Shoulder Instability: Difference between revisions
No edit summary |
No edit summary |
||
| (43 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Johanna Guim|Johanna Guim]] and [[User:Katherine Burdeaux|Katherine Burdeaux]] as part of the [[Temple University Evidence-Based Practice Project]] | '''Original Editor '''- [[User:Johanna Guim|Johanna Guim]] and [[User:Katherine Burdeaux|Katherine Burdeaux]] as part of the [[Temple University Evidence-Based Practice Project]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | |||
== Introduction == | |||
[[File:Shoulder diagram.jpg|thumb|436x436px|Shoulder Diagram]] | [[File:Shoulder diagram.jpg|thumb|436x436px|Shoulder Diagram]] | ||
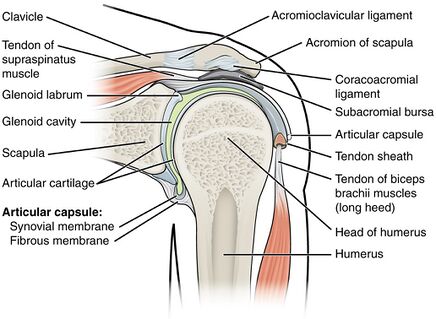
The [[Glenohumeral Joint|glenohumeral joint]] of the shoulder has the highest [[Range of Motion|range of motion]] of the human body and the most inherently unstable, often developing recurrent instability<ref name=":0" />. | The [[Glenohumeral Joint|glenohumeral joint]] of the shoulder has the highest [[Range of Motion|range of motion]] of the human body and the most inherently unstable, often developing recurrent instability<ref name=":0" />. | ||
Shoulder instability is defined as loss of shoulder comfort and function due to undesirable translation of humeral head on the glenoid fossa.<ref name=":2">Nicolozakes CP, Li X, Uhl TL, Marra G, Jain NB, Perreault EJ, Seitz AL. Interprofessional inconsistencies in the diagnosis of shoulder instability: Survey results of physicians and rehabilitation providers. International Journal of Sports Physical Therapy. 2021;16(4):1115.</ref> | |||
The ligamentous and muscle structures(static and dynamic stabilizers) around the glenohumeral joint, in normal conditions, create a balanced net joint reaction force. If the integrity of any of these structures is disrupted it can lead to spectrum of pathologies from subluxation to dislocation.<ref>Hayes K, Callanan M, Walton J, Paxinos A, Murrell GA. Shoulder instability: management and rehabilitation. Journal of Orthopaedic & Sports Physical Therapy. 2002 Oct;32(10):497-509.</ref> | |||
Both structural and nonstructural components can contribute to the instability of the shoulder. | |||
==Classification of Shoulder Instability== | |||
=== [[Stanmore Classification of Shoulder Instability|Stanmore Triangle]]<ref>Jaggi A, Alexander S. Suppl-6, M13: Rehabilitation for Shoulder Instability–Current Approaches. The open orthopaedics journal. 2017;11:957.</ref> === | |||
This classification helps the therapist to correctly diagnose the instability and prioritize the treatment. | |||
There are three main subgroups in this classification: | |||
Polar 1: Shoulder instability is directly related to trauma. There is evidence of a structural deficit in the GH joint | |||
Polar 2: There is evidence of structural deficit and atraumatic instability | |||
Polar 3: No evidence of structural defects. Muscle patterning is present. | |||
=== Based on the direction of shoulder instability<ref name=":1">Brukner P, Khan K. Clinical Sports Medicine, revised 5th edition.</ref> === | |||
==== Anterior Instability ==== | |||
There occurs translation of the humeral head in the anterior. direction It is the most common form of shoulder instability.<ref name=":2" /> | |||
==== Posterior Instability ==== | |||
It accounts for 2 to 5 % of instability cases. Usually, the athletic population is affected by this type of instability who participate in an overhead activity.<ref>Goldenberg BT, Goldsten P, Lacheta L, Arner JW, Provencher MT, Millett PJ. Rehabilitation Following Posterior Shoulder Stabilization. International Journal of Sports Physical Therapy. 2021;16(3):930.</ref> Structural issues like posterior glenoid erosion and glenoid retroversion or deficiency of rotator interval can predispose patients to posterior instability. | |||
==== Multidirectional instability (Atraumatic) ==== | |||
There is a combination of anterior /posterior/inferior instability at the GH joint. In many cases, this type of instability is because of generalized laxity throughout the body. Another cause is repetitive trauma during extremes of motion. | |||
Mainly the pain is during the mid ranges of shoulder ROM which indicates main role of altered muscle activation. Inappropriate position of the scapula can also be the reason for pain or any other symptoms. | |||
=== Traumatic Unidirectional Instability with Bankart lesion (TUBS)<ref name=":1" /> === | |||
==== Anterior Dislocation ==== | |||
This is the commonest sports injury in which acute anterior dislocation of GH joint occurs. The arm is forced into excessive abduction and external rotation. It damages the anterior part of the labrum (Bankart lesion). | |||
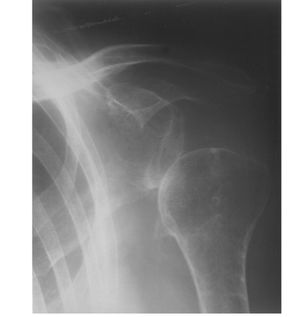
= | The patient presentation is arm adduction and internally rotated with loss of deltoid contour. Posterior sulcus/glenohumeral void is observed. The humeral head is palpated anteriorly. Radiographs are used to confirm the diagnosis and rule out other bone injuries.<ref name=":2" /> | ||
=== | |||
One of the three following criteria has to be fulfilled in order to prescribe the Xray : | |||
Age>40, first time dislocation, traumatic mechanism of injury. | |||
==== Posterior Dislocation ==== | |||
It is less common than an anterior dislocation. The cause is a fall on the outstretched hand or a direct blow on the shoulder in internal rotation of adduction. The Cardinal sign is limited external rotation. An X-ray of lateral view or axillary view is necessary for diagnosis. | |||
=== Acquired sport-specific instability === | |||
This type is commonly seen in overhead athletes when the anterior capsule has become lax due to overuse. This is also known as an acquired instability overuse syndrome. Clinical features are recurrent shoulder pain while throwing, sudden inability to throw or smash and a feels like 'dead arm', GIRD /scapular dyskinesia /signs of labral pathology are also seen. | |||
Apprehension /relocation tests are positive. | |||
This condition can turn into impingement due to abnormal translation of humeral head. | |||
=== Atraumatic === | === Atraumatic === | ||
Abnormal position or motion of the shoulder joint that leads to pain, subluxation, dislocation and functional impairment. | |||
Atraumatic (non-traumatic) shoulder instability is a subclassification of glenohumeral joint instability, encompassing those for whom trauma is not considered the primary etiology. <ref>Barrett C. The Clinical Physiotherapy Assessment of Non-Traumatic Shoulder Instability. Shoulder & Elbow. 2015 Jan;7(1):60-71.</ref> | Atraumatic (non-traumatic) shoulder instability is a subclassification of glenohumeral joint instability, encompassing those for whom trauma is not considered the primary etiology. <ref>Barrett C. The Clinical Physiotherapy Assessment of Non-Traumatic Shoulder Instability. Shoulder & Elbow. 2015 Jan;7(1):60-71.</ref> | ||
| Line 28: | Line 75: | ||
[[Image:Shoulder Joint Hayes.png|border|right|1px|Illustration adapted from Hayes]] | [[Image:Shoulder Joint Hayes.png|border|right|1px|Illustration adapted from Hayes]] | ||
== Shoulder Instability Video == | |||
This 5 minute video is on shoulder instability and clicking {{#ev:youtube|H8TyXqVMwds}} | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
Glenohumeral stability depends on the combination of various factors that can be grouped into: | Glenohumeral stability depends on the combination of various factors that can be grouped into: | ||
| Line 34: | Line 83: | ||
# Musculotendinous or dynamic stabilizers: | # Musculotendinous or dynamic stabilizers: | ||
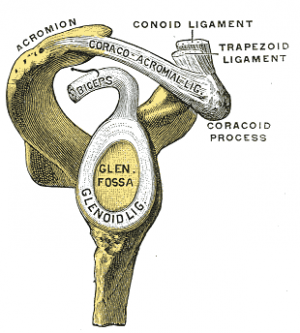
===Static Stabilisers=== | ===1. Static Stabilisers=== | ||
[[File:AC ligs.png|thumb|Glenoid fossa, on R side]] | [[File:AC ligs.png|thumb|Glenoid fossa, on R side]] | ||
The static capsulo-ligamentary elements, are considered to be the main stabilizers of the glenohumeral joint<ref name=":0">Cuéllar R, Ruiz-Ibán MA, Cuéllar A. Suppl-6, M10: [https://benthamopen.com/ABSTRACT/TOORTHJ-11-919 Anatomy and Biomechanics of the Unstable Shoulder]. The open orthopaedics journal. 2017;11:919.</ref> Note - The 3 glenohumeral ligaments are thickenings of the glenohumeral joint capsule.<ref>Radiopedia [https://radiopaedia.org/articles/glenohumeral-ligaments?lang=us Glenohumeral ligaments] Available:https://radiopaedia.org/articles/glenohumeral-ligaments?lang=us (accessed 27.1.2022)</ref> | The static capsulo-ligamentary elements, are considered to be the main stabilizers of the glenohumeral joint<ref name=":0">Cuéllar R, Ruiz-Ibán MA, Cuéllar A. Suppl-6, M10: [https://benthamopen.com/ABSTRACT/TOORTHJ-11-919 Anatomy and Biomechanics of the Unstable Shoulder]. The open orthopaedics journal. 2017;11:919.</ref> Note - The 3 glenohumeral ligaments are thickenings of the glenohumeral joint capsule.<ref>Radiopedia [https://radiopaedia.org/articles/glenohumeral-ligaments?lang=us Glenohumeral ligaments] Available:https://radiopaedia.org/articles/glenohumeral-ligaments?lang=us (accessed 27.1.2022)</ref> | ||
| Line 47: | Line 96: | ||
* Cuellar<ref name=":0" /><ref name=":0" />suggests that shoulder instability can be due to injury and/or failure of the static capsulo-ligamentary stabilizing elements (which are supporting the sensitive afferent ending). | * Cuellar<ref name=":0" /><ref name=":0" />suggests that shoulder instability can be due to injury and/or failure of the static capsulo-ligamentary stabilizing elements (which are supporting the sensitive afferent ending). | ||
* This alteration of the passive stabilizing elements causes a disturbance or delay in the delivery of the proprioceptive signal, delaying or causes errors in [[Coordination Exercises|coordination]] of the muscles response. The dynamic stabilizing mechanism is thus altered and the loss of joint congruity is facilitated. | * This alteration of the passive stabilizing elements causes a disturbance or delay in the delivery of the proprioceptive signal, delaying or causes errors in [[Coordination Exercises|coordination]] of the muscles response. The dynamic stabilizing mechanism is thus altered and the loss of joint congruity is facilitated. | ||
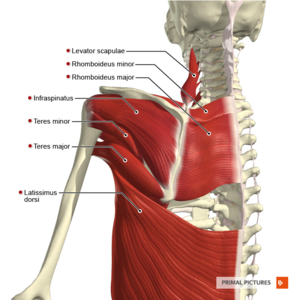
===2. Dynamic Stabilisers=== | |||
===Dynamic Stabilisers=== | |||
[[File:Muscles of the scapular region posterior aspect Primal.png|thumb|Muscles: scapular region posterior]] | [[File:Muscles of the scapular region posterior aspect Primal.png|thumb|Muscles: scapular region posterior]] | ||
Assist with holding the humeral head in the glenoid fossa during movement <ref name="Guerrero" /> | Assist with holding the humeral head in the glenoid fossa during movement <ref name="Guerrero" /> | ||
| Line 63: | Line 109: | ||
* [[Pectoralis major]] | * [[Pectoralis major]] | ||
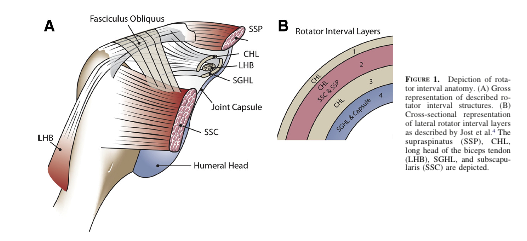
'''3. Rotator Cuff Interval''' | '''3. Rotator Cuff Interval''' | ||
[[File:Rotator cuff interval.jpeg|thumb|Rotator cuff interval]] | |||
This interval is a triangular-shaped area found in the shoulder, with borders noted below. A large rotator interval allows for increased anterior humeral head translation due to the lack of structures supporting the joint capsule anteriorly.<ref name="Guerrero" /> | This interval is a triangular-shaped area found in the shoulder, with borders noted below. A large rotator interval allows for increased anterior humeral head translation due to the lack of structures supporting the joint capsule anteriorly.<ref name="Guerrero" /> | ||
* '''Superior border:''' anterior margin of supraspinatus | * '''Superior border:''' anterior margin of supraspinatus | ||
| Line 69: | Line 115: | ||
* '''Apex:''' transverse humeral ligament | * '''Apex:''' transverse humeral ligament | ||
* '''Base:''' coracoid process of [[Scapula|scapular]] | * '''Base:''' coracoid process of [[Scapula|scapular]] | ||
[[File:RCI.png|frameless|527x527px]]<br>Potential structures involved in shoulder instability are listed in table below. | [[File:RCI.png|frameless|527x527px]]<br>'''Potential structures involved in shoulder instability are listed in table below.''' | ||
{| class="wikitable sortable" width="100%" align="center" border="1" cellspacing="1" cellpadding="1" | {| class="wikitable sortable" width="100%" align="center" border="1" cellspacing="1" cellpadding="1" | ||
|+ | |+ | ||
| Line 101: | Line 147: | ||
| <br> | | <br> | ||
|} | |} | ||
== Mechanism of Injury == | == Mechanism of Injury == | ||
[[File:Glenohumeral Subluxation .jpg|thumb|GH joint anterior dislocation]] | [[File:Glenohumeral Subluxation .jpg|thumb|GH joint anterior dislocation]] | ||
===Traumatic=== | ===1. Traumatic=== | ||
The most common [[Shoulder Dislocation|glenohumeral dislocation]] occurs anteriorly, usually as a result of sporting accidents or [[falls]], particularly when the upper extremity is in 90° abduction and external rotation. | The most common [[Shoulder Dislocation|glenohumeral dislocation]] occurs anteriorly, usually as a result of sporting accidents or [[falls]], particularly when the upper extremity is in 90° abduction and external rotation. | ||
Posterior dislocations most commonly result from seizures, [[shock]] and falls. | Posterior dislocations most commonly result from seizures, [[shock]] and falls. | ||
===Atraumatic=== | ===2. Atraumatic=== | ||
==== Chronic Recurrent ==== | |||
==== '''Chronic Recurrent''' ==== | |||
[[File:Tennis serve.jpeg|thumb|Abducted, extended shoulder - Tennis serve]] | [[File:Tennis serve.jpeg|thumb|Abducted, extended shoulder - Tennis serve]] | ||
Caused by repetitive extreme external rotation with the [[humerus]] abducted and extended (i.e.pitching motion).<ref name="Guerrero" /> Instability may be caused by gradual weakening of the anterior and inferior static restraints. The humeral head will tend to move away from shortened structures. For example: posterior shoulder capsular tightness will cause the humeral head to shift anteriorly, resulting in a loss of integrity of all anterior structures. Commonly associated with participation in sports such as gymnastics, baseball, softball, tennis, swimming, and weight training.<ref name="Guerrero" /> | Caused by repetitive extreme external rotation with the [[humerus]] abducted and extended (i.e.pitching motion).<ref name="Guerrero" /> Instability may be caused by gradual weakening of the anterior and inferior static restraints. The humeral head will tend to move away from shortened structures. For example: posterior shoulder capsular tightness will cause the humeral head to shift anteriorly, resulting in a loss of integrity of all anterior structures. Commonly associated with participation in sports such as gymnastics, baseball, softball, tennis, swimming, and weight training.<ref name="Guerrero" /> | ||
| Line 134: | Line 169: | ||
* ALPSA lesion (Anterior Labroligamentous Periosteal Sleeve Avulsion) | * ALPSA lesion (Anterior Labroligamentous Periosteal Sleeve Avulsion) | ||
* Laxity of the joint capsule | * Laxity of the joint capsule | ||
[[File:Glenoid-dysplasia-1.jpeg|thumb|309x309px|Right shoulder pain after repetitive shoulder posterior dislocation.]] | |||
==== Congenital Instability | ==== Congenital Instability ==== | ||
Congenital instability may be the result of: | Congenital instability may be the result of: | ||
* | * Glenoid hypoplasia, also known as glenoid dysplasia, is an uncommon congenital condition resulting from underdevelopment of inferior glenoid ossification centre<ref>Gilcrease-Garcia, B., Hacking, C. Glenoid hypoplasia. Reference article, Radiopaedia.org. Available: https://radiopaedia.org/articles/glenoid-hypoplasia?lang=gb<nowiki/>(accessed on 27 Jan 2022)</ref>. | ||
* Decrease anterior-posterior diameter of glenoid | * Decrease anterior-posterior diameter of glenoid | ||
* Increased retroversion of glenoid | * Increased retroversion of glenoid | ||
* Increased amount and composition of [[collagen]] and elastin | * Increased amount and composition of [[collagen]] and elastin | ||
* Bony anomalies | * Bony anomalies <ref name="Guerrero" /> | ||
== Clinical Presentation == | == Clinical Presentation == | ||
Possible signs and symptoms of chronic/recurrent instability | Possible signs and symptoms of chronic/recurrent instability | ||
[[Anterior Shoulder Instability|Anterior Instability]] | |||
* Clicking | * Clicking | ||
* Pain | * Pain | ||
* Complain of dead arm with throwing | * Complain of the dead arm with throwing | ||
* Pain posteriorly | * Pain posteriorly | ||
* Possible subacromial or internal impingement signs | * Possible subacromial or internal impingement signs | ||
* The patient may have a positive apprehension test, relocation test, and/or anterior release test | * The patient may have a positive apprehension test, relocation test, and/or anterior release test | ||
* Increased joint accessory motion particularly in the anterior direction | * Increased joint accessory motion particularly in the anterior direction | ||
[https://www.physio-pedia.com/Posterior_Shoulder_Instability Posterior Instability] | |||
* Possible subacromial or [[Internal Impingement of the Shoulder|internal impingement]] | * Possible subacromial or [[Internal Impingement of the Shoulder|internal impingement]] | ||
* Glenohumeral internal rotation deficit (GIRD) may be present | * Glenohumeral internal rotation deficit (GIRD) may be present | ||
| Line 161: | Line 196: | ||
* Clicking | * Clicking | ||
* Increased joint accessory motion particularly in the posterior direction | * Increased joint accessory motion particularly in the posterior direction | ||
Multidirectional Instability | |||
* Antero-inferior laxity most commonly presents with global shoulder pain, cannot pinpoint to a specific location | * Antero-inferior laxity most commonly presents with global shoulder pain, cannot pinpoint to a specific location | ||
* May have a positive sulcus sign, [[Apprehension Test|apprehension/relocation test]], anterior release tests | * May have a positive sulcus sign, [[Apprehension Test|apprehension/relocation test]], anterior release tests | ||
* Secondary rotator cuff impingement can be seen with microtraumatic events caused during participation in sports such as gymnastics, swimming and weight training<ref name="Guerrero" /> | * Secondary rotator cuff impingement can be seen with microtraumatic events caused during participation in sports such as gymnastics, swimming and weight training<ref name="Guerrero" /> | ||
* Increased joint accessory motion in multiple planes | * Increased joint accessory motion in multiple planes | ||
== Red flags == | |||
* Trauma, pain and weakness (indicates rotator cuff tear) | |||
* Swelling/mass (Indicates tumor/malignancy) | |||
* Fever or any systemic illness | |||
* Unreduced dislocation | |||
* Infected joint<ref>Noorani A, Goldring M, Jaggi A, Gibson J, Rees J, Bateman M, Falworth M, Brownson P. BESS/BOA patient care pathways: atraumatic shoulder instability. Shoulder & elbow. 2019 Feb;11(1):60-70.</ref> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 180: | Line 222: | ||
===Subjective History=== | ===Subjective History=== | ||
Global pain around shoulder<ref name="Guerrero" /> | * May have history of: trauma with or without a previous dislocation; lax joints (consider elbow, knee, thumb hyperextension<ref name="Guerrero" />, use [https://www.physio-pedia.com/Beighton_score Beighton scale] to evaluate hypermobility) | ||
* [[Activities of Daily Living|Activities of daily living]] may be difficult to complete | |||
* Global pain around shoulder<ref name="Guerrero" /> | |||
===Physical Examination=== | ===Physical Examination=== | ||
Screen cervical spine and thoracic spine | Screen [[Cervical Anatomy|cervical spine]] and [[Thoracic Anatomy|thoracic spine]] | ||
'''Observation/Palpation''' | '''Observation/Palpation''' | ||
* Long head of biceps, supraspinatus tendon, AC joint, SC joint, spine, 1st rib, other regional muscles | * Long head of biceps, supraspinatus tendon, AC joint, SC joint, spine, [[Ribs|1st rib]], other regional muscles | ||
'''Posture'''<ref name="Jaggi">Jaggi A. Rehabilitation for shoulder instability. Br J Sports Med 2010;44(5):333.</ref> | '''Posture'''<ref name="Jaggi">Jaggi A. Rehabilitation for shoulder instability. Br J Sports Med 2010;44(5):333.</ref> | ||
* Asymmetry | * Asymmetry | ||
* Scapular winging | * [[Winged scapula|Scapular winging]] | ||
* Atrophy | * Atrophy | ||
'''Active ROM''' | '''Active ROM''' | ||
| Line 201: | Line 240: | ||
* Look for apprehensive behavior | * Look for apprehensive behavior | ||
'''Passive ROM''' | '''Passive ROM''' | ||
* May have pain | * May have pain and/or stiffness | ||
* Apprehension will be present | |||
* | |||
'''Muscle Length Testing''' | '''Muscle Length Testing''' | ||
* Upper trapezius, levator scapulae, scalenes, latissimus dorsi, lower trapezius, pectoralis minor, pectoralis major | * Upper trapezius, levator scapulae, scalenes, latissimus dorsi, lower trapezius, pectoralis minor, pectoralis major | ||
| Line 219: | Line 257: | ||
'''Special Tests''' | '''Special Tests''' | ||
* Possibly sulcus sign, apprehension/relocation and/or anterior release tests depending on suspected form of instability | * Possibly sulcus sign, apprehension/relocation and/or anterior release tests depending on suspected form of instability. See special tests below. | ||
== Special Tests == | == Special Tests == | ||
| Line 251: | Line 289: | ||
|- | |- | ||
| Apprehension<ref name="Lo">Lo IK, Nonweiler B, Woolfrey M, Litchfield R, Kirkley A. An evaluation of the apprehension, relocation, and surprise tests for anterior shoulder instability. Am J Sports Med.2004;32:301-7</ref> | | Apprehension<ref name="Lo">Lo IK, Nonweiler B, Woolfrey M, Litchfield R, Kirkley A. An evaluation of the apprehension, relocation, and surprise tests for anterior shoulder instability. Am J Sports Med.2004;32:301-7</ref> | ||
| 0.53 | | 0.53 | ||
| 0.99 | | 0.99 | ||
| Line 263: | Line 302: | ||
|} | |} | ||
== Laxity Tests == | |||
<u rel="mw:ExtLink" href="http://www.physio-pedia.com/index.php5?title=Load_and_Shift">1. [https://www.physio-pedia.com/Load_and_Shift Load and Shift Test]</u> | |||
'''Application:''' The patient lies on their back with the scapula on the table but the caput free. Load the caput humerus into the glenoid and then translate the caput in the anterior and posterior directions. | |||
'''Application:''' | |||
The | '''Conclusion:''' The test aims to evaluate the amount of translation of the caput humerus on the glenoid. There are many methodes to grade the test but the most common one is the Hawkins grading. This method is considered to be the best one because it has a clinical basis. Hawkins divided the movement in four grades: Grade 0 = little to no movement; grade 1 = the humeral head rises up onto the glenoid rim; grade 2 = when the caput humerus can be dislocate but relocate spontaneously; grade 3 = when the head does not relocate after the pressure. '''Clinical Bottom Line:'''Tzannes and Murell <ref name="Tzannes et al. 2004">Tzannes A, Murrel, GAC. An assessment of the interexaminar reliability of tests for shoulder instability. The journal of Shoulder and Elbow Surgery 2004; 13:18-23.</ref> have concluded that this test is entirely reliable (p<0,0001) and a LR > 80 for instability. | ||
2. Drawer Test | |||
The | '''Application:''' The patient is positioned supine. The examiner holds the patients scapula with his left hand while grasping the patient’s upper arm and drawing the humeral anterior head with his right hand. You can hold the shoulder in a different position. | ||
'''Clinical Bottom Line:''' | '''Conclusion:''' The test tells you more about the laxity. The test is positive when the thumb was felt to slide past the coracoid. '''Clinical Bottom Line:''' Tzannes and Murell <ref name="Tzannes et al. 2002">Tzannes A, Murell GAC. Clinical examination of the unstable shoulder. Sports Medicine 2002; 32: 447-457.</ref> have concluded that this test is still to be assessed as to its validity and reliability. | ||
3. <u>[https://www.physio-pedia.com/Inferior_Sulcus_Test Sulcus Sign]</u> | |||
'''Application:''' The patient’s elbow is pulled inferiorly while the patient is relaxed | |||
'''Application:''' | |||
The | '''Conclusion:''' This manoeuvre tests the superior glenohumeral ligament. The test is positive when there is a sulcus of more than 2 cm between the acromion and caput humerus. '''Clinical Bottom Line:''' Tzannes and Murell<ref>Tzannes et al. 2004</ref> also evaluate this test as being completely reliable (p<0,0001). Nakagawa et al report a specificity of 0.93. | ||
== Provocative Tests == | |||
'''1. Anterior Release Test''' | |||
''' | '''Application:''' In this test, the examiner applies posteriorly directed force to the humeral head, with the patient being in abduction and external rotation. | ||
The test | '''Conclusion:''' The test is positive in case of pain or apprehension when easing the pressure. '''Clinical Bottom Line:''' In the light of the results of Tzannes and Murell <ref>Tzannes et al. 2002</ref>(p<0,0001) and Ian et al <ref name="Ian et al.">Ian KY, Lo IKY, Nonweiler B, et al. An evaluation of the apprehension, relocation, and surprise test for anterior shoulder instability. American Journal of Sports Medicine 2004; 32:301-307.</ref> we can conclude that it is a reliable test for the detection of the unstable shoulder. Gross et al report a sensitivity of 0.92 and a specificity of 0.89, making this test useful to rule out shoulder instability with a negative result. | ||
<u>[https://www.physio-pedia.com/Apprehension_Test Apprehension/Augmentation Test]</u> | |||
'''Application:''' The apprehension test is being applied when the patient is lying or sitting with the shoulder in a neutral position (90° abduction). The examiner holds the patient’s wrist with one hand and with the other hand he applies anteriorly directed force to the humeral head. | |||
= | '''Conclusion:''' Signs of glenohumeral anterior instability are: pain, a feeling of subluxation or clear defence. If a relocation test is being applied almost immediately after the apprehension test and if this relocation test results to be negative, than we can decide that there is anterior instability. '''Clinical Bottom Line:''' Based on the results of Levy et al. <ref name="Levy et al.">Levy AS, Lintner S, Kenter K, et al: intra- and interobserver reproducibility of the shoulder laxity examination. The American Journal of Sports medicine 1999; 4: 460-463.</ref>; Ian et al. <ref>Ian et al.</ref> (sensitivity = 53 & specificity = 99), Tzannes and Murell <ref>Tzannes A, Murrel, GAC. An assessment of the interexaminar reliability of tests for shoulder instability. The journal of Shoulder and Elbow Surgery 2004; 13:18-23.</ref> (p= 0,0004 pain and/or apprehension and a LR 8-100 for anterior instability) and Marx et al.<ref name="Marx et al.">Marx RG, Bombardier C, Wright JG. What do we know about the reliability and validity of physical examination tests used to examine the upper extremity? Journal of Hand Surgery 1999; 24A:185-193.</ref>, we are able to conclude that there is not sufficient clinical proof to detect or exclude instability. Lo et al report a specificity of 0.99. | ||
<u>[https://www.physio-pedia.com/Jobes_Relocation_Test Relocation Test]</u> | |||
'''Application:''' The patient is in the starting position of the apprehension test and the examiner now applies posteriorly directed force to the humeral head. | |||
'''Clinical Bottom Line:''' | '''Conclusion:''' When this test results to be negative, there is glenohumeral anterior instability. '''Clinical Bottom Line:''' The article by Ian et al. <ref>Ian et al.</ref> (sensitivity = 45 & specificity = 54) states that the relocation test is not clinically evident. However, other articles by Tzannes and Murell<ref>Tzannes et al. 2004</ref> (p= 0,0003 pain and/or apprehension) and Liu et al.<ref name="Liu et al.">Liu SH, Henry MH, Nuccion S, et al. Diagnosis of glenoid labral tears. A comparison between magnetic resonance imaging and clinical examinations. The American Journal of Sports Medicine 1996; 2:149-154.</ref> provide evidence to the contrary. Lo et al report poor psychometric properties on this test. | ||
== Outcome Measures == | |||
* [https://www.physio-pedia.com/DASH_Outcome_Measure Disabilities of Shoulder, Arm, and Hand (DASH)] | |||
* Quick DASH | |||
* [https://www.physio-pedia.com/Visual_Analogue_Scale Visual Analogue Scale] | |||
* [[Shoulder Pain and Disability Index (SPADI)|Shoulder Pain And Disability Index]]<ref>Breckenridge JD, McAuley JH. Shoulder pain and disability index (SPADI). Journal of physiotherapy. 2011 Jan 1;57(3):197-.</ref> | |||
Diagnosis specific questionnaires<ref name="Rouleau">Rouleau D, Faber K, MacDermin J. Systematic review of patient-administered shoulder functional scores on instability. J Shoulder Elbow Surg. 2010;19:1121-1128.</ref> | |||
* Western Ontario Shoulder Instability Index | |||
* Oxford Shoulder Instability Questionnaire | |||
* Melbourne Instability Shoulder Scale | |||
== Medical Management == | |||
=== | Medical management will hinge on the specifics of the patient presentation including the mechanism of injury, severity, patient goals, etc. In some cases, particularly those with a traumatic mechanism, surgical intervention may be warranted to restore joint stability. <br> <br>Types of surgical procedures for traumatic glenohumeral dislocations<ref name="Guerrero" /> | ||
# Open capsular shift | |||
# Arthroscopic thermal capsulorraphy | |||
# Labral repair | |||
== Physical Therapy Management == | |||
[[File:Wall squat with stability ball.jpg|thumb]] | |||
Non-operative physical therapy management will vary in a case-by-case situation and each patient’s care should be individualised to target their specific [[Goal Setting in Rehabilitation|goals]]. Physical therapy management is largely impairment-based and response-driven as there is little high-level evidence to assist decision making but commonly includes: | |||
* Education to prevent recurrence | |||
* [[Posture|Postural r]]<nowiki/>e-education | |||
* [[Motor Control Changes and Pain|Motor control]] training of specific muscles during functional activities (rotator cuff muscles, scapular stabilisers) | |||
* [[Strength Training|Strengthening]] in particular the deltoid, rotator cuff muscles and scapular stabilisers | |||
* [[Stretching]] in particular posterior shoulder structures, pectoralis major and minor and any other muscles with [[flexibility]] impairments | |||
[[Manual Therapy|Manual therapy]] targeting impairments of mobility in the glenohumeral, [[Acromioclavicular Joint|acromioclavicular]], [[Sternoclavicular Joint|sternoclavicular]] joints and cervico-thoracic spine <ref name="Mintken">Mintken. Some Factors Predict Successful Short-Term Outcomes in IndividualsWith Shoulder Pain Receiving Cervicothoracic Manipulation: A Single-Arm Trial. PTJ 2010;26-42.</ref> | |||
==== < | == Exercise Therapy Findings == | ||
''' | [[File:Overhead retractions.png|thumb]] | ||
A 2020 study to assess the efficacy and safety of physical therapist–supervised, shoulder instability neuromuscular exercise (SINEX) versus self-managed, home-based, standard care shoulder exercise (HOMEX) in patients with traumatic primary and recurrent anterior shoulder dislocations ASDs, concluded "Neuromuscular shoulder exercise (SINEX) was superior to HOMEX in patients with traumatic ASDs. SINEX Program was focused on neuromuscular exercises with movement quality feedback by supervision from physical therapists. The neuromuscular program included strength, coordination, balance, and proprioception exercises. Treatment was a 12 weeks program, individually tailored and supervised, progressing shoulder exercise and functional kinetic chain exercises. It included 7 exercises targeting the glenohumeral and scapular muscles, with 7 progression levels (basic to elite). Exercises followed general strength training principles, with basic and elite levels referring to low and high load exercises<ref>Eshoj, H.R., Rasmussen, S., Frich, L.H., Hvass, I., Christensen, R., Boyle, E., Jensen, S.L., Søndergaard, J., Søgaard, K. and Juul-Kristensen, B., 2020. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6993151/ Neuromuscular exercises improve shoulder function more than standard care exercises in patients with a traumatic anterior shoulder dislocation: a randomized controlled trial.] ''Orthopaedic journal of sports medicine'', ''8''(1), p.2325967119896102. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6993151/<nowiki/>(accessed 28.1.2022)</ref>. | |||
A 2018 study "The effects of a conservative rehabilitation program for multidirectional instability (MDI) of the shoulder" evaluated the effectiveness of a physiotherapy-led exercise program for participants with MDI. The rehabilitation program focused on regaining stability and control of muscles acting on the glenohumeral joint and scapulothoracic joints and gradually progressing the shoulder into functional positions and activities. The program, which has been published in detail, required participants to attend rehabilitation once weekly for 12 weeks. The results "identified improvement in functional status, shoulder muscle strength, and scapular positioning after rehabilitation" highlighting the value of conservative management of MDI. <ref name="WATSON, Lyn, et al.">WATSON, Lyn, et al. [https://www.sciencedirect.com/science/article/abs/pii/S1058274617304238 The effects of a conservative rehabilitation program for multidirectional instability of the shoulder.] Journal of shoulder and elbow surgery, 2018, 27.1: 104-111. Available:https://www.sciencedirect.com/science/article/abs/pii/S1058274617304238 (accessed 28.1.2022) </ref> | |||
Exercise therapy after Bankart and reverse Bankart. | |||
Following surgery, a shoulder immobilizer was worn for 3 weeks. | |||
Isometric exercise in the sling was started at 1 day postoperatively. Increasing range of motion exercises were prescribed for 2 weeks after surgery. | |||
* The shoulder immobilizer was removed, and active flexion exercise in the supine position and passive external rotation exercise were started at 3 weeks postoperatively. | |||
* Rotator cuff exercise was started using a rubber band at 4 weeks postoperatively, and unlimited activities of daily living were allowed at 6 weeks postoperatively. | |||
* Upper limb muscle training was permitted using a <2kg dumbbell at 2 months, and push-ups were permitted at 3 months. | |||
* Noncontact sports were permitted at 2 to 3 months, and contact sports and overhead throwing were permitted at 6 months. | |||
Posterior shoulder instability is divided dimensionally: unidirectionally (posterior), bidirectionally (posteroinferior), and multidirectionally (posterior, inferior, and anterior). Bidirectional and multidirectional instability being the most common. Multidirectional instability may have an inciting traumatic event, but it is due to preexisting global capsular laxity. Conservative physiotherapy management is the primary option for treatment. If conservative treatment is unsuccessful after a 6-month course, surgery may be considered. | |||
* For the first month, the shoulder should be kept in relative external or neutral rotation to relax the posterior capsule and antevert itself. | |||
* Between the first and second months’ postsurgery, passive and active assisted range of motion can begin in a protected fashion while still limiting end ranges of motion in positions that maximally stress the posterior capsule. | |||
* The sling use may be discontinued around 6 weeks. | |||
* Between 2 and 5 months, strengthening can begin with isometrics for the rotator cuff and periscapular muscles. | |||
* Full motion should be achieved between 2 and 3 months. | |||
* Between months 5 and 8, patients may begin gradual return to previous sports, activities, and work duties but under controlled conditions. | |||
* Full return depends on full functional range of motion, no pain or tenderness, good strength, and satisfactory clinical examination..<ref name="TANNENBAUM, Eric; SEKIYA, Jon K.">TANNENBAUM, Eric; SEKIYA, Jon K. Evaluation and management of posterior shoulder instability. Sports Health, 2011, 3.3: 253-263. </ref> | |||
''' | '''''<br>'''''<b>Post-Op Physical Therapy Management</b> | ||
Depends on: | |||
* Surgical procedure | |||
* Surgeon’s protocol | |||
* Mechanism of injury | |||
* Concomitant injuries | |||
* Tissue quality | |||
* Impairments noted at evaluation | |||
This 4 minutes video gives some examples of exercises for shoulder instability.{{#ev:youtube|5PH5SuL51wI}} | |||
== Rehabilitation Of Posterior Shoulder stabilization<ref name=":3">Goldenberg BT, Goldsten P, Lacheta L, Arner JW, Provencher MT, Millett PJ. Rehabilitation Following Posterior Shoulder Stabilization. International Journal of Sports Physical Therapy. 2021;16(3):930.</ref> == | |||
* Posterior shoulder stabilization is done in the patients of posterior shoulder instability who failed conservative management. | |||
=== | === Phase One - Protection Phase === | ||
==== Goals ==== | |||
To reduce pain, edema, restore the movement of accessory joint and educate the patient. | |||
==== Rehabilitation ==== | |||
===== Postoperative Day 1 to Day 15. Protection Phase. ===== | |||
''' | * The first visit of physiotherapy includes history taking, assessing the postoperative status, and establish functional goals. | ||
* Surgical findings such as the procedure, postoperative restrictions, rehabilitation protocol, and prognosis are reviewed. | |||
* The plan of care is prepared by the physiotherapist along with the inputs from the surgeon. | |||
* The limb is immobilized with a sling and abduction pillow placing the limb in the scaption plane. | |||
* Cryotherapy is to be applied five to six times a day to reduce pain , spasm, and edema. | |||
* Active range of motion is applied on other joints of the body and postural education is provided. | |||
* Usually, passive range of motion is initiated after 2 weeks with prior permission from the surgeon. | |||
* '''PROM''' is limited to '''120 degrees of flexion,''' '''90 degrees of abduction''', '''internal rotation''' '''till the abdomen''', and '''external rotation till 30 degrees'''. | |||
* Isometrics of rotator cuff and scapulothoracic muscles to improve the dynamic joint stability. | |||
* Isometrics can be prescribed as home program and the patient can use wall as the resistance. Submaximal amount of force is used in the initial sessions. | |||
===== Criteria to progress to AROM and muscle endurance(phase 2) ===== | |||
* PROM mentioned above has to be fulfilled inorder to ensure proper stability of GH joint. | |||
* Patient should be able to perform scapular clock exercise while using minimal substitution. Clock exercise includes protraction, retraction, elevation and depression of scapula. | |||
* Pain level has to be 3/10. | |||
* The score of Quick DASH score has to be less than 60%. | |||
===== Postoperative phase TWO (Active Motion and Endurance Phase) (Day 16 to Day 44) ===== | |||
* The '''goal''' of this phase is to achieve AROM and improve the strength of rotator cuff and periscapular muscles. | |||
* Active assisted range of motion exercises are started initially with progression to Active ROM exercises. | |||
* At first, the active-assisted ROM is done in a supine or prone lying position to minimize the effect of gravity then progressed to sitting position followed by standing as per the tolerance of the patient. | |||
* Active assisted ROM is done by using normal extremity or lightweight wooden dowel within the surgical restrictions. | |||
* For more function involvement, standing forward flexion with support can be started. This can be prescribed as a home exercise program and the patient can do it with dowel or ski pole and progress it in multiple planes. | |||
* | |||
* | |||
* | |||
===== Active Range Of Motion Exercises( After 6 weeks) ===== | |||
* This is initiated when the patient can perform isometrics and AAROM exercises with minimum compensatory movements and minimal pain. | |||
* The sling is removed. | |||
* It is commenced in supine position and progressed to standing as the firing of the muscles is improved. | |||
It is important to activate the RC properly as it enhances the dynamic stability of the shoulder and prevents impingement by restricting abnormal superior translation of humeral head. | |||
===== Criteria for progression to Initial resistance strengthening ===== | |||
Pain <3/10 during active ROM | |||
== | |||
Quick DASH score <40% | |||
AROM : Flexion 120degrees, Abduction 120degrees, External Rotation 45 degrees | |||
Posses normal scapula movements | |||
'''Ability to perform the following motions at least for 20 repetitions without fatigue''': | |||
* Elevation up to 90 degrees in scaption plane | |||
* Abduction upto 90 degrees | |||
* Side-lying external rotation to zero degrees | |||
===== Criteria for progression to advanced strengthening<ref name=":3" /> ===== | |||
Quick DASH <20% | |||
AROM of flexion, abduction and external rotation > 90% as compared to contralateral side. | |||
>80%on hand held dynamometer in all the planes of the shoulder joint. | |||
<br /> | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Shoulder instability may have a traumatic or atraumatic cause. There is a high recurrence rate after a primary shoulder dislocation, which is greatest in individuals < 20 years old. Rehabilitation should be based on each individual patient’s case with consideration to the type of surgery and surgeon’s preference where surgery is undertaken. | Shoulder instability may have a traumatic or atraumatic cause. There is a high recurrence rate after a primary shoulder dislocation, which is greatest in individuals < 20 years old. Rehabilitation should be based on each individual patient’s case with consideration to the type of surgery and surgeon’s preference where surgery is undertaken. | ||
| Line 414: | Line 495: | ||
[[Category:Sports Injuries]] | [[Category:Sports Injuries]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category: | [[Category:Plus Content]] | ||
Latest revision as of 18:19, 17 January 2023
Original Editor - Johanna Guim and Katherine Burdeaux as part of the Temple University Evidence-Based Practice Project Top Contributors - Katherine Burdeaux, Nupur Smit Shah, Lucinda hampton, Admin, Rachael Lowe, Kim Jackson, Naomi O'Reilly, Johnathan Fahrner, Birgit Schauvliege, Vandoorne Ben, Fasuba Ayobami, Simisola Ajeyalemi, Johanna Guim, WikiSysop, Uchechukwu Chukwuemeka, Joao Costa, Rucha Gadgil, Wanda van Niekerk, Aminat Abolade and Scott A Burns
Introduction[edit | edit source]
The glenohumeral joint of the shoulder has the highest range of motion of the human body and the most inherently unstable, often developing recurrent instability[1].
Shoulder instability is defined as loss of shoulder comfort and function due to undesirable translation of humeral head on the glenoid fossa.[2]
The ligamentous and muscle structures(static and dynamic stabilizers) around the glenohumeral joint, in normal conditions, create a balanced net joint reaction force. If the integrity of any of these structures is disrupted it can lead to spectrum of pathologies from subluxation to dislocation.[3]
Both structural and nonstructural components can contribute to the instability of the shoulder.
Classification of Shoulder Instability[edit | edit source]
Stanmore Triangle[4][edit | edit source]
This classification helps the therapist to correctly diagnose the instability and prioritize the treatment.
There are three main subgroups in this classification:
Polar 1: Shoulder instability is directly related to trauma. There is evidence of a structural deficit in the GH joint
Polar 2: There is evidence of structural deficit and atraumatic instability
Polar 3: No evidence of structural defects. Muscle patterning is present.
Based on the direction of shoulder instability[5][edit | edit source]
Anterior Instability[edit | edit source]
There occurs translation of the humeral head in the anterior. direction It is the most common form of shoulder instability.[2]
Posterior Instability[edit | edit source]
It accounts for 2 to 5 % of instability cases. Usually, the athletic population is affected by this type of instability who participate in an overhead activity.[6] Structural issues like posterior glenoid erosion and glenoid retroversion or deficiency of rotator interval can predispose patients to posterior instability.
Multidirectional instability (Atraumatic)[edit | edit source]
There is a combination of anterior /posterior/inferior instability at the GH joint. In many cases, this type of instability is because of generalized laxity throughout the body. Another cause is repetitive trauma during extremes of motion.
Mainly the pain is during the mid ranges of shoulder ROM which indicates main role of altered muscle activation. Inappropriate position of the scapula can also be the reason for pain or any other symptoms.
Traumatic Unidirectional Instability with Bankart lesion (TUBS)[5][edit | edit source]
Anterior Dislocation[edit | edit source]
This is the commonest sports injury in which acute anterior dislocation of GH joint occurs. The arm is forced into excessive abduction and external rotation. It damages the anterior part of the labrum (Bankart lesion).
The patient presentation is arm adduction and internally rotated with loss of deltoid contour. Posterior sulcus/glenohumeral void is observed. The humeral head is palpated anteriorly. Radiographs are used to confirm the diagnosis and rule out other bone injuries.[2]
One of the three following criteria has to be fulfilled in order to prescribe the Xray :
Age>40, first time dislocation, traumatic mechanism of injury.
Posterior Dislocation[edit | edit source]
It is less common than an anterior dislocation. The cause is a fall on the outstretched hand or a direct blow on the shoulder in internal rotation of adduction. The Cardinal sign is limited external rotation. An X-ray of lateral view or axillary view is necessary for diagnosis.
Acquired sport-specific instability[edit | edit source]
This type is commonly seen in overhead athletes when the anterior capsule has become lax due to overuse. This is also known as an acquired instability overuse syndrome. Clinical features are recurrent shoulder pain while throwing, sudden inability to throw or smash and a feels like 'dead arm', GIRD /scapular dyskinesia /signs of labral pathology are also seen.
Apprehension /relocation tests are positive.
This condition can turn into impingement due to abnormal translation of humeral head.
Atraumatic[edit | edit source]
Abnormal position or motion of the shoulder joint that leads to pain, subluxation, dislocation and functional impairment.
Atraumatic (non-traumatic) shoulder instability is a subclassification of glenohumeral joint instability, encompassing those for whom trauma is not considered the primary etiology. [7]
Two main types of atraumatic instabilities:
- Congenital instabilities;
- Laxity of structures in the shoulder which may be present since birth.[8]
- Chronic recurrent instabilities
- May be seen after surgery for shoulder dislocation, due to glenoid rim lesions.[9]
- Over time, microtrauma can lead to instability of the glenohumeral joint.
Shoulder Instability Video[edit | edit source]
This 5 minute video is on shoulder instability and clicking
Clinically Relevant Anatomy [edit | edit source]
Glenohumeral stability depends on the combination of various factors that can be grouped into:
- Capsulo-ligamentary or static stabilizers
- Musculotendinous or dynamic stabilizers:
1. Static Stabilisers[edit | edit source]
The static capsulo-ligamentary elements, are considered to be the main stabilizers of the glenohumeral joint[1] Note - The 3 glenohumeral ligaments are thickenings of the glenohumeral joint capsule.[10]
- Superior glenohumeral ligament (SGHL) [11] - limits anterior and inferior translation of adducted humerus
- Medial glenohumeral ligament (MGHL) - limits anterior translation in lower and middle range of abduction
- Inferior glenohumeral ligament (IGHL) - longest glenohumeral ligament and primary static restraint against anterior, posterior and inferior translation when humerus is abducted beyond 45 degrees
- Glenoid labrum - increases depth of glenoid cavity and increases stability up to 50% [8]
- Negative intra-articular pressure [11] - assists in maximizing joint congruency
The proprioception mechanisms of the shoulder joint have been investigated and found to be closely related to the response of the dynamic muscle stabilisers.
- Various histological studies in anatomical specimens have confirmed the presence of afferent nerve endings (Ruffini corpuscles and Pacini mechanoreceptors, sensory receptors that responds to mechanical changes of tissues) and they are distributed in the shoulder capsuloligamentary complex.[1]
- Cuellar[1][1]suggests that shoulder instability can be due to injury and/or failure of the static capsulo-ligamentary stabilizing elements (which are supporting the sensitive afferent ending).
- This alteration of the passive stabilizing elements causes a disturbance or delay in the delivery of the proprioceptive signal, delaying or causes errors in coordination of the muscles response. The dynamic stabilizing mechanism is thus altered and the loss of joint congruity is facilitated.
2. Dynamic Stabilisers[edit | edit source]
Assist with holding the humeral head in the glenoid fossa during movement [8]
1. Primary
- Rotator cuff muscles (supraspinatus,infraspinatus, teres minor, subscapularis)
- Long head of biceps
- Deltoid
2. Secondary
3. Rotator Cuff Interval
This interval is a triangular-shaped area found in the shoulder, with borders noted below. A large rotator interval allows for increased anterior humeral head translation due to the lack of structures supporting the joint capsule anteriorly.[8]
- Superior border: anterior margin of supraspinatus
- Inferior border: subscapularis
- Apex: transverse humeral ligament
- Base: coracoid process of scapular
Potential structures involved in shoulder instability are listed in table below.
| Anterior | Posterior | Multidirectional |
| SGHL,MGHL, Anterior IGHL | SGHL, Posterior IGHL | Dysfunction of dynamic stabilisers |
| Anterior capsule | Posterior capsule | Joint capsule in 2 or more directions. Inferior capsule is primarily affected. |
| Coracohumeral ligament | Coracohumeral ligament | All structures involved in anterior or posterior instability can be affected |
| Superior anterior labrum | ||
| Long head of biceps | ||
| Subscapularis |
Mechanism of Injury[edit | edit source]
1. Traumatic[edit | edit source]
The most common glenohumeral dislocation occurs anteriorly, usually as a result of sporting accidents or falls, particularly when the upper extremity is in 90° abduction and external rotation.
Posterior dislocations most commonly result from seizures, shock and falls.
2. Atraumatic[edit | edit source]
Chronic Recurrent[edit | edit source]
Caused by repetitive extreme external rotation with the humerus abducted and extended (i.e.pitching motion).[8] Instability may be caused by gradual weakening of the anterior and inferior static restraints. The humeral head will tend to move away from shortened structures. For example: posterior shoulder capsular tightness will cause the humeral head to shift anteriorly, resulting in a loss of integrity of all anterior structures. Commonly associated with participation in sports such as gymnastics, baseball, softball, tennis, swimming, and weight training.[8]
Common concomitant features or causes:
- Bankart lesion
- HillSachs lesion
- SLAP lesion (Superior Labrum Anterior Posterior)
- HAGL lesion (Humeral Avulsion of Glenohumeral Ligaments)
- ALPSA lesion (Anterior Labroligamentous Periosteal Sleeve Avulsion)
- Laxity of the joint capsule
Congenital Instability [edit | edit source]
Congenital instability may be the result of:
- Glenoid hypoplasia, also known as glenoid dysplasia, is an uncommon congenital condition resulting from underdevelopment of inferior glenoid ossification centre[12].
- Decrease anterior-posterior diameter of glenoid
- Increased retroversion of glenoid
- Increased amount and composition of collagen and elastin
- Bony anomalies [8]
Clinical Presentation [edit | edit source]
Possible signs and symptoms of chronic/recurrent instability
- Clicking
- Pain
- Complain of the dead arm with throwing
- Pain posteriorly
- Possible subacromial or internal impingement signs
- The patient may have a positive apprehension test, relocation test, and/or anterior release test
- Increased joint accessory motion particularly in the anterior direction
- Possible subacromial or internal impingement
- Glenohumeral internal rotation deficit (GIRD) may be present
- Pain
- Clicking
- Increased joint accessory motion particularly in the posterior direction
Multidirectional Instability
- Antero-inferior laxity most commonly presents with global shoulder pain, cannot pinpoint to a specific location
- May have a positive sulcus sign, apprehension/relocation test, anterior release tests
- Secondary rotator cuff impingement can be seen with microtraumatic events caused during participation in sports such as gymnastics, swimming and weight training[8]
- Increased joint accessory motion in multiple planes
Red flags[edit | edit source]
- Trauma, pain and weakness (indicates rotator cuff tear)
- Swelling/mass (Indicates tumor/malignancy)
- Fever or any systemic illness
- Unreduced dislocation
- Infected joint[13]
Differential Diagnosis[edit | edit source]
- Rotator Cuff Tear
- Subacromial Impingement
- Internal Impingement
- Cervical Spine Mechanical Pain (referring to shoulder)
- Biceps Tendinopathy
- Labral Pathology
- Laxity due to Congenital Causes (ie: Ehlers-Danlos Syndrome)
Examination [edit | edit source]
Subjective History[edit | edit source]
- May have history of: trauma with or without a previous dislocation; lax joints (consider elbow, knee, thumb hyperextension[8], use Beighton scale to evaluate hypermobility)
- Activities of daily living may be difficult to complete
- Global pain around shoulder[8]
Physical Examination[edit | edit source]
Screen cervical spine and thoracic spine
Observation/Palpation
- Long head of biceps, supraspinatus tendon, AC joint, SC joint, spine, 1st rib, other regional muscles
Posture[14]
- Asymmetry
- Scapular winging
- Atrophy
Active ROM
- Glenohumeral flexion, extension, abduction, adduction, rotation - internal & external, scaption
- Look for apprehensive behavior
Passive ROM
- May have pain and/or stiffness
- Apprehension will be present
Muscle Length Testing
- Upper trapezius, levator scapulae, scalenes, latissimus dorsi, lower trapezius, pectoralis minor, pectoralis major
Resistive Testing
Functional Testing[15]
- Hand to posterior neck
- Hand to scapula
- Hand to opposite scapula
Joint Accessory Motion Testing
- Increased mobility in the direction of the instability (anterior, posterior, multidirectional)
Scapular/Thoracic Motion[8]
Proprioception
Special Tests
- Possibly sulcus sign, apprehension/relocation and/or anterior release tests depending on suspected form of instability. See special tests below.
Special Tests[edit | edit source]
Provocative tests and laxity examinations may be used to confirm a hypothesis of shoulder instability:
| Test | Sensitivity | Specificity | + LR | -LR |
| Sulcus |
0.17 |
0.93 | 2.43 | 0.89 |
|
Anterior Release Test[16] |
0.92 | 0.89 | 8.36 | 0.09 |
| Apprehension[17] | 0.53 | 0.99 | 53 | 0.47 |
| Relocation[17] | 0.46 | 0.54 | 1 | 1 |
Laxity Tests[edit | edit source]
Application: The patient lies on their back with the scapula on the table but the caput free. Load the caput humerus into the glenoid and then translate the caput in the anterior and posterior directions.
Conclusion: The test aims to evaluate the amount of translation of the caput humerus on the glenoid. There are many methodes to grade the test but the most common one is the Hawkins grading. This method is considered to be the best one because it has a clinical basis. Hawkins divided the movement in four grades: Grade 0 = little to no movement; grade 1 = the humeral head rises up onto the glenoid rim; grade 2 = when the caput humerus can be dislocate but relocate spontaneously; grade 3 = when the head does not relocate after the pressure. Clinical Bottom Line:Tzannes and Murell [18] have concluded that this test is entirely reliable (p<0,0001) and a LR > 80 for instability.
2. Drawer Test
Application: The patient is positioned supine. The examiner holds the patients scapula with his left hand while grasping the patient’s upper arm and drawing the humeral anterior head with his right hand. You can hold the shoulder in a different position.
Conclusion: The test tells you more about the laxity. The test is positive when the thumb was felt to slide past the coracoid. Clinical Bottom Line: Tzannes and Murell [19] have concluded that this test is still to be assessed as to its validity and reliability.
3. Sulcus Sign
Application: The patient’s elbow is pulled inferiorly while the patient is relaxed
Conclusion: This manoeuvre tests the superior glenohumeral ligament. The test is positive when there is a sulcus of more than 2 cm between the acromion and caput humerus. Clinical Bottom Line: Tzannes and Murell[20] also evaluate this test as being completely reliable (p<0,0001). Nakagawa et al report a specificity of 0.93.
Provocative Tests [edit | edit source]
1. Anterior Release Test
Application: In this test, the examiner applies posteriorly directed force to the humeral head, with the patient being in abduction and external rotation.
Conclusion: The test is positive in case of pain or apprehension when easing the pressure. Clinical Bottom Line: In the light of the results of Tzannes and Murell [21](p<0,0001) and Ian et al [22] we can conclude that it is a reliable test for the detection of the unstable shoulder. Gross et al report a sensitivity of 0.92 and a specificity of 0.89, making this test useful to rule out shoulder instability with a negative result.
Apprehension/Augmentation Test
Application: The apprehension test is being applied when the patient is lying or sitting with the shoulder in a neutral position (90° abduction). The examiner holds the patient’s wrist with one hand and with the other hand he applies anteriorly directed force to the humeral head.
Conclusion: Signs of glenohumeral anterior instability are: pain, a feeling of subluxation or clear defence. If a relocation test is being applied almost immediately after the apprehension test and if this relocation test results to be negative, than we can decide that there is anterior instability. Clinical Bottom Line: Based on the results of Levy et al. [23]; Ian et al. [24] (sensitivity = 53 & specificity = 99), Tzannes and Murell [25] (p= 0,0004 pain and/or apprehension and a LR 8-100 for anterior instability) and Marx et al.[26], we are able to conclude that there is not sufficient clinical proof to detect or exclude instability. Lo et al report a specificity of 0.99.
Application: The patient is in the starting position of the apprehension test and the examiner now applies posteriorly directed force to the humeral head.
Conclusion: When this test results to be negative, there is glenohumeral anterior instability. Clinical Bottom Line: The article by Ian et al. [27] (sensitivity = 45 & specificity = 54) states that the relocation test is not clinically evident. However, other articles by Tzannes and Murell[28] (p= 0,0003 pain and/or apprehension) and Liu et al.[29] provide evidence to the contrary. Lo et al report poor psychometric properties on this test.
Outcome Measures[edit | edit source]
- Disabilities of Shoulder, Arm, and Hand (DASH)
- Quick DASH
- Visual Analogue Scale
- Shoulder Pain And Disability Index[30]
Diagnosis specific questionnaires[31]
- Western Ontario Shoulder Instability Index
- Oxford Shoulder Instability Questionnaire
- Melbourne Instability Shoulder Scale
Medical Management [edit | edit source]
Medical management will hinge on the specifics of the patient presentation including the mechanism of injury, severity, patient goals, etc. In some cases, particularly those with a traumatic mechanism, surgical intervention may be warranted to restore joint stability.
Types of surgical procedures for traumatic glenohumeral dislocations[8]
- Open capsular shift
- Arthroscopic thermal capsulorraphy
- Labral repair
Physical Therapy Management [edit | edit source]
Non-operative physical therapy management will vary in a case-by-case situation and each patient’s care should be individualised to target their specific goals. Physical therapy management is largely impairment-based and response-driven as there is little high-level evidence to assist decision making but commonly includes:
- Education to prevent recurrence
- Postural re-education
- Motor control training of specific muscles during functional activities (rotator cuff muscles, scapular stabilisers)
- Strengthening in particular the deltoid, rotator cuff muscles and scapular stabilisers
- Stretching in particular posterior shoulder structures, pectoralis major and minor and any other muscles with flexibility impairments
Manual therapy targeting impairments of mobility in the glenohumeral, acromioclavicular, sternoclavicular joints and cervico-thoracic spine [32]
Exercise Therapy Findings[edit | edit source]
A 2020 study to assess the efficacy and safety of physical therapist–supervised, shoulder instability neuromuscular exercise (SINEX) versus self-managed, home-based, standard care shoulder exercise (HOMEX) in patients with traumatic primary and recurrent anterior shoulder dislocations ASDs, concluded "Neuromuscular shoulder exercise (SINEX) was superior to HOMEX in patients with traumatic ASDs. SINEX Program was focused on neuromuscular exercises with movement quality feedback by supervision from physical therapists. The neuromuscular program included strength, coordination, balance, and proprioception exercises. Treatment was a 12 weeks program, individually tailored and supervised, progressing shoulder exercise and functional kinetic chain exercises. It included 7 exercises targeting the glenohumeral and scapular muscles, with 7 progression levels (basic to elite). Exercises followed general strength training principles, with basic and elite levels referring to low and high load exercises[33].
A 2018 study "The effects of a conservative rehabilitation program for multidirectional instability (MDI) of the shoulder" evaluated the effectiveness of a physiotherapy-led exercise program for participants with MDI. The rehabilitation program focused on regaining stability and control of muscles acting on the glenohumeral joint and scapulothoracic joints and gradually progressing the shoulder into functional positions and activities. The program, which has been published in detail, required participants to attend rehabilitation once weekly for 12 weeks. The results "identified improvement in functional status, shoulder muscle strength, and scapular positioning after rehabilitation" highlighting the value of conservative management of MDI. [34]
Exercise therapy after Bankart and reverse Bankart.
Following surgery, a shoulder immobilizer was worn for 3 weeks.
Isometric exercise in the sling was started at 1 day postoperatively. Increasing range of motion exercises were prescribed for 2 weeks after surgery.
- The shoulder immobilizer was removed, and active flexion exercise in the supine position and passive external rotation exercise were started at 3 weeks postoperatively.
- Rotator cuff exercise was started using a rubber band at 4 weeks postoperatively, and unlimited activities of daily living were allowed at 6 weeks postoperatively.
- Upper limb muscle training was permitted using a <2kg dumbbell at 2 months, and push-ups were permitted at 3 months.
- Noncontact sports were permitted at 2 to 3 months, and contact sports and overhead throwing were permitted at 6 months.
Posterior shoulder instability is divided dimensionally: unidirectionally (posterior), bidirectionally (posteroinferior), and multidirectionally (posterior, inferior, and anterior). Bidirectional and multidirectional instability being the most common. Multidirectional instability may have an inciting traumatic event, but it is due to preexisting global capsular laxity. Conservative physiotherapy management is the primary option for treatment. If conservative treatment is unsuccessful after a 6-month course, surgery may be considered.
- For the first month, the shoulder should be kept in relative external or neutral rotation to relax the posterior capsule and antevert itself.
- Between the first and second months’ postsurgery, passive and active assisted range of motion can begin in a protected fashion while still limiting end ranges of motion in positions that maximally stress the posterior capsule.
- The sling use may be discontinued around 6 weeks.
- Between 2 and 5 months, strengthening can begin with isometrics for the rotator cuff and periscapular muscles.
- Full motion should be achieved between 2 and 3 months.
- Between months 5 and 8, patients may begin gradual return to previous sports, activities, and work duties but under controlled conditions.
- Full return depends on full functional range of motion, no pain or tenderness, good strength, and satisfactory clinical examination..[35]
Post-Op Physical Therapy Management
Depends on:
- Surgical procedure
- Surgeon’s protocol
- Mechanism of injury
- Concomitant injuries
- Tissue quality
- Impairments noted at evaluation
This 4 minutes video gives some examples of exercises for shoulder instability.
Rehabilitation Of Posterior Shoulder stabilization[36][edit | edit source]
- Posterior shoulder stabilization is done in the patients of posterior shoulder instability who failed conservative management.
Phase One - Protection Phase[edit | edit source]
Goals[edit | edit source]
To reduce pain, edema, restore the movement of accessory joint and educate the patient.
Rehabilitation[edit | edit source]
Postoperative Day 1 to Day 15. Protection Phase.[edit | edit source]
- The first visit of physiotherapy includes history taking, assessing the postoperative status, and establish functional goals.
- Surgical findings such as the procedure, postoperative restrictions, rehabilitation protocol, and prognosis are reviewed.
- The plan of care is prepared by the physiotherapist along with the inputs from the surgeon.
- The limb is immobilized with a sling and abduction pillow placing the limb in the scaption plane.
- Cryotherapy is to be applied five to six times a day to reduce pain , spasm, and edema.
- Active range of motion is applied on other joints of the body and postural education is provided.
- Usually, passive range of motion is initiated after 2 weeks with prior permission from the surgeon.
- PROM is limited to 120 degrees of flexion, 90 degrees of abduction, internal rotation till the abdomen, and external rotation till 30 degrees.
- Isometrics of rotator cuff and scapulothoracic muscles to improve the dynamic joint stability.
- Isometrics can be prescribed as home program and the patient can use wall as the resistance. Submaximal amount of force is used in the initial sessions.
Criteria to progress to AROM and muscle endurance(phase 2)[edit | edit source]
- PROM mentioned above has to be fulfilled inorder to ensure proper stability of GH joint.
- Patient should be able to perform scapular clock exercise while using minimal substitution. Clock exercise includes protraction, retraction, elevation and depression of scapula.
- Pain level has to be 3/10.
- The score of Quick DASH score has to be less than 60%.
Postoperative phase TWO (Active Motion and Endurance Phase) (Day 16 to Day 44)[edit | edit source]
- The goal of this phase is to achieve AROM and improve the strength of rotator cuff and periscapular muscles.
- Active assisted range of motion exercises are started initially with progression to Active ROM exercises.
- At first, the active-assisted ROM is done in a supine or prone lying position to minimize the effect of gravity then progressed to sitting position followed by standing as per the tolerance of the patient.
- Active assisted ROM is done by using normal extremity or lightweight wooden dowel within the surgical restrictions.
- For more function involvement, standing forward flexion with support can be started. This can be prescribed as a home exercise program and the patient can do it with dowel or ski pole and progress it in multiple planes.
Active Range Of Motion Exercises( After 6 weeks)[edit | edit source]
- This is initiated when the patient can perform isometrics and AAROM exercises with minimum compensatory movements and minimal pain.
- The sling is removed.
- It is commenced in supine position and progressed to standing as the firing of the muscles is improved.
It is important to activate the RC properly as it enhances the dynamic stability of the shoulder and prevents impingement by restricting abnormal superior translation of humeral head.
Criteria for progression to Initial resistance strengthening[edit | edit source]
Pain <3/10 during active ROM
Quick DASH score <40%
AROM : Flexion 120degrees, Abduction 120degrees, External Rotation 45 degrees
Posses normal scapula movements
Ability to perform the following motions at least for 20 repetitions without fatigue:
- Elevation up to 90 degrees in scaption plane
- Abduction upto 90 degrees
- Side-lying external rotation to zero degrees
Criteria for progression to advanced strengthening[36][edit | edit source]
Quick DASH <20%
AROM of flexion, abduction and external rotation > 90% as compared to contralateral side.
>80%on hand held dynamometer in all the planes of the shoulder joint.
Clinical Bottom Line[edit | edit source]
Shoulder instability may have a traumatic or atraumatic cause. There is a high recurrence rate after a primary shoulder dislocation, which is greatest in individuals < 20 years old. Rehabilitation should be based on each individual patient’s case with consideration to the type of surgery and surgeon’s preference where surgery is undertaken.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Cuéllar R, Ruiz-Ibán MA, Cuéllar A. Suppl-6, M10: Anatomy and Biomechanics of the Unstable Shoulder. The open orthopaedics journal. 2017;11:919.
- ↑ 2.0 2.1 2.2 Nicolozakes CP, Li X, Uhl TL, Marra G, Jain NB, Perreault EJ, Seitz AL. Interprofessional inconsistencies in the diagnosis of shoulder instability: Survey results of physicians and rehabilitation providers. International Journal of Sports Physical Therapy. 2021;16(4):1115.
- ↑ Hayes K, Callanan M, Walton J, Paxinos A, Murrell GA. Shoulder instability: management and rehabilitation. Journal of Orthopaedic & Sports Physical Therapy. 2002 Oct;32(10):497-509.
- ↑ Jaggi A, Alexander S. Suppl-6, M13: Rehabilitation for Shoulder Instability–Current Approaches. The open orthopaedics journal. 2017;11:957.
- ↑ 5.0 5.1 Brukner P, Khan K. Clinical Sports Medicine, revised 5th edition.
- ↑ Goldenberg BT, Goldsten P, Lacheta L, Arner JW, Provencher MT, Millett PJ. Rehabilitation Following Posterior Shoulder Stabilization. International Journal of Sports Physical Therapy. 2021;16(3):930.
- ↑ Barrett C. The Clinical Physiotherapy Assessment of Non-Traumatic Shoulder Instability. Shoulder & Elbow. 2015 Jan;7(1):60-71.
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 Guerrero P, Busconi B, Deangelis N, Powers G. Congenital instability of the shoulder joint: assessment and treatment options. JOSPT. 2009;39(2):124-134.
- ↑ Charousset C, Beauthler V, Bellaïche, Guillin R, Brassart N, Thomazeau H. Can we improve radiological analysis of osseous lesions in chronic anterior shoulder instability? Orthop. Traumatol. Surg. Res. 2010;96:88-93.
- ↑ Radiopedia Glenohumeral ligaments Available:https://radiopaedia.org/articles/glenohumeral-ligaments?lang=us (accessed 27.1.2022)
- ↑ 11.0 11.1 Hayes K, Callanan M, Walton J. Shoulder instability: Management and rehabilitation. JOSPT 2002;23(10):497-509.
- ↑ Gilcrease-Garcia, B., Hacking, C. Glenoid hypoplasia. Reference article, Radiopaedia.org. Available: https://radiopaedia.org/articles/glenoid-hypoplasia?lang=gb(accessed on 27 Jan 2022)
- ↑ Noorani A, Goldring M, Jaggi A, Gibson J, Rees J, Bateman M, Falworth M, Brownson P. BESS/BOA patient care pathways: atraumatic shoulder instability. Shoulder & elbow. 2019 Feb;11(1):60-70.
- ↑ Jaggi A. Rehabilitation for shoulder instability. Br J Sports Med 2010;44(5):333.
- ↑ Yang J, Lin J. Reliability of function-related tests in patients with shoulder pathologies. JOSPT. 2006;36: 572-576.
- ↑ Gross M, Disefano M. Anterior release test: A new test for occult shoulder instability. Clinical Orthopaedics and Related Research. 1997;339:105-108.
- ↑ 17.0 17.1 Lo IK, Nonweiler B, Woolfrey M, Litchfield R, Kirkley A. An evaluation of the apprehension, relocation, and surprise tests for anterior shoulder instability. Am J Sports Med.2004;32:301-7
- ↑ Tzannes A, Murrel, GAC. An assessment of the interexaminar reliability of tests for shoulder instability. The journal of Shoulder and Elbow Surgery 2004; 13:18-23.
- ↑ Tzannes A, Murell GAC. Clinical examination of the unstable shoulder. Sports Medicine 2002; 32: 447-457.
- ↑ Tzannes et al. 2004
- ↑ Tzannes et al. 2002
- ↑ Ian KY, Lo IKY, Nonweiler B, et al. An evaluation of the apprehension, relocation, and surprise test for anterior shoulder instability. American Journal of Sports Medicine 2004; 32:301-307.
- ↑ Levy AS, Lintner S, Kenter K, et al: intra- and interobserver reproducibility of the shoulder laxity examination. The American Journal of Sports medicine 1999; 4: 460-463.
- ↑ Ian et al.
- ↑ Tzannes A, Murrel, GAC. An assessment of the interexaminar reliability of tests for shoulder instability. The journal of Shoulder and Elbow Surgery 2004; 13:18-23.
- ↑ Marx RG, Bombardier C, Wright JG. What do we know about the reliability and validity of physical examination tests used to examine the upper extremity? Journal of Hand Surgery 1999; 24A:185-193.
- ↑ Ian et al.
- ↑ Tzannes et al. 2004
- ↑ Liu SH, Henry MH, Nuccion S, et al. Diagnosis of glenoid labral tears. A comparison between magnetic resonance imaging and clinical examinations. The American Journal of Sports Medicine 1996; 2:149-154.
- ↑ Breckenridge JD, McAuley JH. Shoulder pain and disability index (SPADI). Journal of physiotherapy. 2011 Jan 1;57(3):197-.
- ↑ Rouleau D, Faber K, MacDermin J. Systematic review of patient-administered shoulder functional scores on instability. J Shoulder Elbow Surg. 2010;19:1121-1128.
- ↑ Mintken. Some Factors Predict Successful Short-Term Outcomes in IndividualsWith Shoulder Pain Receiving Cervicothoracic Manipulation: A Single-Arm Trial. PTJ 2010;26-42.
- ↑ Eshoj, H.R., Rasmussen, S., Frich, L.H., Hvass, I., Christensen, R., Boyle, E., Jensen, S.L., Søndergaard, J., Søgaard, K. and Juul-Kristensen, B., 2020. Neuromuscular exercises improve shoulder function more than standard care exercises in patients with a traumatic anterior shoulder dislocation: a randomized controlled trial. Orthopaedic journal of sports medicine, 8(1), p.2325967119896102. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6993151/(accessed 28.1.2022)
- ↑ WATSON, Lyn, et al. The effects of a conservative rehabilitation program for multidirectional instability of the shoulder. Journal of shoulder and elbow surgery, 2018, 27.1: 104-111. Available:https://www.sciencedirect.com/science/article/abs/pii/S1058274617304238 (accessed 28.1.2022)
- ↑ TANNENBAUM, Eric; SEKIYA, Jon K. Evaluation and management of posterior shoulder instability. Sports Health, 2011, 3.3: 253-263.
- ↑ 36.0 36.1 Goldenberg BT, Goldsten P, Lacheta L, Arner JW, Provencher MT, Millett PJ. Rehabilitation Following Posterior Shoulder Stabilization. International Journal of Sports Physical Therapy. 2021;16(3):930.