, asking just four questions relevant to the past month will give an idea of asthma control. these questions are stated in the table below: | |||
{| class="wikitable" | |||
|+ '''Routine Assessment of Asthma Patients''' | |||
!Question | |||
!Controlled | |||
!Partially Controlled | |||
!Uncontrolled | |||
|- | |||
!Have you had daytime symptoms more than twice in one week | |||
!No | |||
! rowspan="4" |one or two "yes" | |||
! rowspan="4" |Three or four "yes" | |||
|- | |||
|Have you had any night waking due to asthma | |||
|No | |||
|- | |||
|Have you needed short-acting beta-agonist (SABA), such as albuterol, rescue more than twice in one week | |||
|No | |||
|- | |||
|Have you had any activity limitations due to asthma | |||
|No | |||
|} | |||
== '''Diagnostic Tests''' == | |||
[[File:Spirometry1.jpg|right|frameless|399x399px]] | |||
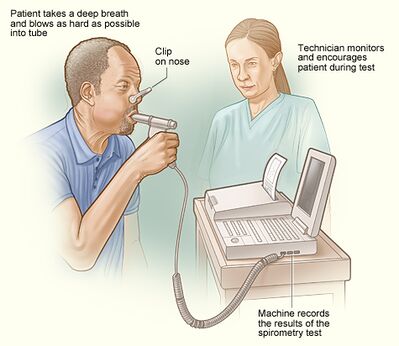
The following tests are used to assess the patient’s breathing and monitor the effectiveness of asthma treatment. | |||
[[Pulmonary Function Test|Lung function tests]]''<ref>Web MD. Diagnosing Asthma. Available from | |||
http://www.webmd.com/asthma/guide/diagnosing-asthma?page=4 | |||
</ref>'' | |||
[[Pulmonary Function Test|Spirometry,]] | |||
[http://www.lung.org/lung-health-and-diseases/lung-disease-lookup/asthma/living-with-asthma/managing-asthma/measuring-your-peak-flow-rate.html Peak flow testing] | |||
''Other tests:'' | |||
*Allergy testing | |||
*[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5617850/ Bronchoprovocation] | |||
*[[Chest X-Rays|Chest X-ray]] | |||
*[https://www.webmd.com/heart-disease/electrocardiogram-ekgs#1 Electrocardiogram (ECG)]<br> | |||
== Treatment == | |||
[[File:Kids with Asthma.jpeg|right|frameless|399x399px]] | |||
The goal of the treatment is to control the symptoms, prevent exacerbations and loss of lung function and reduce associated mortality. | |||
# Drugs used for asthma control depend on the severity of the disease. Short-acting β2-agonists can be used in patients with mild occasional symptoms. Inhaled steroids (oral steroids might be required in severe cases) and long-acting β2-agonists can be used for long-term control. Oxygen, short-acting β2-agonists, inhaled anticholinergics and systemic steroids are used in acute exacerbations. | |||
*'''Short-acting beta 2-agonists''' (quick acting or rescue medicine): these drugs are best used to treat sudden and severe or new asthma symptoms, as they dilate the airways, relieve symptoms within 20 minutes, and last four to six hours. It can also be used before physical activity about 15-20 minutes before the time to prevent exercise-induced asthma. | |||
*'''Long-acting beta 2-agonists''': these drugs are not used for quick relief of asthma symptoms, instead they are used to control symptoms and their effect lasts 12 hours. | |||
*An easy-to-follow diagram for stepped care can be assessed on page 66 of the [https://ginasthma.org/wp-content/uploads/2023/07/GINA-2023-Full-report-23_07_06-WMS.pdf GINA guideline PDF]<ref>Global Initiative for Asthma, [[Global Strategy for Asthma Management and Prevention]]. 2023. Available from: www.ginaasthma.org (Accessed 29 April 2024)</ref> | |||
2, Mechanical ventilation may be necessary for severe exacerbations that do not respond to medical treatment. Non-pharmacological measures, such as smoking cessation and avoidance of occupational sensitisers, are also important. | |||
3. Non-pharmacologic management, including asthma education on inhaler technique and self-monitoring, is vital.<ref name=":0">Anil Nanda, Alan P. Baptist, Rohit Divekar, Neil Parikh, Joram S. Seggev, Joseph S. Yusin & Sharmilee M. Nyenhuis. Asthma in the older adult, Journal of Asthma (2019); DOI: 10.1080/02770903.2019.1565828</ref> | |||
== Prognosis == | |||
Asthma is a disease with variable progression and severity of symptoms over time. The prognosis depends on the severity of the disease and the degree of control with treatment. Some patients can be symptom-free for long periods, whereas a few patients with severe persistent asthma develop progressive loss of lung function. Death due to asthma is very rare.<ref name=":2" /> | |||
Even though asthma is a reversible disorder, poor lifestyle and lack of management can lead to airway remodelling that leads to chronic symptoms, which are disabling.<ref name=":4" /> | |||
| | == Physiotherapy Management == | ||
[[File:Breathing relaxing.jpg|right|frameless]] | |||
The majority of patients suffering from asthma will seek physiotherapy for dyspnea and hyperventilation. <ref>Thomas M, Bruton A. Breathing exercises for asthma. Breathe 2014;10(4):312-322. (level of evidence 3a)</ref> Physiotherapists treat asthma in different ways to improve breathing techniques. Physiotherapy techniques for asthma are in addition to medication and should never be used as a replacement for prescribed medication, however may reduce the dosage required. | |||
'''1. Breathing Retraining Techniques''' <ref>Bott J, British Thoracic Society Physiotherapy Guideline Development Group. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. BMJ Publ. Group; 2009. (level of evidence 5)</ref> | |||
Breathing techniques may have more benefit on mild-moderate asthma <ref>Lord of Physiotherapy. Postural Drainage. Available from: http://www.youtube.com/watch?v=TPZsP1ujg0U[last accessed 08/02/13] (level of evidence 5)</ref>. The aim of breathing retraining is to normalise breathing patterns by stabilising respiratory rate and increasing expiratory airflow. Instructions are given from the physiotherapist on how to complete this technique, with the following components: | |||
*Decreasing Breaths Taken (Reducing Respiratory Rate) | |||
*Taking Smaller Breaths (Reducing Tidal Volume) | |||
*Deep Breathing (Diaphragmatic breathing through the use of abdominal muscles and lower thoracic chest movement) | |||
*Breathing through the Nose (Nasal Breathing) | |||
*Relaxation (Relaxed, controlled breathing) | |||
*Decreasing Air Leaving (Decreased expiratory flow through pursed lip breathing) | |||
*These retraining techniques help control breathing and reduce airflow turbulence, hyperinflation, variable breathing patterns and anxiety.<br> | |||
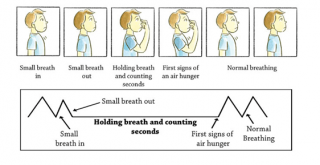
[[Image:Buteyko.png|right|320x190px]]Buteyko Breathing Technique<ref>Cowie RL, Conley DP, Underwood MF, Reader PG. A randomised controlled trial of the Buteyko technique as an adjunct to conventional management of asthma. Respir Med 2008;102(5):726-732. (level of evidence 1b)</ref> | |||
* The Buteyko breathing technique is another breathing retraining technique; however, it is specific to reducing hyperinflation. It was developed based on the theory that asthmatic bronchospasm is caused by hyperventilation, leading to a low PaCO<sub>2</sub> and therefore all asthmatic symptoms are due to this. The narrowed airways induce an “air hunger” causing a switch to mouth-breathing and an increased respiratory rate leading to hyperinflation. Buteyko believes that this hyperinflation then also contributes to bronchoconstriction. The Buteyko technique aims to reduce ventilation and subsequently [[Lung Volumes|lung volume]], as a treatment for asthma and other respiratory diseases. A qualified practitioner is necessary to train the patient <ref>Hough A. Physiotherapy in Respiratory and Cardiac Care: An Evidence-Based Approach. Nelson Thornes; 2013. (level of evidence 5)</ref>. | |||
* The Buteyko Technique<ref>http://www.buteyko.co.uk/ (level of evidence 5)</ref> | |||
**Breathe normally through the nose for 2-3 mins | |||
**Breathe out normally, close your nose with your fingers, and hold | |||
**Record number of seconds | |||
< | **On the first need to breathe, release the nose and return to nasal breathing (Control Pause) | ||
< | **Wait 3 minutes | ||
< | **Repeat and hold your breath for as long as possible (Maximum Pause)<br> | ||
[[Breathing Pattern Disorders|Breathing pattern]] retraining and relaxed breathing techniques are two approaches to physiotherapy asthma management. Breathing pattern retraining aims to develop a more efficient pattern of respiration, thereby reducing breathlessness. This is usually accomplished by slowing the breathing rate and encouraging relaxed, ‘abdominal’ breathing (Bruton, 2006). Another potential mechanism for breathing pattern retraining is that by encouraging a longer expiratory time, the effects of any static/ dynamic hyperinflation may be reduced. | |||
Mild asthmatics can hold their breath for up to twenty seconds, moderate asthmatics for fifteen seconds and severe asthmatics for up to ten seconds. This method aims to increase the control pause to 60 seconds and the maximum pause to 2 minutes. It is practised twice a day, with the practitioner there to help with breath holding and ensure safety. It aims to reduce minute volume through reduction of respiratory rate, and increasing carbon dioxide levels through breath holding, reducing bronchospasm caused by hyperventilation in the asthmatic patient. | |||
'''2. Physical Training''' | |||
* | * Physical training with asthma is advised when taking the proper precautions and should not be avoided. The American College of Sports Medicine (ACSM) Guidelines provide tips and safety precautions for asthmatics to exercise safely<ref>https://www.acsm.org/docs/current-comments/allergiesandasthmatemp.pdf (level of evidence 5)</ref>. | ||
* [[Physical Activity and Respiratory Conditions|Physical training]] should be prescribed by physiotherapists for asthmatics to increase fitness and [https://en.wikipedia.org/wiki/Cardiorespiratory_fitness cardiorespiratory performance], reduce symptoms such as breathlessness and improve quality of life <ref>Bott J, British Thoracic Society Physiotherapy Guideline Development Group. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. BMJ Publ. Group; 2009. (level of evidence 5)</ref>. Breathlessness, chest tightness and wheezing can occur when exercising, deterring patients from physical exertion <ref>Turner S, Eastwood P, Cook A, Jenkins S. Improvements in symptoms and quality of life following exercise training in older adults with moderate/severe persistent asthma. Respiration 2011;81(4):302-310. (level of evidence 1b)</ref>. Fear-avoidance can contribute to a further deterioration of physical health and quality of life, leading to anxiety and depression. It has been shown <ref>Fanelli A, Cabral ALB, Neder JA, Martins MA, Carvalho CRF. Exercise training on disease control and quality of life in asthmatic children. Med Sci Sports Exerc 2007;39(9):1474. (level of evidence 1b)</ref> that maintaining physical training in asthmatics improves disease symptoms and quality of life, making it a crucial management strategy. | |||
* A study protocol suggests behaviour change intervention focusing on increasing participation in physical activity may exert control over asthma and quality of life<ref>Freitas PD, Xavier RF, Passos NF, Carvalho-Pinto RM, Cukier A, Martins MA, Cavalheri V, Hill K, Stelmach R, Carvalho CR. [https://www.ncbi.nlm.nih.gov/pubmed/31428433 Effects of a behaviour change intervention aimed at increasing physical activity on clinical control of adults with asthma: study protocol for a randomised controlled trial]. BMC Sports Science, Medicine and Rehabilitation. 2019 Dec;11(1):1-9.</ref>. <br> | |||
'''3. Respiratory Muscle Training''' | |||
* | * Hyperinflation in asthma causes increased lung volume, leading to altered inspiratory muscle mechanics. [[Muscles of Respiration|Inspiratory muscles]] are shortened resulting in a sub-optimal length-tension relationship for contraction. There is a decreased capacity for tension generation when breathing, resulting in accessory muscles of inspiration being utilised <ref>Silva IS, Fregonezi GA, Dias FA, Ribeiro CT, Guerra RO, Ferreira GM. Inspiratory muscle training for asthma. The Cochrane Library 2013. (level of evidence 1a)</ref> | ||
* Breathing exercises are carried out using an external device to make breathing more difficult. This helps to strengthen the inspiratory muscles, making it easier to breathe in everyday life.<br>A breathing device sets up a load to breathe against. During inspiration, air is only released if enough effort is used to force open the valves of the device. [[Respiratory Muscle Training|Respiratory muscles]] are forced to work harder, increasing their strength, leading to diaphragmatic breathing becoming easier, and reducing hyperinflation. <br> | |||
* | '''4. Removal of secretions'" | ||
*[[Percussion|Percussions]] | |||
*Shaking | |||
*Vibrations, | |||
*[[Postural Drainage|Postural drainage]] and | |||
*Effective coughing | |||
A randomized crossover study<ref>Felicio-Júnior EL, Barnabé V, de Almeida FM, Avona MD, de Genaro IS, Kurdejak A, Eller MC, Verganid KP, Rodrigues JC, Tibério ID, Martins MD. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6970279/#!po=44.1176 Randomized trial of physiotherapy and hypertonic saline techniques for sputum induction in asthmatic children and adolescents.] Clinics. 2020;75.</ref> examining the ability of physiotherapy techniques in sputum induction in children and adolescent patients with Asthma suggested that specific physiotherapy manoeuvres may facilitate the collection of mucus, yielding the same amount of sputum as the gold-standard technique (hypertonic saline). The study confirms that sputum induction through physiotherapy manoeuvres is safe in well-controlled asthmatic and enables physical therapists to mobilize secretions without causing bronchospasms in patients. | |||
'''5. Range of motion exercises''' | |||
* | * Exercises for patients who need hospitalisation. | ||
* | '''6. Education''' | ||
*About condition | |||
*On the use of a bronchodilator and any other medication | |||
*How to prevent chest infection from occurring | |||
*Correct posture in standing and sitting assists in the management of asthma attacks by allowing the chest to expand appropriately and the lungs to function optimally. | |||
== Evidenced-Based Physiotherapy Management == | |||
Due to the high prevalence of asthma and associated healthcare costs, it is important to identify low-cost alternatives to traditional pharmacotherapy. One of these low-cost alternatives is the use of inspiratory muscle training (IMT), a technique aimed at increasing the strength and endurance of the diaphragm and accessory muscles of respiration. IMT typically consists of taking voluntary inspirations against a resistive load across the entire range of vital capacity while at rest. In healthy individuals, the most notable benefits of IMT are an increase in diaphragm thickness and strength, a decrease in exertional dyspnoea and the oxygen cost of breathing. IMT has been shown to decrease dyspnea, increase inspiratory muscle strength, and improve exercise capacity in asthmatic individuals.<ref>Ren-Jay Shei, Hunter L. R. Paris, Daniel P. Wilhite, Robert F. Chapman & Timothy D. Mickleborough. The role of inspiratory muscle training in the management of asthma and exercise-induced bronchoconstriction. The Physician and Sportsmedicine (2016); 44:4,327-334, </ref> | |||
Also, a systematic review by Vera et al. (2012) found that exercise can provoke asthma symptoms, such as dyspnoea, in children with asthma. Exercise-induced bronchoconstriction (EIB) is prevalent in 40–90% of children with asthma. and it was concluded physical exercise is safe and can be recommended for children with asthma. A training programme should have a minimum duration of 3 months, with at least two 60-minute training sessions per week, and a training intensity set at the (personalised) ventilatory threshold.<ref>Wanrooij VH, Willeboordse M, Dompeling E, Kim D van de Kant. Exercise training in children with asthma: a systematic review. Br J Sports Med 2014;48:1024-1031</ref> Another systematic review by Cristina et al (2018) demonstrated that aerobic physical exercise may improve nocturnal asthma in children and adults by reducing the prevalence and frequency of nocturnal symptoms.<ref>Cristina de Oliveira Francisco, Swati Anil, W. Darlene Reid, Azadeh Y. Effects of physical exercise training on nocturnal symptoms in asthma: Systematic review. PLoS One. 2018; 13(10): e0204953 | |||
</ref> A study protocol will provide the effectiveness of physiotherapy on the quality of life of children with asthma<ref>Zhang W, Liu L, Yang W, Liu H. [https://www.ncbi.nlm.nih.gov/pubmed/31261560 Effectiveness of physiotherapy on quality of life in children with asthma: Study protocol for a systematic review and meta-analysis]. Medicine. 2019 Jun;98(26).</ref>. | |||
== Other Health Professional Management == | |||
* | Asthma patients will be involved with a multidisciplinary team to manage their condition. Other health professionals treating the patient include: | ||
#Doctor | |||
#*Initial diagnosis and treatment. | |||
#Consultant | |||
#*Specialised in asthma, to help with reducing symptoms and recognising triggers. | |||
#Specialised Nurse | |||
#*To provide help, education, medication advice and general information. | |||
#Pharmacist | |||
#*Medication distribution. | |||
#Dietitian | |||
#*Advice on proper diet to not induce symptoms. | |||
#Health Psychologist | |||
#*To help with anxiety/depression associated with symptoms<br> | |||
== References == | |||
<references /> | |||
[[Category:Open_Physio]] [[Category: | [[Category:Conditions]] | ||
[[Category:Chronic Respiratory Disease]] | |||
[[Category:Cardiopulmonary]] | |||
[[Category:Open_Physio]] | |||
[[Category:Glasgow_Caledonian_University_Project]] | |||
[[Category:Chronic Respiratory Disease - Conditions]] | |||
[[Category:Non Communicable Diseases]] | |||
Latest revision as of 14:49, 29 April 2024
Original Editor - Open Physio Top Contributors - Caoimhe Mackey, Akano Oluwadara Tomisin, Kim Jackson, Chloe Hunter, Uchechukwu Chukwuemeka, Saeed Dokhnan, Rachael Lowe, Admin, Lucinda hampton, Evan Thomas, Vidya Acharya, Ayelawa Samuel, Tony Lowe, Laura Ritchie, Scott Buxton, Julie Plas, Leana Louw, Mohit Chand, Michelle Lee and WikiSysop
Introduction[edit | edit source]
Asthma is a relatively common condition characterised by at least partially reversible inflammation of the airways and reversible airway obstruction due to airway hyperreactivity. It can be acute, subacute or chronic[1] and exercise induced.
Asthma:
- Is a major noncommunicable disease (NCD) affecting children and adults.
- Affects an estimated 262 million people in 2019 and caused 461000 deaths.[1]
- Is the most common chronic disease among children.
- Symptoms can be controlled by inhaled medication and allow people with asthma to lead a normal, active life.
- Trigger avoidance can also help to reduce asthma symptoms.
- Related deaths mostly occur in low- and lower-middle-income countries, where under-diagnosis and under-treatment is a challenge.[2]
Epidemiology[edit | edit source]
Asthma is one of the most common chronic diseases in the world. It is a common pathology, affecting around 15% to 20% of people in developed countries and around 2% to 4% in less developed countries. It is significantly more common in children.[3]
Asthma:
- Affected an estimated 262 million people in 2019 and caused 461000 deaths.[2]
- May occur at any age (significantly more common in children), most patients with asthma experience their first symptoms before the age of 5 years old and about 66% are diagnosed before the age of 18 years.
- Almost 50% of children with asthma have a decrease in severity or disappearance of symptoms during early adulthood.[1]
- Prevalence is greater in extreme ages due to airway responsiveness and lower levels of lung function[3].
- In many countries, including the US, kills one out of every 100,000 persons.
- Results in millions of school and workdays lost. In the US alone, approximately 2 million asthmatics seek regular care in the emergency department, which increases healthcare costs[3].
Aetiology[edit | edit source]
Inflammation plays a major role in asthma and involves multiple cell types and mediators. The factors that initiate the inflammatory process are complex and still under investigation. Genetic factors (e.g. cytokine response profiles) and environmental exposures (such as allergens, pollution, infections, microbes, stress) at a crucial time in the development of the immune system are known to be involved.[1]
Risk Factors[edit | edit source]
- Asthma is more likely if other family members also have asthma – particularly a close relative, such as a parent or sibling.
- Asthma is more likely in people that have other allergic conditions, eczema and rhinitis (hay fever).
- Urbanisation is associated with increased asthma prevalence, probably due to multiple lifestyle factors.
- Events in early life affect the developing lungs and can increase the risk of asthma. E.g. low birth weight, prematurity, exposure to tobacco smoke and other sources of air pollution, and viral respiratory infections.
- Exposures to a range of environmental allergens and irritants are also thought to increase the risk of asthma, eg indoor and outdoor air pollution, house dust mites, moulds, and occupational exposure to chemicals, fumes, or dust.
- Children and adults who are overweight or obese are at a greater risk of asthma.
Pathophysiology[edit | edit source]
Asthma is a condition of acute, fully reversible airway inflammation, often following exposure to an environmental trigger. The pathological process begins with the inhalation of an irritant (e.g., cold air) or an allergen (e.g., pollen), which then, due to bronchial hypersensitivity, leads to airway inflammation and an increase in mucus production. This leads to a significant increase in airway resistance, which is most pronounced on expiration.
Airway obstruction occurs due to the combination of:
- Inflammatory cell infiltration.
- Mucus hypersecretion with mucus plug formation.
- Smooth muscle contraction.
These reversible changes may become irreversible over time due to
- Basement membrane thickening, collagen deposition, and epithelial desquamation.
- Airway remodelling occurs in chronic disease with smooth muscle hypertrophy and hyperplasia.
If not corrected rapidly, asthma may become more difficult to treat, as the mucus production prevents the inhaled medication from reaching the mucosa. The inflammation also becomes more edematous. This process is resolved (in theory complete resolution is required in asthma, but in practice, this is not checked or tested) with beta-2 agonists (e.g., salbutamol, salmeterol, albuterol) and can be aided by muscarinic receptor antagonists (e.g., ipratropium bromide), which act to reduce the inflammation and relax the bronchial musculature, as well as reducing mucus production.[3]
Clinical Presentation[edit | edit source]
The classic symptoms of asthma are wheezing, shortness of breath, chest tightness or difficulty breathing and cough. These symptoms are typically variable and can be absent for long periods, with possible episodic exacerbations often triggered by factors such as exercise, allergen or irritant exposure, cold air or viral respiratory infections.
The diagnosis of asthma is clinical and relies on characteristic patterns or respiratory symptoms recognition and signs in the absence of an alternative explanation. Features that increase the probability of asthma are:
- More than one of the following symptoms: wheezing, cough, difficulty breathing and chest tightness.
- Episodic symptoms that are worse at night and in the early morning, and occur in response to certain triggers, e.g. exercise, allergen exposure, cold air.
- Personal history of an atopic disorder or family history of an atopic (allergic) disorder and/or asthma
- Widespread wheeze on auscultation
- Lung function tests are useful in the evaluation of a patient with asthma to assess the presence, severity and reversibility of the airflow obstruction. On spirometry an FEV1/FEV ratio less than 0.7 confirms obstruction. In asthmatic patients, there is usually a large bronchodilator response (typically an increase of at least 12-15% in FEV1) 3, and also typically an abnormally high variability of the peak expiratory flow. A normal spirometry, particularly if performed when the patient is asymptomatic, does not exclude the diagnosis of asthma[1]
When does asthma become life threatening?
- Difficulty to catch a breath
- Difficulty talking and concentrating
- Difficulty talking and walking
- Cyanosis of skin especially around the mouth and finger areas
- Nasal flaring and constant wheeze
When these signs and symptoms present, a person should be aware and advised to consult with their general practitioner as soon as possible.
Investigations and Diagnosis[edit | edit source]
Diagnosis of asthma is confirmed based upon various factors[4]:
- Medical History
- Family History: If the patient has a family history of asthma or allergies, they are more likely to suffer from asthmatic symptoms.
- Physical Assessment: The patient’s nose, throat and upper airways will be examined for signs of asthma or allergies. Assessment of the patient’s respiratory rate and breathing pattern will be carried out in conjunction with auscultation S & S including Wheezing (high-pitched whistling sounds when the patient exhales) Coughing, chest tightness, Shortness of breath (SOB), A runny nose, Swollen nasal passages.[5].
- It is important to assess symptom control and risk of future exacerbation at every clinical visit. According to the Global Initiative for Asthma(GINA) guideline, asking just four questions relevant to the past month will give an idea of asthma control. these questions are stated in the table below:
| Question | Controlled | Partially Controlled | Uncontrolled |
|---|---|---|---|
| Have you had daytime symptoms more than twice in one week | No | one or two "yes" | Three or four "yes" |
| Have you had any night waking due to asthma | No | ||
| Have you needed short-acting beta-agonist (SABA), such as albuterol, rescue more than twice in one week | No | ||
| Have you had any activity limitations due to asthma | No |
Diagnostic Tests[edit | edit source]
The following tests are used to assess the patient’s breathing and monitor the effectiveness of asthma treatment.
Other tests:
- Allergy testing
- Bronchoprovocation
- Chest X-ray
- Electrocardiogram (ECG)
Treatment[edit | edit source]
The goal of the treatment is to control the symptoms, prevent exacerbations and loss of lung function and reduce associated mortality.
- Drugs used for asthma control depend on the severity of the disease. Short-acting β2-agonists can be used in patients with mild occasional symptoms. Inhaled steroids (oral steroids might be required in severe cases) and long-acting β2-agonists can be used for long-term control. Oxygen, short-acting β2-agonists, inhaled anticholinergics and systemic steroids are used in acute exacerbations.
- Short-acting beta 2-agonists (quick acting or rescue medicine): these drugs are best used to treat sudden and severe or new asthma symptoms, as they dilate the airways, relieve symptoms within 20 minutes, and last four to six hours. It can also be used before physical activity about 15-20 minutes before the time to prevent exercise-induced asthma.
- Long-acting beta 2-agonists: these drugs are not used for quick relief of asthma symptoms, instead they are used to control symptoms and their effect lasts 12 hours.
- An easy-to-follow diagram for stepped care can be assessed on page 66 of the GINA guideline PDF[7]
2, Mechanical ventilation may be necessary for severe exacerbations that do not respond to medical treatment. Non-pharmacological measures, such as smoking cessation and avoidance of occupational sensitisers, are also important.
3. Non-pharmacologic management, including asthma education on inhaler technique and self-monitoring, is vital.[8]
Prognosis[edit | edit source]
Asthma is a disease with variable progression and severity of symptoms over time. The prognosis depends on the severity of the disease and the degree of control with treatment. Some patients can be symptom-free for long periods, whereas a few patients with severe persistent asthma develop progressive loss of lung function. Death due to asthma is very rare.[1]
Even though asthma is a reversible disorder, poor lifestyle and lack of management can lead to airway remodelling that leads to chronic symptoms, which are disabling.[3]
Physiotherapy Management[edit | edit source]
The majority of patients suffering from asthma will seek physiotherapy for dyspnea and hyperventilation. [9] Physiotherapists treat asthma in different ways to improve breathing techniques. Physiotherapy techniques for asthma are in addition to medication and should never be used as a replacement for prescribed medication, however may reduce the dosage required.
1. Breathing Retraining Techniques [10]
Breathing techniques may have more benefit on mild-moderate asthma [11]. The aim of breathing retraining is to normalise breathing patterns by stabilising respiratory rate and increasing expiratory airflow. Instructions are given from the physiotherapist on how to complete this technique, with the following components:
- Decreasing Breaths Taken (Reducing Respiratory Rate)
- Taking Smaller Breaths (Reducing Tidal Volume)
- Deep Breathing (Diaphragmatic breathing through the use of abdominal muscles and lower thoracic chest movement)
- Breathing through the Nose (Nasal Breathing)
- Relaxation (Relaxed, controlled breathing)
- Decreasing Air Leaving (Decreased expiratory flow through pursed lip breathing)
- These retraining techniques help control breathing and reduce airflow turbulence, hyperinflation, variable breathing patterns and anxiety.
Buteyko Breathing Technique[12]
- The Buteyko breathing technique is another breathing retraining technique; however, it is specific to reducing hyperinflation. It was developed based on the theory that asthmatic bronchospasm is caused by hyperventilation, leading to a low PaCO2 and therefore all asthmatic symptoms are due to this. The narrowed airways induce an “air hunger” causing a switch to mouth-breathing and an increased respiratory rate leading to hyperinflation. Buteyko believes that this hyperinflation then also contributes to bronchoconstriction. The Buteyko technique aims to reduce ventilation and subsequently lung volume, as a treatment for asthma and other respiratory diseases. A qualified practitioner is necessary to train the patient [13].
- The Buteyko Technique[14]
- Breathe normally through the nose for 2-3 mins
- Breathe out normally, close your nose with your fingers, and hold
- Record number of seconds
- On the first need to breathe, release the nose and return to nasal breathing (Control Pause)
- Wait 3 minutes
- Repeat and hold your breath for as long as possible (Maximum Pause)
Breathing pattern retraining and relaxed breathing techniques are two approaches to physiotherapy asthma management. Breathing pattern retraining aims to develop a more efficient pattern of respiration, thereby reducing breathlessness. This is usually accomplished by slowing the breathing rate and encouraging relaxed, ‘abdominal’ breathing (Bruton, 2006). Another potential mechanism for breathing pattern retraining is that by encouraging a longer expiratory time, the effects of any static/ dynamic hyperinflation may be reduced.
Mild asthmatics can hold their breath for up to twenty seconds, moderate asthmatics for fifteen seconds and severe asthmatics for up to ten seconds. This method aims to increase the control pause to 60 seconds and the maximum pause to 2 minutes. It is practised twice a day, with the practitioner there to help with breath holding and ensure safety. It aims to reduce minute volume through reduction of respiratory rate, and increasing carbon dioxide levels through breath holding, reducing bronchospasm caused by hyperventilation in the asthmatic patient.
2. Physical Training
- Physical training with asthma is advised when taking the proper precautions and should not be avoided. The American College of Sports Medicine (ACSM) Guidelines provide tips and safety precautions for asthmatics to exercise safely[15].
- Physical training should be prescribed by physiotherapists for asthmatics to increase fitness and cardiorespiratory performance, reduce symptoms such as breathlessness and improve quality of life [16]. Breathlessness, chest tightness and wheezing can occur when exercising, deterring patients from physical exertion [17]. Fear-avoidance can contribute to a further deterioration of physical health and quality of life, leading to anxiety and depression. It has been shown [18] that maintaining physical training in asthmatics improves disease symptoms and quality of life, making it a crucial management strategy.
- A study protocol suggests behaviour change intervention focusing on increasing participation in physical activity may exert control over asthma and quality of life[19].
3. Respiratory Muscle Training
- Hyperinflation in asthma causes increased lung volume, leading to altered inspiratory muscle mechanics. Inspiratory muscles are shortened resulting in a sub-optimal length-tension relationship for contraction. There is a decreased capacity for tension generation when breathing, resulting in accessory muscles of inspiration being utilised [20]
- Breathing exercises are carried out using an external device to make breathing more difficult. This helps to strengthen the inspiratory muscles, making it easier to breathe in everyday life.
A breathing device sets up a load to breathe against. During inspiration, air is only released if enough effort is used to force open the valves of the device. Respiratory muscles are forced to work harder, increasing their strength, leading to diaphragmatic breathing becoming easier, and reducing hyperinflation.
4. Removal of secretions'"
- Percussions
- Shaking
- Vibrations,
- Postural drainage and
- Effective coughing
A randomized crossover study[21] examining the ability of physiotherapy techniques in sputum induction in children and adolescent patients with Asthma suggested that specific physiotherapy manoeuvres may facilitate the collection of mucus, yielding the same amount of sputum as the gold-standard technique (hypertonic saline). The study confirms that sputum induction through physiotherapy manoeuvres is safe in well-controlled asthmatic and enables physical therapists to mobilize secretions without causing bronchospasms in patients.
5. Range of motion exercises
- Exercises for patients who need hospitalisation.
6. Education
- About condition
- On the use of a bronchodilator and any other medication
- How to prevent chest infection from occurring
- Correct posture in standing and sitting assists in the management of asthma attacks by allowing the chest to expand appropriately and the lungs to function optimally.
Evidenced-Based Physiotherapy Management[edit | edit source]
Due to the high prevalence of asthma and associated healthcare costs, it is important to identify low-cost alternatives to traditional pharmacotherapy. One of these low-cost alternatives is the use of inspiratory muscle training (IMT), a technique aimed at increasing the strength and endurance of the diaphragm and accessory muscles of respiration. IMT typically consists of taking voluntary inspirations against a resistive load across the entire range of vital capacity while at rest. In healthy individuals, the most notable benefits of IMT are an increase in diaphragm thickness and strength, a decrease in exertional dyspnoea and the oxygen cost of breathing. IMT has been shown to decrease dyspnea, increase inspiratory muscle strength, and improve exercise capacity in asthmatic individuals.[22]
Also, a systematic review by Vera et al. (2012) found that exercise can provoke asthma symptoms, such as dyspnoea, in children with asthma. Exercise-induced bronchoconstriction (EIB) is prevalent in 40–90% of children with asthma. and it was concluded physical exercise is safe and can be recommended for children with asthma. A training programme should have a minimum duration of 3 months, with at least two 60-minute training sessions per week, and a training intensity set at the (personalised) ventilatory threshold.[23] Another systematic review by Cristina et al (2018) demonstrated that aerobic physical exercise may improve nocturnal asthma in children and adults by reducing the prevalence and frequency of nocturnal symptoms.[24] A study protocol will provide the effectiveness of physiotherapy on the quality of life of children with asthma[25].
Other Health Professional Management[edit | edit source]
Asthma patients will be involved with a multidisciplinary team to manage their condition. Other health professionals treating the patient include:
- Doctor
- Initial diagnosis and treatment.
- Consultant
- Specialised in asthma, to help with reducing symptoms and recognising triggers.
- Specialised Nurse
- To provide help, education, medication advice and general information.
- Pharmacist
- Medication distribution.
- Dietitian
- Advice on proper diet to not induce symptoms.
- Health Psychologist
- To help with anxiety/depression associated with symptoms
- To help with anxiety/depression associated with symptoms
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Radiopedia Asthma Available from:https://radiopaedia.org/articles/asthma-1 (accessed 25.5.2021)
- ↑ 2.0 2.1 WHO Asthma Available from: https://www.who.int/news-room/fact-sheets/detail/asthma(accessed 25.5.2021)
- ↑ 3.0 3.1 3.2 3.3 3.4 Hashmi MF, Tariq M, Cataletto ME, Hoover EL. Asthma 2020.Available from:https://www.ncbi.nlm.nih.gov/books/NBK430901/ (accessed 25.5.2021)
- ↑ National heart, lung and blood institute. Asthma 2014. available from http://www.nhlbi.nih.gov/health/health-topics/topics/asthma/diagnosis
- ↑ Mayo Clinic. Asthma: steps in testing and diagnosis. available from http://www.mayoclinic.org/diseases-conditions/asthma/in-depth/asthma/art-20045198
- ↑ Web MD. Diagnosing Asthma. Available from http://www.webmd.com/asthma/guide/diagnosing-asthma?page=4
- ↑ Global Initiative for Asthma, Global Strategy for Asthma Management and Prevention. 2023. Available from: www.ginaasthma.org (Accessed 29 April 2024)
- ↑ Anil Nanda, Alan P. Baptist, Rohit Divekar, Neil Parikh, Joram S. Seggev, Joseph S. Yusin & Sharmilee M. Nyenhuis. Asthma in the older adult, Journal of Asthma (2019); DOI: 10.1080/02770903.2019.1565828
- ↑ Thomas M, Bruton A. Breathing exercises for asthma. Breathe 2014;10(4):312-322. (level of evidence 3a)
- ↑ Bott J, British Thoracic Society Physiotherapy Guideline Development Group. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. BMJ Publ. Group; 2009. (level of evidence 5)
- ↑ Lord of Physiotherapy. Postural Drainage. Available from: http://www.youtube.com/watch?v=TPZsP1ujg0U[last accessed 08/02/13] (level of evidence 5)
- ↑ Cowie RL, Conley DP, Underwood MF, Reader PG. A randomised controlled trial of the Buteyko technique as an adjunct to conventional management of asthma. Respir Med 2008;102(5):726-732. (level of evidence 1b)
- ↑ Hough A. Physiotherapy in Respiratory and Cardiac Care: An Evidence-Based Approach. Nelson Thornes; 2013. (level of evidence 5)
- ↑ http://www.buteyko.co.uk/ (level of evidence 5)
- ↑ https://www.acsm.org/docs/current-comments/allergiesandasthmatemp.pdf (level of evidence 5)
- ↑ Bott J, British Thoracic Society Physiotherapy Guideline Development Group. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. BMJ Publ. Group; 2009. (level of evidence 5)
- ↑ Turner S, Eastwood P, Cook A, Jenkins S. Improvements in symptoms and quality of life following exercise training in older adults with moderate/severe persistent asthma. Respiration 2011;81(4):302-310. (level of evidence 1b)
- ↑ Fanelli A, Cabral ALB, Neder JA, Martins MA, Carvalho CRF. Exercise training on disease control and quality of life in asthmatic children. Med Sci Sports Exerc 2007;39(9):1474. (level of evidence 1b)
- ↑ Freitas PD, Xavier RF, Passos NF, Carvalho-Pinto RM, Cukier A, Martins MA, Cavalheri V, Hill K, Stelmach R, Carvalho CR. Effects of a behaviour change intervention aimed at increasing physical activity on clinical control of adults with asthma: study protocol for a randomised controlled trial. BMC Sports Science, Medicine and Rehabilitation. 2019 Dec;11(1):1-9.
- ↑ Silva IS, Fregonezi GA, Dias FA, Ribeiro CT, Guerra RO, Ferreira GM. Inspiratory muscle training for asthma. The Cochrane Library 2013. (level of evidence 1a)
- ↑ Felicio-Júnior EL, Barnabé V, de Almeida FM, Avona MD, de Genaro IS, Kurdejak A, Eller MC, Verganid KP, Rodrigues JC, Tibério ID, Martins MD. Randomized trial of physiotherapy and hypertonic saline techniques for sputum induction in asthmatic children and adolescents. Clinics. 2020;75.
- ↑ Ren-Jay Shei, Hunter L. R. Paris, Daniel P. Wilhite, Robert F. Chapman & Timothy D. Mickleborough. The role of inspiratory muscle training in the management of asthma and exercise-induced bronchoconstriction. The Physician and Sportsmedicine (2016); 44:4,327-334,
- ↑ Wanrooij VH, Willeboordse M, Dompeling E, Kim D van de Kant. Exercise training in children with asthma: a systematic review. Br J Sports Med 2014;48:1024-1031
- ↑ Cristina de Oliveira Francisco, Swati Anil, W. Darlene Reid, Azadeh Y. Effects of physical exercise training on nocturnal symptoms in asthma: Systematic review. PLoS One. 2018; 13(10): e0204953
- ↑ Zhang W, Liu L, Yang W, Liu H. Effectiveness of physiotherapy on quality of life in children with asthma: Study protocol for a systematic review and meta-analysis. Medicine. 2019 Jun;98(26).