Overview of Cervical Spine Assessment
Top Contributors - Jacquie Kieck, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Neck pain is one of the most common musculoskeletal conditions with a high personal and economic burden.[1][2] Clinicians will often encounter patients with neck pain and other cervical spine conditions. It is, therefore, essential that they can confidently perform a thorough assessment of the cervical spine. This page provides a step-by-step overview of the key elements of the cervical spine evaluation, including the subjective assessment (history taking) and the objective assessment (observation and tests). It also introduces the Proposed Classification System for the Cervical Spine.
Subjective Assessment[edit | edit source]
History[edit | edit source]
The mnemonic L-M-N-O-P-Q-R-S-T can be used to cover the key aspects you should consider when taking a patient’s history.
L: Location of symptoms and level of functional impairment
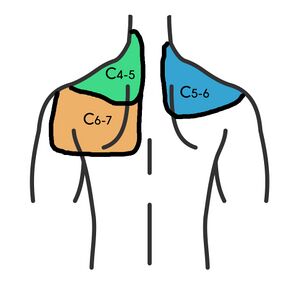
This table summarises the likely source of symptoms based on the area of symptoms.
| Area of Symptoms | Possible Source of Symptoms |
|---|---|
| Head / occipital region | Upper cervical spine |
| Localised pain without radiation / referral |
|
| Radiating pain | Nerve root irritation |
M: Medical factors (medications) and mechanism of injury
In the assessment, find out exactly when and how the injury occurred, what forces were applied, and the position of the head at the time of the trauma. Also, ask about any neurological symptoms associated with the trauma.
Red flag symptoms related to the mechanism of injury: sudden onset of severe pain in the absence of an incident or accident.
N: Neurological examination
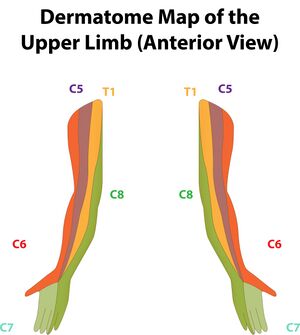
A neurological examination is performed to establish neurologic function and to help form a diagnosis.[4] It is important to establish if the patient has numbness, tingling, burning or electrifying symptoms, as these symptoms indicate neurologic involvement. Be specific about the location of these symptoms, i.e. is the distribution of these symptoms dermatomal? The clinician should also note if the symptoms are constant or intermittent and if they are associated with the position of the head.
O: Occupation, including limitations
Establish if there are any work- or activity-related factors that are relevant.
P: Palliating and provocating symptoms
Establish what increases and decreases the symptoms. Also, note how long it takes for symptoms to calm down once aggravated.
Red flag symptom: constant/unrelenting pain independent of position or activity.
Q: Quality of symptoms/pain
Consider the description of symptoms. Are symptoms described as sharp, dull, stabbing, aching or electric / shock-like?
R: Radiation of symptoms
Be specific about where the symptoms radiate to, how long the radiating symptoms last, and whether they are constant or position / activity related.
Red flag symptom: radiating symptoms that cover multiple dermatomes.
S: Severity of symptoms
Note how symptoms impact function and activity.
T: Timing of symptoms
Ask about the sequence and progression of symptoms.
Red flag symptoms: pain is interrupting sleep or constant / unrelenting pain.
Be sure to check the patient's age and include questions about history of neck pain, constitutional symptoms (i.e. dizziness / lightheadedness, drop attacks and vertigo), paraesthesia, numbness, weakness, or stiffness.
Red Flags[edit | edit source]
Red flags are symptoms that suggest the presence of serious pathology. International guidelines recommend using red flags to identify serious pathology.[5] Below is a list of red flags to screen when assessing the cervical spine:
- severe loss of range of motion (ROM) with sudden onset of symptoms
- changes in balance / gait
- hyporeflexia/hyperreflexia
- constant pain
- severe radiating pain
- moderate to severe occipital headache
- facial pain
- psychological changes
- cranial nerve symptoms
- dizziness
- Horner's syndrome
- hemiparaesthesia
- bowel and bladder changes
- ataxia
- nystagmus
- drop attacks
- hemifacial paraesthesia
- dysphagia
The History can be Suggestive of Certain Conditions[edit | edit source]
History suggesting cervical spondylosis[edit | edit source]
A history suggestive of cervical spondylosis would include a person over the age of 45 years with gradual, slow onset of symptoms (no specific incident). The pain is usually unilateral and radiates in a facet joint referral pattern. Pain usually increases with extension ('closing down' of the joint) and reduces with flexion ('opening' of the joint). The most commonly affected cervical spine levels are C5, C6 and C7.[6][3]
History suggesting disc involvement[edit | edit source]
A history suggestive of cervical disc involvement would include a person under the age of 60 years, with sudden onset of symptoms. Symptoms may be associated with a specific incident, such as a motor vehicle accident, or simply moving "strangely". Pain is usually unilateral and radiates in a dermatomal referral pattern. Pain usually increases with flexion. Tingling and other neurological symptoms may be present. The most commonly affected levels of the cervical spine are C5 and C6.[6]
Self-Assessment Questionnaires[edit | edit source]
Useful self-assessment questionnaires in the assessment of the cervical spine include:
- Neck Disability Index (NDI)[7][8]
- Patient Specific Functional Scale (PSFS)[8]
- Fear-Avoidance Belief Questionnaire (FABQ)[9]
- Numeric Pain Rating Scale (NPRS)[7][8]
Objective Assessment[edit | edit source]
Observation[edit | edit source]
It is important to complete a general observation of posture, including the head, neck, and shoulder position. Also, observe for any signs of torticollis.
Instability Testing[edit | edit source]
The Sharp-Purser Test is used to assess the integrity of the transverse ligament. However, there are concerns about the reliability, validity, and safety of this test.[10] See the video below for a demonstration of the Sharp-Purser Test.
Vertebral Artery Testing[edit | edit source]
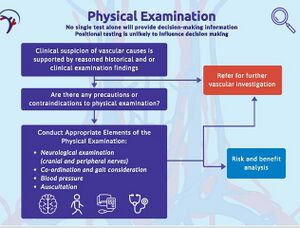
Symptoms of vertebral insufficiency include dizziness/vertigo, nausea/vomiting, inability to stand, blurred vision/diplopia, headache, facial paraesthesia/facial palsy/difficulty swallowing.[12]
Following a thorough subjective assessment of the cervical spine, clinicians should carefully plan the physical examination and consider any precautions and contraindications related to vertebral insufficiency.
In addition, the clinician should reflect on their ability to perform certain tests and seek additional training if needed.[12]
The following tests can be included for the assessment of vertebral artery insufficiency:[6]
- Hautant Test
- Cervical Quadrant Test
- Pre-manipulative Position Test
Canadian C-Spine Rule[edit | edit source]
The Canadian C-Spine Rule is a decision-making tool used to determine when radiography should be utilised in patients following trauma. This tool has a very low negative likelihood ratio. This means that if you get a negative finding for the test, there is only a very small chance that the patient would still have the condition (i.e. for the Canadian C-Spine Rule, that the patient would still need a radiograph).[13][6]
Functional Screening[edit | edit source]
Typically, a functional screen will include a chin tuck action, cervical flexion, extension and rotation, and shoulder movements.
Palpation[edit | edit source]
Palpation includes palpation of the relevant musculature of the cervical spine, namely the trapezius, sternocleidomastoid, suboccipital muscles, and the scalene muscles. Also include palpation of the spinous processes and facet joints.
Range of Motion[edit | edit source]
When assessing range of motion of the cervical spine, take note of symptoms associated with the movements. Generally, over-pressure is not applied when testing the range of motion of the cervical spine, as the weight of the head is sufficient for testing.
Muscle Testing[edit | edit source]
Neck pain is often associated with weakness of the cervical deep neck flexors, which results in a lack of endurance and decreased ability to hold the neck in position.[14] The Deep Cervical Flexion Test (also known as the Cranial Cervical Flexion Test) and neck flexor endurance testing can be performed to assess the strength and endurance of the deep neck flexors.
Neurological Testing[edit | edit source]
A neurological screen includes testing of reflexes, dermatomes and myotomes. It is important to also include a cranial nerve screen and upper limb tension tests (i.e. neurodynamic testing).
Joint Mobility Testing[edit | edit source]
Passive physiological intervertebral mobility testing, passive intervertebral testing and intervertebral glides are included in the cervical spine evaluation to assess joint mobility.
Special Tests[edit | edit source]
- Cervical Compression Test:
- pain with this test may indicate an intervertebral disc issue, vertebral fracture, or nerve root irritation (if there are radiating symptoms)
- this test can be modified to stress specific tissues; applying compression with the neck in a more flexed position will stress the disc and vertebral body while applying compression with the neck in a more extended position will stress the facet joint and the nerve as it exits the formina
- Cervical Distraction Test:
- decreased pain with distraction may indicate disc pathology, nerve root compression or facet joint pathology
- Spurling's A Test[16][17]
- this test is used when looking for cervical nerve root compression causing cervical radiculopathy
- the test has a good specificity, but a low sensitivity, and is most useful when used in conjunction with other tests
- Test Item Cluster:
- when combined, a test item cluster of Spurling's Test, Upper Limb Tension Test 1, Cervical Distraction Test and Cervical Rotation Test has high diagnostic accuracy when compared to EMG studies[18]
- Shoulder Abduction Test or Bakody Sign
- this test was designed to assess radicular pain - it can suggest cervical nerve involvement, but is not diagnostic
- the client is asked to place the affected extremity on their head. If symptoms reduce, the test is positive
Classification of Cervical Spine Pain[edit | edit source]
A classification system identifies groups with common characteristics. Classification systems help to determine the intervention(s) that would produce optimal clinical outcomes within specific groups.[6] Fritz et al.[19] found that when subjects were matched to interventions using the Proposed Treatment-Based Classification System, they had greater disability reduction than those unmatched to interventions.[19]
| Classification | Key Feature | Examination Findings | Intervention Focus |
|---|---|---|---|
| Neck pain with mobility deficits | Mobility |
|
|
| Neck pain with radiating pain | Centralisation |
|
|
| Neck pain with movement coordination impairments | Conditioning exercise |
|
|
| Neck pain | Pain |
|
|
| Neck pain with headache | Headache |
|
|
Resources[edit | edit source]
- International Framework for Examination of the Cervical Region for potential of vascular pathologies of the neck prior to Orthopaedic Manual Therapy (OMT) Intervention: International IFOMPT Cervical [12]
References[edit | edit source]
- ↑ Safiri S, Kolahi AA, Hoy D, Buchbinder R, Mansournia MA, Bettampadi D, et al. Global, regional, and national burden of neck pain in the general population, 1990-2017: systematic analysis of the Global Burden of Disease Study 2017. BMJ. 2020 Mar 26;368:m791.
- ↑ Kazeminasab S, Nejadghaderi SA, Amiri P, Pourfathi H, Araj-Khodaei M, Sullman MJM, et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 2022 Jan 3;23(1):26.
- ↑ 3.0 3.1 Hurley RW, Adams MCB, Barad M, Bhaskar A, Bhatia A, Chadwick A, et al. Consensus practice guidelines on interventions for cervical spine (facet) joint pain from a multispecialty international working group. Regional Anesthesia & Pain Medicine [Internet]. 2021 Nov 7 [cited 2022 Jan 20];47(1).
- ↑ Shahrokhi M, Asuncion RM. Neurologic exam. InStatPearls [Internet] 2022 Jan 20. StatPearls Publishing.
- ↑ Childs, J.D., Cleland, J.A., Elliott, J.M., Teyhen, D.S., Wainner, R.S., Whitman, J.M., Sopky, B.J., Godges, J.J., Flynn, T.W., Delitto, A. and Dyriw, G.M. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. Journal of Orthopaedic & Sports Physical Therapy. 2008; 38(9):A1-A34.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Cunningham, S. An Overview of Cervical Spine Assessment. Course. Plus. 2023.
- ↑ 7.0 7.1 Cleland JA, Childs JD, Whitman JM. Psychometric Properties of the neck disability index and numeric pain rating scale in patients with mechanical neck pain. Archives of Physical Medicine and Rehabilitation. 2008;89(1):69–74.
- ↑ 8.0 8.1 8.2 Basson CA, Olivier B, Rushton A. Neck pain in South Africa: An overview of the prevalence, assessment and management for the Contemporary Clinician. South African Journal of Physiotherapy. 2019;75(1).
- ↑ Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–68.
- ↑ Mansfield CJ, Domnisch C, Iglar L, Boucher L, Onate J, Briggs M. Systematic review of the diagnostic accuracy, reliability, and safety of the sharp-purser test. Journal of Manual & Manipulative Therapy. 2019;28(2):72–81.
- ↑ The Student Physical Therapist. Sharp-Purser Test. Available from: https://www.youtube.com/watch?v=j_qFxxCq7fY [last accessed 25/1/2024]
- ↑ 12.0 12.1 12.2 Rushton A, Carlesso LC, Flynn T, Hing WA, Rubinstein SM, Vogel S, et al. International Framework for examination of the cervical region for potential of vascular pathologies of the neck prior to musculoskeletal intervention: International IFOMPT cervical framework. Journal of Orthopaedic & Sports Physical Therapy. 2023;53(1):7–22.
- ↑ Michaleff ZA, Maher CG, Verhagen AP, Rebbeck T, Lin C-WC. Accuracy of the Canadian C-spine rule and nexus to screen for clinically important cervical spine injury in patients following Blunt Trauma: A systematic review. Canadian Medical Association Journal. 2012;184(16).
- ↑ Kamayoga ID, Adyasputri AA, Putra IP, Widnyana M, Utama AA. The efficacy of deep cervical flexor training with feedback reducing pain and disability in individuals with work-related Neck Pain. Physical Therapy Journal of Indonesia. 2021;2(2):50–3.
- ↑ Cranial Nerve Examination | OSCE Guide | NEW. Available from: https://www.youtube.com/watch?v=yZ5kV7dJoZw[last accessed 25/1/2024]
- ↑ Rubinstein SM, Pool JJ, van Tulder MW, Riphagen II, de Vet HC. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J. 2007; 16: 307-319.
- ↑ Kang KC, Lee HS, Lee JH. Cervical Radiculopathy Focus on Characteristics and Differential Diagnosis. Asian Spine Journal [Internet]. 2020 Dec 1;14(6):921–30. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7788378/
- ↑ Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine 2003; 28(1):52-62.
- ↑ 19.0 19.1 Fritz JM, Brennan GP. Preliminary Examination of a Proposed Treatment-Based Classification System for Patients Receiving Physical Therapy Interventions for Neck Pain. Physical Therapy. 2007 May 1;87(5):513–24.