Low Back Pain Related to Hyperlordosis: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (150 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Gertjan Peeters|Gertjan Peeters]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original | '''Original Editor '''- Your name will be added here if you created the original content for this page. | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition == | |||
[[File:Posture types (vertebral column).jpg|right|frameless|400x400px]] | |||
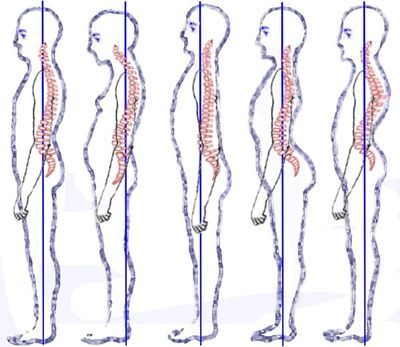
The lordotic posture [see 2 images on far right as opposed to [[Sway Back Posture|sway back posture]] second from the left] represents a faulty posture that differs from the good one by the following: | |||
# Increased lumbar lordosis and | |||
# Increased pelvic anteversion (anterior tilt). | |||
Increased anterior tilt of the pelvis leads to increased flexion of hip joints. The knees can be in hyperextension and, due to this knee position, the plantar flexion of the feet occurs<ref name=":5">Czaprowski D, Stoliński Ł, Tyrakowski M, Kozinoga M, Kotwicki T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis and spinal disorders. 2018 Dec 1;13(1):6. Available from: <nowiki>https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5836359/</nowiki> (last accessed 10.12.2019)</ref> | |||
There is increasing recognition of the importance (functional and clinical) of lumbar lordosis. It is a key feature in maintaining sagittal balance.<ref name=":0">Been, Ella, and Leonid Kalichman. "Lumbar lordosis." The Spine Journal 2014; 14.1: 87-97.</ref> [See [[Cardinal Planes and Axes of Movement|Cardinal planes]]] Sagittal disposition outside the ranges of normality result in decreased functional capacity and perceived quality of life. In addition, spinal misalignment is associated with a slow gait, poor balance and a higher risk of falls.<ref name=":6">González-Gálvez N, Gea-García GM, Marcos-Pardo PJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6488071/ Effects of exercise programs on kyphosis and lordosis angle: A systematic review and meta-analysis.] PloS one. 2019 Apr 29;14(4):e0216180. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6488071/ (last accessed 12.12.2019)</ref> | |||
When planning physiotherapeutic intervention using postural corrective exercises, not only the analysis of muscles in respect to their shortening and lengthening but also their hypoactivity and hyperactivity should be considered. The practice of a systematic and continuous exercise can influence sagittal spinal curvature<ref name=":6" />. | |||
== Clinically Relevant Anatomy | == Clinically Relevant Anatomy == | ||
[[File:Posture .gif|right|frameless|442x442px]] | |||
If a straight lumbar spine articulated with the sacrum, it would consequently be inclined forwards. To restore an upward orientation and to compensate for the inclination of the sacrum, the intact lumbar spine must assume a curve. This curve is known as the lumbar lordosis.<ref>Bogduk, Nikolai. “Clinical anatomy of the lumbar spine and sacrum”. Elsevier Health Sciences, 2005 </ref> | |||
Normal lumbar lordosis is characterized by an average lumbosacral angle of 39° - 53°.<ref name=":3">Polly Jr, David W., et al. "Measurement of lumbar lordosis: evaluation of intraobserver, interobserver, and technique variability." Spine 21.13 (1996): 1530-1535. </ref>, the results depend on how the lumbosacral angle is measured and there is an enormous difference in lumbosacral angle over patients. | |||
[ | The angle between the base of the sacrum and its pelvic surface, Sacral Angle.The lumbosacral curve (LSC) is defined as the anteroposterior distance between the L1 vertebra and the sacrum. SA is smaller whereas LSC is larger in black adult men and women when compared to white adult men and women.<ref>[https://pubmed.ncbi.nlm.nih.gov/9831771/ Hanson P, Magnusson SP, Simonsen EB. Differences in sacral angulation and lumbosacral curvature in black and white young men and women. Acta Anat (Basel). 1998;162(4):226-31. doi: 10.1159/000046437. PMID: 9831771.]</ref> | ||
However, when the curvature of the lumbar spine is very pronounced, it refers to hyperlordosis, this means that the lumbosacral angle and the lumbar index (the chord of the lumbar lordosis) increase.<ref name=":3" /> As opposed to [[Sway Back Posture|Sway Back posture]] | |||
In addition to the bones, ligaments, muscles and vertebral discs have also a key role in lordosis curvature. Without muscle action, the performance of the pelvic girdle would not have sufficient stability. Central stabilize of the vertebral column is supported by special muscles such as multifidus, transversus abdominis and internal muscles in the trunk. They provide stability of vertebrae in a focal form and provide also segmental stabilization by controlling motion in the neutral zone. The neutral zone can be regained to within physiological limits by effective muscle control. | |||
Women have less vertebral wedging in the lower thoracic and upper lumbar vertebrae, they have relatively greater interspinous space and larger inter facet within lumbar hyperlordosis in. These anatomical features could explain the altered vertebral morphology predisposing to pregnancy.In a study conducted on black and white female adults,it was found that black women had a greater lordosis than white women.<ref>[https://pubmed.ncbi.nlm.nih.gov/2711246/ Mosner EA, Bryan JM, Stull MA, Shippee R. A comparison of actual and apparent lumbar lordosis in black and white adult females. Spine (Phila Pa 1976). 1989 Mar;14(3):310-4. doi: 10.1097/00007632-198903000-00011. PMID: 2711246.]</ref> | |||
Women also have a less kyphotic posture of the upper and the lower thoracic area than males. Furthermore, the trunk’s center of mass is maintained in an approximate sagittal alignment with the hip thus reducing biomechanical load and facilitating spinal extension. There is an advantage of this deeper lordosis- less kyphotic female spine because there is a larger superior-inferior space for the human fetus. The downside of this morphological feature is the resultant size reduction of the intervertebral foramen which in turn may contribute to low back pain commonly experienced in pregnancy.<ref name=":10">Gomes-Neto, Mansueto, et al. "Stabilization exercise compared to general exercises or manual therapy for the management of low back pain: A systematic review and meta-analysis." Physical Therapy in Sport (2016).</ref> | |||
==Low Back Pain Related to Hyperlordosis== | |||
An increase in lordotic angle proportionally increases the shearing strain or stress in the anterior direction and shifts the center of gravity anteriorly. This increased angle and stress are thought by some to be associated with poor posture and back pain. From a biomechanical point of view, the accentuated lumbar lordosis is associated with an increased prevalence of low back pain. <ref name=":2">Fatemi, Rouholah, Marziyeh Javid, and Ebrahim Moslehi Najafabadi. "Effects of William training on lumbosacral muscles function, lumbar curve and pain." Journal of back and musculoskeletal rehabilitation 2015; 28.3: 591-597. | |||
</ref>However several studies have concluded that low back pain is not directly related to lumbar hyperlordosis. There are factors that contribute to a higher amount of lumbar lordosis. These etiological factors, like the weakness of the trunk, short back muscles, weak thigh, and hamstrings, etc. in turn can cause low back pain. | |||
= | It is important to mention that not solely the lumbar hyperlordosis is the causing factor for low back pain. It is thus not reasonable to conclude that there is a relationship between LBP and the size of the lumbar lordosis.<ref name=":4">Nourbakhsh, Mohammad Reza, and Amir Massoud Arab. "Relationship between mechanical factors and incidence of low back pain." Journal of Orthopaedic & Sports Physical Therapy 32.9 (2002): 447-460. </ref> On the other hand, it is likely that trunk muscle weakness can influence the shape of the lumbar lordosis and might be a cause of LBP.<ref name=":2" /> | ||
The multifidus, transversus abdominis and internal muscles in the trunk act late in patients with hyperlordosis. <ref name=":2" /> There is a correlation between the weakness of the trunk muscles and an increased lordotic angle, which can be a cause of low back pain<ref name=":1">Kim, Ho-Jun, et al. "Influences of trunk muscles on lumbar lordosis and sacral angle." European Spine Journal 15.4 (2006): 409-414. </ref>. Weakness in any of the muscles of the lumbar-pelvic belt can follow pelvic rotations and diversions of back-arc by impairing muscular balance in this area and thus a person can be prone to musculoskeletal disorders.<ref name=":2" /> | |||
= | There are various factors affecting lumbar lordosis. Some studies show that the range of lumbar lordosis is affected by age, sex, movement in the center of mass such as pregnancy and obesity.<ref name=":2" /> Possible causes of hyperlordosis: | ||
*Congenital spine deformities | |||
*Interior tilt of the hip | |||
*Short back muscles | |||
*Imbalance between the muscles surrounding the pelvic bones ie Tight hip flexors, weak core muscles, weak gluteal muscles. This muscular imbalance ([[Lower Crossed Syndrome]]) causes the postural muscles to shorten in response to stress and they, in turn, inhibit their antagonists. | |||
People with low back pain have reduced lumbar ROM and proprioception. Their stabilizing muscles act more slowly compared to people without LBP. Normally the stabilizing muscles are activated before the movement is initiated, but in people with low back pain, this contraction is delayed.<ref>Laird RA, Gilbert J, Kent P, Keating JL. Comparing lumbo-pelvic kinematics in people with and without back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2014 Jul 10;15:229. doi: 10.1186/1471-2474-15-229. PMID: 25012528; PMCID: PMC4096432.[https://pubmed.ncbi.nlm.nih.gov/25012528/] </ref> | |||
== Differential Diagnosis == | |||
It’s essential to make a correct postural assessment and not confuse with eg [[Sway Back Posture|sway back posture]] as treatment pins on your identification of correct postural fault. In sway back posture the [[Pelvic Tilt|pelvis]] is posteriorly tilted as opposed to the lordotic lumbar spine when it is anteriorly tilted. | |||
[[Spondylolisthesis|Spondylolistheis]] is a serious condition that should be ruled out, as should more serious conditions by doing a complete [[Lumbar Examination|lumbar spine examination.]] | |||
== | == Physiotherapy Assessment == | ||
=== A Good Postural Assessment === | |||
In the ideal posture, the head line, beginning at the external auditory meatus (or at the mastoid process of the temporal bone), should run vertically through the acromion, the lumbar vertebral bodies, the promontory, then slightly posteriorly to the hip joint axis, slightly in front of the knee joint axis, and finish at the lateral malleolus or slightly in front of it. The course of this line in a good body posture overlaps the base line joining the center of gravity with the central point of the supporting area ( | |||
== | In the lordotic posture the head line runs down posteriorly to lumbar vertebral bodies, passing near the intervertebral facet joints, which results in extensory overloading within the facets. The head line is also anterior to the knee joint axis, which leads to the overloading of the anterior knee compartment (Fig. 6). The head line may overlap the base line, or in the case of head protraction, it may run in front of it<br><sup></sup> | ||
===Spinal Curve Measurement=== | |||
The normal curve of the lumbar spine should be approx 30-35 degrees while standing. | |||
* Evaluate the space between the lumbar spine and the wall. When a person has an acceptable degree of lumbar lordosis, you should only be able to slide your fingers behind the lower back up to, and in line with the second or third knuckle of your hand (i.e., where the fingers meet the hand). If the space between the back and the wall is big enough for you to slide your whole hand or arm through, then the client has excessive lumbar lordosis. The greater the space is between the wall and the lower back, the more extreme the deviation or imbalance is.<ref>Physiotherapy and recovery [https://beyutza.wordpress.com/2014/02/16/lumbar-lordosis/ Lumbar Lordosis]. Available from: https://beyutza.wordpress.com/2014/02/16/lumbar-lordosis/ (last accessed 12.12.2019)</ref> | |||
*The lumbar angle and sacral angle can be measured with a goniometer. The sacral angle is the angle between the horizontal line parallel to the bottom end and the superior endplate of the sacrum. The lumbar angle can be measured between the Inferior endplate of L5 and the superior endplate of L1: this is called the method of Cobb.<ref name=":1" /> However, the reliability of the goniometer is still questioned. <ref name=":8">Bryan, Jean M., et al. "Investigation of the Flexible Ruler as a Noninvasive Measure of Lumbar Lordosis in Black and White Adult Female Sample Populations*." Journal of Orthopaedic & Sports Physical Therapy 11.1 (1989): 3-7. </ref> | |||
== Physical Therapy Management == | |||
[[File:Pelvic tilt 1.jpg|right|frameless]] | |||
'''Education is vital.''' Educate them on the points below: | |||
* Correct postural positions in sitting, standing, walking and ADL's. Poor posture is one of the most common causes of hyperlordosis. When the body is in a seated position, muscles in the lumbar region can tighten too much as they try to stabilize and support the spinal column. This gradually pulls the spine out of alignment, causing increased curving of the spine. People with jobs that require them to sit for extended periods may have a higher risk of getting hyperlordosis. | |||
* Importance of exercise - addition to increasing the risk of obesity, a lack of exercise can weaken the core muscles that sit around the trunk and pelvis. Weak muscles are less able to support the spinal column, allowing the spine to curve excessively | |||
* Teach how to perform a basic pelvic tilt manoeuvre. This is first learnt in supine and progress to on all fours and then in standing. | |||
The below video gives a good overview of the essential education points and the exercises to perform. | |||
{{#ev:youtube|https://www.youtube.com/watch?v=2NZMaI-HeNU|width}}<ref>J Ethier Fix "Anterior Pelvic Tilt" in 10 Minutes/Day (Daily Exercise Routine) Available from: https://www.youtube.com/watch?v=2NZMaI-HeNU (last accessed 12.12.2019)</ref> | |||
'''The imbalance of muscle pull around the pelvis must be addressed'''. This involves releasing/stretching the tight muscles and strengthening the weakened muscles. | |||
Tight/overactive: | |||
* [[Psoas Major|Iliopsoas]] | |||
* [[Tensor Fascia Lata|Tensor fascia latae]] | |||
* [[Rectus Femoris|Rectus femoris]] (Quadriceps) | |||
* Lower back erectors | |||
* Longissimus, iliocostalis | |||
* Quadratus lumborum | |||
* [[Thoracolumbar Fascia|Thoracolumbar fascia]] | |||
* [[Latissimus Dorsi Muscle|Latissimus dorsi]] | |||
* Anterior fibres of the adductors | |||
Weak/inhibited: | |||
* Gluteal group | |||
* [[Hamstrings|Hamstring]] | |||
* Abdominals<br> | |||
The below protocol is one example of an effective program. | |||
< | === Williams Training Protocol === | ||
This is an exercise protocol for men under 50 years and women under 40 years which had a lumbar hyperlordosis, whose radiography showed a contraction of the lumbar segment interarticular space.<ref name=":2" /> The purpose of these exercises was to reduce pain and to ensure the stability of the lower trunk by toning the abdominal muscles, buttocks, and hamstrings altogether with the passive extent of hip flexors and sacrospinalis muscles. Each group performed special training for 8 weeks: | |||
• 3 sessions per week: about 1 hour. | |||
• Duration of each exercise: 8 to 10 seconds in each set. | |||
• Protocols were started with 1 set of 10 repetitions at starting baseline and by improving performance and patients’ compatibility with training, all eventually finished with 3 sets of 20 repetitions at the end of protocols. | |||
# '''[[Pelvic Tilt|Pelvic Tilt]]:''' The patient lies on his back with knees bent, feet flat on floor. Cue: Flatten the small of your back against the floor, without pushing down with the legs, hold for 5 to 10 seconds. | |||
# '''Single Knee to chest:''' The patient lies on his back with knees bent and feet flat on the floor. Cue: Slowly pull your right knee toward your shoulder and hold 5 to 10 seconds. Lower the knee and repeat with the other knee. | |||
# '''Double knee to chest:''' The patient begins as in the previous exercise. Cue: Pulling right knee to chest, pull left knee to chest and hold both knees for 5 to 10 seconds. Slowly lower one leg at a time. | |||
# Partial sit-up: The patient has to do the pelvic tilt ''(exercise 1)'' and while holding this position Cue: Slowly curl your head and shoulders off the floor. Hold briefly. Return slowly to the starting position. | |||
# Hamstring stretch: The patient starts in long sitting with toes directed toward the ceiling and knees fully extended. Cue: Slowly lower the trunk forward over the legs, keeping knees extended, arms outstretched over the legs, and eyes focus ahead. | |||
# Hip Flexor stretch: The patient places one foot in front of the other with the left (front) knee flexed and the right (back) knee held rigidly straight. Cue: Flex forward through the trunk until the left knee contacts the axillary fold (armpit region). Repeat with right leg forward and left leg back. | |||
# Squat: The patient stands with both feet parallel, about shoulder’s width apart. Attempting to maintain the trunk as perpendicular as possible to the floor, eyes focused ahead, and feet flat on the floor. Cue: Slowly lower the body by flexing the knees. | |||
< | === Other Treatment Options === | ||
In order to bring variation in the therapy, you can perform other sports. The most recommended sports are walking swimming and cross-training. You better avoid contact sports like basketball. <ref name=":9">Wong, J. J., et al. "Clinical practice guidelines for the noninvasive management of low back pain: A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration." European Journal of Pain (2016). </ref> | |||
==== Strengthening Exercises ==== | |||
* Isometric and isotonic exercises:'' May be beneficial for strengthening of the main muscle groups of the trunk, which stabilizes the spine and it can also decrease the pain''<ref name=":11">[https://pubmed.ncbi.nlm.nih.gov/15867410/ Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005 May 3;142(9):776-85. doi: 10.7326/0003-4819-142-9-200505030-00014. PMID: 15867410.]</ref>''. '' | |||
** The patient should gradually build up these exercises until he can hold it for 10 x 10sec. <ref name=":12">Hodges PW. Core stability exercise in chronic low back pain. Orthop Clin North Am 2003;34:245-254. Barr KP, Griggs M, Cadby T. Lumbar stabilization: core concepts and current literature, Part 1. Am J Phys Med Rehabil 2005;84:473-480. </ref> | |||
** Through core strength training, patients with chronic low back pain can strengthen their deep trunk muscles. | |||
** There is an enormous range of exercises on the ground to increase [https://www.physio-pedia.com/Core_stability core stability]. <ref name=":12" /> | |||
== | * Motor control exercises'':'' Seem to have beneficial effects on pain and disability. <ref>Byström, Martin Gustaf, Eva Rasmussen-Barr, and Wilhelmus Johannes Andreas Grooten. "Motor control exercises reduces pain and disability in chronic and recurrent low back pain: a meta-analysis." Spine 38.6 (2013): E350-E358. </ref> | ||
** The patient needs to learn to activate the transversus abdominis muscle and at the same time to breath normally during the exercise. Palpation can give him/her feedback. | |||
** The next step would be a co-contraction with the multifidus muscle and the pelvic floor muscles. | |||
** When the patient has a good performance of this exercise, the physical therapist could combine the exercise with movements of the arms or legs. | |||
** After that, the patient should integrate the contraction of the transversus abdominis muscle in the ADL. <ref name=":13">Unsgaard-Tøndel, Monica, et al. "Motor control exercises, sling exercises, and general exercises for patients with chronic low back pain: a randomized controlled trial with 1-year follow-up." Physical therapy 90.10 (2010): 1426-1440. </ref> | |||
====Stretching Exercises ==== | |||
With a crossed leg syndrome type of problem, it’s beneficial to stretch the tightened muscles. For improving the mobility, the patient could perform stretching of the hamstrings, hip flexors, and lumbar paraspinal muscles over 15 seconds. This will improve the active and the passive ROM in the lower extremity.<ref name=":11" /> | |||
* Hold-relax stretching of the iliopsoas: It can reduce back pain, excessive lumbar lordosis angle, lengthen the iliopsoas and increase transversus abdominis activation capacity. The target hip is moved toward the floor until the patient feels a mild stretch sensation. Then the patient must perform a submaximal voluntary isometric contraction of the M. Iliopsoas for 10 seconds and then completely relax for 10 seconds. The participant’s leg is now slowly moved to a new range until a mild stretching sensation is felt and described by the patient. This position is then held for 20 seconds. This is repeated 5 times, followed by a 1 min rest, for 15 minutes. <ref>Malai, Suthichan, Sopa Pichaiyongwongdee, and Prasert Sakulsriprasert. "Immediate Effect of Hold-Relax Stretching of Iliopsoas Muscle on Transversus Abdominis Muscle Activation in Chronic Non-Specific Low Back Pain with Lumbar Hyperlordosis." J Med Assoc Thai 2015; 98 (Suppl. 5): S6-S11. </ref> | |||
== | * Stretching technique for improving the ROM of the M.Iliopsoas and the M. Rectus femoris: The patient lies in Thomas position, the not stretched leg is maximally flexed to stabilize the pelvis and flatten the lumbar spine. The other leg is in a normal flexed position because of the tightness of the M. Iliopsoas. It’s this leg that needs to be pushed against the table. If you want to stretch the M. rectus femoris, bend the knee more than 90°, while performing the same stretch. | ||
==== Stabilization Exercises ==== | |||
The stabilization exercises may be beneficial for reducing pain and disability. <ref name=":10" /> Patients following a supervised spinal stabilization exercise program show higher pain reduction compared to patients following another exercise program. During external perturbation, there is a decreased anterior-posterior displacement.<ref>Rhee, Hyun Sill, Yoon Hyuk Kim, and Paul S. Sung. "A randomized controlled trial to determine the effect of spinal stabilization exercise intervention based on pain level and standing balance differences in patients with low back pain." Medical Science Monitor 18.3 (2012): CR174-CR189. </ref> | |||
====Sling Exercise Training==== | |||
Sling exercise training seems to be effective at reducing the pain intensity and disability levels of LBP patients. The patient is suspended in a system of pulleys. He/She has to move the arms or legs, while he/she keeps the spine in a neutral position. Both the deep and superficial muscles need to contract.<ref name=":13" /> The patient can also put only his feet in the sling while he can perform some bridging exercises. | |||
==== The Swiss Ball==== | |||
The exercises on the swiss ball demand contraction of the stabilizing muscles, but there is also a contraction of the rectus abdominis muscle <ref>Marshall, Paul W., and Bernadette A. Murphy. "Core stability exercises on and off a Swiss ball." Archives of physical medicine and rehabilitation 86.2 (2005): 242-249. </ref> | |||
==== Exercise Therapy ==== | |||
Exercise therapy, including supervised exercises, appears to be slightly effective at decreasing pain and improving function in adults with chronic low-back pain, particularly in healthcare populations. Patients with an acute outburst of low back pain who received exercise therapy in addition to the medical management had fewer recurrences over a long time. [1] Decreasing the extension forces on the lumbar spine must be the purpose of the exercises. This can result in a decreased lumbar lordosis. Exercises should be done on a regular basis to reach maximum effect. | |||
== Outcome Measures == | |||
* Oswestry Disability Index is the most effective for persistent severe disability. [[Oswestry Disability Index]] <ref name=":7">Davies, Claire C., and Arthur J. Nitz. "Psychometric properties of the Roland-Morris Disability Questionnaire compared to the Oswestry Disability Index: a systematic review." Physical therapy reviews 2013; 14.6: 399-408</ref> | |||
* Roland-Morris Disability Questionnaire is better for mild to moderate disability. [[Roland‐Morris Disability Questionnaire]] <ref name=":7" /> | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
In most cases, hyperlordosis is due to specific lifestyle factors. Often, maintaining a healthy weight and exercising regularly can improve issues with posture and lower back pain. | |||
NB In some cases, hyperlordosis may be the result of other underlying spinal problems, such as kyphosis, spondylolisthesis, and discitis and these must be ruled out if problems persist or red flags evident.<ref>Medical news today [https://www.medicalnewstoday.com/articles/321959.php Lumbar lordosis] Available from: https://www.medicalnewstoday.com/articles/321959.php (last accessed 12.12.2019)</ref> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Lumbar Spine]] | |||
[[Category:Interventions]] | |||
[[Category:Pain]] | |||
[[Category:Lumbar]] [[Category: | |||
Latest revision as of 16:49, 10 August 2022
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Lise Buelens, Leen Meylemans, Claudia Karina, Loes Verspecht, Gertjan Peeters, Lucinda hampton, Cameron Mostinckx, Rishika Babburu, Admin, Kim Jackson, Geubels Kaat, Evan Thomas and Oyemi Sillo
Definition[edit | edit source]
The lordotic posture [see 2 images on far right as opposed to sway back posture second from the left] represents a faulty posture that differs from the good one by the following:
- Increased lumbar lordosis and
- Increased pelvic anteversion (anterior tilt).
Increased anterior tilt of the pelvis leads to increased flexion of hip joints. The knees can be in hyperextension and, due to this knee position, the plantar flexion of the feet occurs[1]
There is increasing recognition of the importance (functional and clinical) of lumbar lordosis. It is a key feature in maintaining sagittal balance.[2] [See Cardinal planes] Sagittal disposition outside the ranges of normality result in decreased functional capacity and perceived quality of life. In addition, spinal misalignment is associated with a slow gait, poor balance and a higher risk of falls.[3]
When planning physiotherapeutic intervention using postural corrective exercises, not only the analysis of muscles in respect to their shortening and lengthening but also their hypoactivity and hyperactivity should be considered. The practice of a systematic and continuous exercise can influence sagittal spinal curvature[3].
Clinically Relevant Anatomy[edit | edit source]
If a straight lumbar spine articulated with the sacrum, it would consequently be inclined forwards. To restore an upward orientation and to compensate for the inclination of the sacrum, the intact lumbar spine must assume a curve. This curve is known as the lumbar lordosis.[4]
Normal lumbar lordosis is characterized by an average lumbosacral angle of 39° - 53°.[5], the results depend on how the lumbosacral angle is measured and there is an enormous difference in lumbosacral angle over patients.
The angle between the base of the sacrum and its pelvic surface, Sacral Angle.The lumbosacral curve (LSC) is defined as the anteroposterior distance between the L1 vertebra and the sacrum. SA is smaller whereas LSC is larger in black adult men and women when compared to white adult men and women.[6]
However, when the curvature of the lumbar spine is very pronounced, it refers to hyperlordosis, this means that the lumbosacral angle and the lumbar index (the chord of the lumbar lordosis) increase.[5] As opposed to Sway Back posture
In addition to the bones, ligaments, muscles and vertebral discs have also a key role in lordosis curvature. Without muscle action, the performance of the pelvic girdle would not have sufficient stability. Central stabilize of the vertebral column is supported by special muscles such as multifidus, transversus abdominis and internal muscles in the trunk. They provide stability of vertebrae in a focal form and provide also segmental stabilization by controlling motion in the neutral zone. The neutral zone can be regained to within physiological limits by effective muscle control.
Women have less vertebral wedging in the lower thoracic and upper lumbar vertebrae, they have relatively greater interspinous space and larger inter facet within lumbar hyperlordosis in. These anatomical features could explain the altered vertebral morphology predisposing to pregnancy.In a study conducted on black and white female adults,it was found that black women had a greater lordosis than white women.[7]
Women also have a less kyphotic posture of the upper and the lower thoracic area than males. Furthermore, the trunk’s center of mass is maintained in an approximate sagittal alignment with the hip thus reducing biomechanical load and facilitating spinal extension. There is an advantage of this deeper lordosis- less kyphotic female spine because there is a larger superior-inferior space for the human fetus. The downside of this morphological feature is the resultant size reduction of the intervertebral foramen which in turn may contribute to low back pain commonly experienced in pregnancy.[8]
Low Back Pain Related to Hyperlordosis[edit | edit source]
An increase in lordotic angle proportionally increases the shearing strain or stress in the anterior direction and shifts the center of gravity anteriorly. This increased angle and stress are thought by some to be associated with poor posture and back pain. From a biomechanical point of view, the accentuated lumbar lordosis is associated with an increased prevalence of low back pain. [9]However several studies have concluded that low back pain is not directly related to lumbar hyperlordosis. There are factors that contribute to a higher amount of lumbar lordosis. These etiological factors, like the weakness of the trunk, short back muscles, weak thigh, and hamstrings, etc. in turn can cause low back pain.
It is important to mention that not solely the lumbar hyperlordosis is the causing factor for low back pain. It is thus not reasonable to conclude that there is a relationship between LBP and the size of the lumbar lordosis.[10] On the other hand, it is likely that trunk muscle weakness can influence the shape of the lumbar lordosis and might be a cause of LBP.[9]
The multifidus, transversus abdominis and internal muscles in the trunk act late in patients with hyperlordosis. [9] There is a correlation between the weakness of the trunk muscles and an increased lordotic angle, which can be a cause of low back pain[11]. Weakness in any of the muscles of the lumbar-pelvic belt can follow pelvic rotations and diversions of back-arc by impairing muscular balance in this area and thus a person can be prone to musculoskeletal disorders.[9]
There are various factors affecting lumbar lordosis. Some studies show that the range of lumbar lordosis is affected by age, sex, movement in the center of mass such as pregnancy and obesity.[9] Possible causes of hyperlordosis:
- Congenital spine deformities
- Interior tilt of the hip
- Short back muscles
- Imbalance between the muscles surrounding the pelvic bones ie Tight hip flexors, weak core muscles, weak gluteal muscles. This muscular imbalance (Lower Crossed Syndrome) causes the postural muscles to shorten in response to stress and they, in turn, inhibit their antagonists.
People with low back pain have reduced lumbar ROM and proprioception. Their stabilizing muscles act more slowly compared to people without LBP. Normally the stabilizing muscles are activated before the movement is initiated, but in people with low back pain, this contraction is delayed.[12]
Differential Diagnosis[edit | edit source]
It’s essential to make a correct postural assessment and not confuse with eg sway back posture as treatment pins on your identification of correct postural fault. In sway back posture the pelvis is posteriorly tilted as opposed to the lordotic lumbar spine when it is anteriorly tilted.
Spondylolistheis is a serious condition that should be ruled out, as should more serious conditions by doing a complete lumbar spine examination.
Physiotherapy Assessment[edit | edit source]
A Good Postural Assessment[edit | edit source]
In the ideal posture, the head line, beginning at the external auditory meatus (or at the mastoid process of the temporal bone), should run vertically through the acromion, the lumbar vertebral bodies, the promontory, then slightly posteriorly to the hip joint axis, slightly in front of the knee joint axis, and finish at the lateral malleolus or slightly in front of it. The course of this line in a good body posture overlaps the base line joining the center of gravity with the central point of the supporting area (
In the lordotic posture the head line runs down posteriorly to lumbar vertebral bodies, passing near the intervertebral facet joints, which results in extensory overloading within the facets. The head line is also anterior to the knee joint axis, which leads to the overloading of the anterior knee compartment (Fig. 6). The head line may overlap the base line, or in the case of head protraction, it may run in front of it
Spinal Curve Measurement[edit | edit source]
The normal curve of the lumbar spine should be approx 30-35 degrees while standing.
- Evaluate the space between the lumbar spine and the wall. When a person has an acceptable degree of lumbar lordosis, you should only be able to slide your fingers behind the lower back up to, and in line with the second or third knuckle of your hand (i.e., where the fingers meet the hand). If the space between the back and the wall is big enough for you to slide your whole hand or arm through, then the client has excessive lumbar lordosis. The greater the space is between the wall and the lower back, the more extreme the deviation or imbalance is.[13]
- The lumbar angle and sacral angle can be measured with a goniometer. The sacral angle is the angle between the horizontal line parallel to the bottom end and the superior endplate of the sacrum. The lumbar angle can be measured between the Inferior endplate of L5 and the superior endplate of L1: this is called the method of Cobb.[11] However, the reliability of the goniometer is still questioned. [14]
Physical Therapy Management[edit | edit source]
Education is vital. Educate them on the points below:
- Correct postural positions in sitting, standing, walking and ADL's. Poor posture is one of the most common causes of hyperlordosis. When the body is in a seated position, muscles in the lumbar region can tighten too much as they try to stabilize and support the spinal column. This gradually pulls the spine out of alignment, causing increased curving of the spine. People with jobs that require them to sit for extended periods may have a higher risk of getting hyperlordosis.
- Importance of exercise - addition to increasing the risk of obesity, a lack of exercise can weaken the core muscles that sit around the trunk and pelvis. Weak muscles are less able to support the spinal column, allowing the spine to curve excessively
- Teach how to perform a basic pelvic tilt manoeuvre. This is first learnt in supine and progress to on all fours and then in standing.
The below video gives a good overview of the essential education points and the exercises to perform.
The imbalance of muscle pull around the pelvis must be addressed. This involves releasing/stretching the tight muscles and strengthening the weakened muscles.
Tight/overactive:
- Iliopsoas
- Tensor fascia latae
- Rectus femoris (Quadriceps)
- Lower back erectors
- Longissimus, iliocostalis
- Quadratus lumborum
- Thoracolumbar fascia
- Latissimus dorsi
- Anterior fibres of the adductors
Weak/inhibited:
- Gluteal group
- Hamstring
- Abdominals
The below protocol is one example of an effective program.
Williams Training Protocol[edit | edit source]
This is an exercise protocol for men under 50 years and women under 40 years which had a lumbar hyperlordosis, whose radiography showed a contraction of the lumbar segment interarticular space.[9] The purpose of these exercises was to reduce pain and to ensure the stability of the lower trunk by toning the abdominal muscles, buttocks, and hamstrings altogether with the passive extent of hip flexors and sacrospinalis muscles. Each group performed special training for 8 weeks:
• 3 sessions per week: about 1 hour.
• Duration of each exercise: 8 to 10 seconds in each set.
• Protocols were started with 1 set of 10 repetitions at starting baseline and by improving performance and patients’ compatibility with training, all eventually finished with 3 sets of 20 repetitions at the end of protocols.
- Pelvic Tilt: The patient lies on his back with knees bent, feet flat on floor. Cue: Flatten the small of your back against the floor, without pushing down with the legs, hold for 5 to 10 seconds.
- Single Knee to chest: The patient lies on his back with knees bent and feet flat on the floor. Cue: Slowly pull your right knee toward your shoulder and hold 5 to 10 seconds. Lower the knee and repeat with the other knee.
- Double knee to chest: The patient begins as in the previous exercise. Cue: Pulling right knee to chest, pull left knee to chest and hold both knees for 5 to 10 seconds. Slowly lower one leg at a time.
- Partial sit-up: The patient has to do the pelvic tilt (exercise 1) and while holding this position Cue: Slowly curl your head and shoulders off the floor. Hold briefly. Return slowly to the starting position.
- Hamstring stretch: The patient starts in long sitting with toes directed toward the ceiling and knees fully extended. Cue: Slowly lower the trunk forward over the legs, keeping knees extended, arms outstretched over the legs, and eyes focus ahead.
- Hip Flexor stretch: The patient places one foot in front of the other with the left (front) knee flexed and the right (back) knee held rigidly straight. Cue: Flex forward through the trunk until the left knee contacts the axillary fold (armpit region). Repeat with right leg forward and left leg back.
- Squat: The patient stands with both feet parallel, about shoulder’s width apart. Attempting to maintain the trunk as perpendicular as possible to the floor, eyes focused ahead, and feet flat on the floor. Cue: Slowly lower the body by flexing the knees.
Other Treatment Options[edit | edit source]
In order to bring variation in the therapy, you can perform other sports. The most recommended sports are walking swimming and cross-training. You better avoid contact sports like basketball. [16]
Strengthening Exercises[edit | edit source]
- Isometric and isotonic exercises: May be beneficial for strengthening of the main muscle groups of the trunk, which stabilizes the spine and it can also decrease the pain[17].
- The patient should gradually build up these exercises until he can hold it for 10 x 10sec. [18]
- Through core strength training, patients with chronic low back pain can strengthen their deep trunk muscles.
- There is an enormous range of exercises on the ground to increase core stability. [18]
- Motor control exercises: Seem to have beneficial effects on pain and disability. [19]
- The patient needs to learn to activate the transversus abdominis muscle and at the same time to breath normally during the exercise. Palpation can give him/her feedback.
- The next step would be a co-contraction with the multifidus muscle and the pelvic floor muscles.
- When the patient has a good performance of this exercise, the physical therapist could combine the exercise with movements of the arms or legs.
- After that, the patient should integrate the contraction of the transversus abdominis muscle in the ADL. [20]
Stretching Exercises[edit | edit source]
With a crossed leg syndrome type of problem, it’s beneficial to stretch the tightened muscles. For improving the mobility, the patient could perform stretching of the hamstrings, hip flexors, and lumbar paraspinal muscles over 15 seconds. This will improve the active and the passive ROM in the lower extremity.[17]
- Hold-relax stretching of the iliopsoas: It can reduce back pain, excessive lumbar lordosis angle, lengthen the iliopsoas and increase transversus abdominis activation capacity. The target hip is moved toward the floor until the patient feels a mild stretch sensation. Then the patient must perform a submaximal voluntary isometric contraction of the M. Iliopsoas for 10 seconds and then completely relax for 10 seconds. The participant’s leg is now slowly moved to a new range until a mild stretching sensation is felt and described by the patient. This position is then held for 20 seconds. This is repeated 5 times, followed by a 1 min rest, for 15 minutes. [21]
- Stretching technique for improving the ROM of the M.Iliopsoas and the M. Rectus femoris: The patient lies in Thomas position, the not stretched leg is maximally flexed to stabilize the pelvis and flatten the lumbar spine. The other leg is in a normal flexed position because of the tightness of the M. Iliopsoas. It’s this leg that needs to be pushed against the table. If you want to stretch the M. rectus femoris, bend the knee more than 90°, while performing the same stretch.
Stabilization Exercises[edit | edit source]
The stabilization exercises may be beneficial for reducing pain and disability. [8] Patients following a supervised spinal stabilization exercise program show higher pain reduction compared to patients following another exercise program. During external perturbation, there is a decreased anterior-posterior displacement.[22]
Sling Exercise Training[edit | edit source]
Sling exercise training seems to be effective at reducing the pain intensity and disability levels of LBP patients. The patient is suspended in a system of pulleys. He/She has to move the arms or legs, while he/she keeps the spine in a neutral position. Both the deep and superficial muscles need to contract.[20] The patient can also put only his feet in the sling while he can perform some bridging exercises.
The Swiss Ball[edit | edit source]
The exercises on the swiss ball demand contraction of the stabilizing muscles, but there is also a contraction of the rectus abdominis muscle [23]
Exercise Therapy[edit | edit source]
Exercise therapy, including supervised exercises, appears to be slightly effective at decreasing pain and improving function in adults with chronic low-back pain, particularly in healthcare populations. Patients with an acute outburst of low back pain who received exercise therapy in addition to the medical management had fewer recurrences over a long time. [1] Decreasing the extension forces on the lumbar spine must be the purpose of the exercises. This can result in a decreased lumbar lordosis. Exercises should be done on a regular basis to reach maximum effect.
Outcome Measures[edit | edit source]
- Oswestry Disability Index is the most effective for persistent severe disability. Oswestry Disability Index [24]
- Roland-Morris Disability Questionnaire is better for mild to moderate disability. Roland‐Morris Disability Questionnaire [24]
Clinical Bottom Line[edit | edit source]
In most cases, hyperlordosis is due to specific lifestyle factors. Often, maintaining a healthy weight and exercising regularly can improve issues with posture and lower back pain.
NB In some cases, hyperlordosis may be the result of other underlying spinal problems, such as kyphosis, spondylolisthesis, and discitis and these must be ruled out if problems persist or red flags evident.[25]
References[edit | edit source]
- ↑ Czaprowski D, Stoliński Ł, Tyrakowski M, Kozinoga M, Kotwicki T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis and spinal disorders. 2018 Dec 1;13(1):6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5836359/ (last accessed 10.12.2019)
- ↑ Been, Ella, and Leonid Kalichman. "Lumbar lordosis." The Spine Journal 2014; 14.1: 87-97.
- ↑ 3.0 3.1 González-Gálvez N, Gea-García GM, Marcos-Pardo PJ. Effects of exercise programs on kyphosis and lordosis angle: A systematic review and meta-analysis. PloS one. 2019 Apr 29;14(4):e0216180. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6488071/ (last accessed 12.12.2019)
- ↑ Bogduk, Nikolai. “Clinical anatomy of the lumbar spine and sacrum”. Elsevier Health Sciences, 2005
- ↑ 5.0 5.1 Polly Jr, David W., et al. "Measurement of lumbar lordosis: evaluation of intraobserver, interobserver, and technique variability." Spine 21.13 (1996): 1530-1535.
- ↑ Hanson P, Magnusson SP, Simonsen EB. Differences in sacral angulation and lumbosacral curvature in black and white young men and women. Acta Anat (Basel). 1998;162(4):226-31. doi: 10.1159/000046437. PMID: 9831771.
- ↑ Mosner EA, Bryan JM, Stull MA, Shippee R. A comparison of actual and apparent lumbar lordosis in black and white adult females. Spine (Phila Pa 1976). 1989 Mar;14(3):310-4. doi: 10.1097/00007632-198903000-00011. PMID: 2711246.
- ↑ 8.0 8.1 Gomes-Neto, Mansueto, et al. "Stabilization exercise compared to general exercises or manual therapy for the management of low back pain: A systematic review and meta-analysis." Physical Therapy in Sport (2016).
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Fatemi, Rouholah, Marziyeh Javid, and Ebrahim Moslehi Najafabadi. "Effects of William training on lumbosacral muscles function, lumbar curve and pain." Journal of back and musculoskeletal rehabilitation 2015; 28.3: 591-597.
- ↑ Nourbakhsh, Mohammad Reza, and Amir Massoud Arab. "Relationship between mechanical factors and incidence of low back pain." Journal of Orthopaedic & Sports Physical Therapy 32.9 (2002): 447-460.
- ↑ 11.0 11.1 Kim, Ho-Jun, et al. "Influences of trunk muscles on lumbar lordosis and sacral angle." European Spine Journal 15.4 (2006): 409-414.
- ↑ Laird RA, Gilbert J, Kent P, Keating JL. Comparing lumbo-pelvic kinematics in people with and without back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2014 Jul 10;15:229. doi: 10.1186/1471-2474-15-229. PMID: 25012528; PMCID: PMC4096432.[1]
- ↑ Physiotherapy and recovery Lumbar Lordosis. Available from: https://beyutza.wordpress.com/2014/02/16/lumbar-lordosis/ (last accessed 12.12.2019)
- ↑ Bryan, Jean M., et al. "Investigation of the Flexible Ruler as a Noninvasive Measure of Lumbar Lordosis in Black and White Adult Female Sample Populations*." Journal of Orthopaedic & Sports Physical Therapy 11.1 (1989): 3-7.
- ↑ J Ethier Fix "Anterior Pelvic Tilt" in 10 Minutes/Day (Daily Exercise Routine) Available from: https://www.youtube.com/watch?v=2NZMaI-HeNU (last accessed 12.12.2019)
- ↑ Wong, J. J., et al. "Clinical practice guidelines for the noninvasive management of low back pain: A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration." European Journal of Pain (2016).
- ↑ 17.0 17.1 Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005 May 3;142(9):776-85. doi: 10.7326/0003-4819-142-9-200505030-00014. PMID: 15867410.
- ↑ 18.0 18.1 Hodges PW. Core stability exercise in chronic low back pain. Orthop Clin North Am 2003;34:245-254. Barr KP, Griggs M, Cadby T. Lumbar stabilization: core concepts and current literature, Part 1. Am J Phys Med Rehabil 2005;84:473-480.
- ↑ Byström, Martin Gustaf, Eva Rasmussen-Barr, and Wilhelmus Johannes Andreas Grooten. "Motor control exercises reduces pain and disability in chronic and recurrent low back pain: a meta-analysis." Spine 38.6 (2013): E350-E358.
- ↑ 20.0 20.1 Unsgaard-Tøndel, Monica, et al. "Motor control exercises, sling exercises, and general exercises for patients with chronic low back pain: a randomized controlled trial with 1-year follow-up." Physical therapy 90.10 (2010): 1426-1440.
- ↑ Malai, Suthichan, Sopa Pichaiyongwongdee, and Prasert Sakulsriprasert. "Immediate Effect of Hold-Relax Stretching of Iliopsoas Muscle on Transversus Abdominis Muscle Activation in Chronic Non-Specific Low Back Pain with Lumbar Hyperlordosis." J Med Assoc Thai 2015; 98 (Suppl. 5): S6-S11.
- ↑ Rhee, Hyun Sill, Yoon Hyuk Kim, and Paul S. Sung. "A randomized controlled trial to determine the effect of spinal stabilization exercise intervention based on pain level and standing balance differences in patients with low back pain." Medical Science Monitor 18.3 (2012): CR174-CR189.
- ↑ Marshall, Paul W., and Bernadette A. Murphy. "Core stability exercises on and off a Swiss ball." Archives of physical medicine and rehabilitation 86.2 (2005): 242-249.
- ↑ 24.0 24.1 Davies, Claire C., and Arthur J. Nitz. "Psychometric properties of the Roland-Morris Disability Questionnaire compared to the Oswestry Disability Index: a systematic review." Physical therapy reviews 2013; 14.6: 399-408
- ↑ Medical news today Lumbar lordosis Available from: https://www.medicalnewstoday.com/articles/321959.php (last accessed 12.12.2019)