Wound Healing: Difference between revisions
No edit summary |
No edit summary |
||
| Line 13: | Line 13: | ||
* Begins immediately after an injury to the epidermal layer and might take years. | * Begins immediately after an injury to the epidermal layer and might take years. | ||
* Dynamic process including highly organized cellular, humoral, and molecular mechanisms. | * Dynamic process including highly organized cellular, humoral, and molecular mechanisms. | ||
* Has 3 overlapping phases which are inflammation, proliferation, and remodeling. Any disruption leads to abnormal wound healing<ref>Kangal MK, Regan JP. Issues of Concern.2020 Available from:https://www.ncbi.nlm.nih.gov/books/NBK535406/ (last accessed 24.10.2020)</ref>. | * Has 3 overlapping phases which are inflammation, proliferation, and remodeling. Any disruption leads to abnormal wound healing<ref name=":3">Kangal MK, Regan JP. Issues of Concern.2020 Available from:https://www.ncbi.nlm.nih.gov/books/NBK535406/ (last accessed 24.10.2020)</ref>. | ||
== Types of wound == | == Types of wound == | ||
| Line 32: | Line 32: | ||
== Wound Healing stages in Adults == | == Wound Healing stages in Adults == | ||
In adults, optimal wound healing should involve four continuous and overlapping phases: '''hemostasis, inflammation, proliferation, and remodeling''' .<ref name=":0">David J Magee, James E. Zachazewski, and William S. Quillen,Pathology and intervention of muscloskeletal disorders.2nd ed,2008.</ref> | [[File:4-STAGES-OF-WOUND-HEALING.png|right|frameless|801x801px]]In adults, optimal wound healing should involve four continuous and overlapping phases: '''hemostasis, inflammation, proliferation, and remodeling''' .<ref name=":0">David J Magee, James E. Zachazewski, and William S. Quillen,Pathology and intervention of muscloskeletal disorders.2nd ed,2008.</ref> | ||
# '''Hemostasis Phase''' - the process of the wound being closed by clotting. | |||
* Happens very quickly. | |||
* Starts when blood leaks out of the body, then blood vessels constrict to restrict the blood flow. | |||
* The platelets aggregate and adhere to the sub-endothelium surface within seconds of the rupture of a blood vessel's epithelial wall. | |||
* After that, the first fibrin strands begin to adhere in about sixty seconds. | |||
* As the fibrin mesh begins, the blood is transformed from liquid to gel through pro-coagulants and the release of prothrombin. | |||
* The formation of a thrombus or clot keeps the platelets and blood cells trapped in the wound area. | |||
* The thrombus is generally important in the stages of wound healing but becomes a problem if it detaches from the vessel wall and goes through the circulatory system, possibly causing a stroke, pulmonary embolism or heart attack<ref name=":3" />. | |||
2. I'''nflammatory Phase''' | |||
* Begins right after the injury when the injured blood vessels leak transudate (made of water, salt, and protein) causing localized swelling. | |||
* Inflammation both controls bleeding and prevents infection. | |||
* The fluid engorgement allows healing and repair cells to move to the site of the wound. | |||
* During the inflammatory phase, damaged cells, pathogens, and bacteria are removed from the wound area. | |||
* These white blood cells, growth factors, nutrients and enzymes create the swelling, heat, pain and redness commonly seen during this stage of wound healing. | |||
* Inflammation is a natural part of the wound healing process and only problematic if prolonged or excessive. | |||
The | 3. '''Proliferative Phase''' - when the wound is rebuilt with new tissue made up of collagen and extracellular matrix. | ||
* The wound contracts as new tissues are built. | |||
* A new network of blood vessels must be constructed so that the granulation tissue can be healthy and receive sufficient oxygen and nutrients. | |||
* Myofibroblasts cause the wound to contract by gripping the wound edges and pulling them together using a mechanism similar to that of smooth muscle cells. | |||
* In healthy stages of wound healing, granulation tissue is pink or red and uneven in texture. Healthy granulation tissue does not bleed easily. | |||
* Dark granulation tissue can be a sign of infection, ischemia, or poor perfusion. | |||
* Finally epithelial cells resurface the injury. | |||
* Epithelialization happens faster when wounds are kept moist and hydrated. | |||
* Generally, when occlusive or semiocclusive dressings are applied within 48 hours after injury, they will maintain correct tissue humidity to optimize epithelialization. | |||
4. '''Maturation Phase''' (remodeling stage) | |||
* Collagen is remodeled from type III to type I and the wound fully closes. | |||
* The cells that had been used to repair the wound but which are no longer needed are removed by apoptosis, or programmed cell death. | |||
* The collagen laid down during the proliferative phase, it is disorganized and the wound is thick. | |||
* [[Collagen]] is remodeled into a more organized structure along lines of stress, thereby increasing the tensile strength of the healing tissues. Fibroblasts secrete matrix metalloproteinases. The enzymes facilitate remodeling of type III collagen to type I collagen.<ref name=":0" /> | |||
* Generally, remodeling begins about 21 days after an injury and can continue for a year or more. | |||
* Even with cross-linking, healed wound areas continue to be weaker than uninjured skin, generally only having 80% of the tensile strength of unwounded skin<ref name=":3" />. | |||
[[Collagen]] is remodeled into a more organized structure along lines of stress, thereby increasing the tensile strength of the healing tissues. Fibroblasts secrete matrix metalloproteinases. The enzymes facilitate remodeling of type III collagen to type I collagen, | |||
== Factors affecting the wound healing == | == Factors affecting the wound healing == | ||
'''Intrinsic factors''' include :age, nutrition, and hydration levels, location and depth of the wound, medications, and co-morbidities. | '''Intrinsic factors''' include :age, nutrition, and hydration levels, location and depth of the wound, medications, and co-morbidities. | ||
Revision as of 07:36, 24 October 2020
Original Editor - Esraa Mohamed Abdullzaher
Top Contributors - Esraa Mohamed Abdullzaher, Naomi O'Reilly, Lucinda hampton, Kim Jackson, Olajumoke Ogunleye, Joao Costa, Claire Knott, Admin, Lauren Lopez and Aya Alhindi
Introduction[edit | edit source]
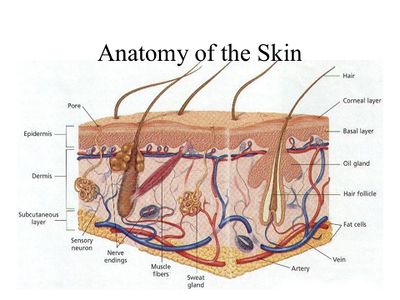
Skin is the largest organ in the body and covers the body's entire external surface.
- Made up of three layers, the epidermis, dermis, and the hypodermis.
- Skin's structure is made up of an intricate network which serves as the body’s initial barrier against pathogens, UV light, and chemicals, and mechanical injury, and regulates temperature and the amount of water released into the environment.
A skin wound results from the breakdown of the epidermal layer integrity[1].
- Wound healing mostly means healing of the skin.
- Begins immediately after an injury to the epidermal layer and might take years.
- Dynamic process including highly organized cellular, humoral, and molecular mechanisms.
- Has 3 overlapping phases which are inflammation, proliferation, and remodeling. Any disruption leads to abnormal wound healing[2].
Types of wound[edit | edit source]
Wounds can be separated into open or closed wounds.
- Closed wound: the surface of the skin is intact, but the underlying tissues may be damaged. eg contusions, hematomas, or stage 1 pressure ulcers.
- Open wounds: the skin is split or cracked, and the underlying tissues are exposed to the outside environment.
Types of Wound healing[edit | edit source]
Wound healing is classified as primary healing and secondary healing.
Primary Healing
- Uncomplicated healing of a noninfected, well-approximated wound is defined as primary healing. eg Surgical wounds.
Secondary healing
- If the wound healing course in this wound is disrupted by infection, dehiscence, hypoxia or immune dysfunction, secondary healing stage begins.
- During secondary healing, granulation tissue formation and epithelization over this new tissue take place. These type of wounds are more susceptible to infections and poor healing.
Wound Healing stages in Adults[edit | edit source]
In adults, optimal wound healing should involve four continuous and overlapping phases: hemostasis, inflammation, proliferation, and remodeling .[3]
- Hemostasis Phase - the process of the wound being closed by clotting.
- Happens very quickly.
- Starts when blood leaks out of the body, then blood vessels constrict to restrict the blood flow.
- The platelets aggregate and adhere to the sub-endothelium surface within seconds of the rupture of a blood vessel's epithelial wall.
- After that, the first fibrin strands begin to adhere in about sixty seconds.
- As the fibrin mesh begins, the blood is transformed from liquid to gel through pro-coagulants and the release of prothrombin.
- The formation of a thrombus or clot keeps the platelets and blood cells trapped in the wound area.
- The thrombus is generally important in the stages of wound healing but becomes a problem if it detaches from the vessel wall and goes through the circulatory system, possibly causing a stroke, pulmonary embolism or heart attack[2].
2. Inflammatory Phase
- Begins right after the injury when the injured blood vessels leak transudate (made of water, salt, and protein) causing localized swelling.
- Inflammation both controls bleeding and prevents infection.
- The fluid engorgement allows healing and repair cells to move to the site of the wound.
- During the inflammatory phase, damaged cells, pathogens, and bacteria are removed from the wound area.
- These white blood cells, growth factors, nutrients and enzymes create the swelling, heat, pain and redness commonly seen during this stage of wound healing.
- Inflammation is a natural part of the wound healing process and only problematic if prolonged or excessive.
3. Proliferative Phase - when the wound is rebuilt with new tissue made up of collagen and extracellular matrix.
- The wound contracts as new tissues are built.
- A new network of blood vessels must be constructed so that the granulation tissue can be healthy and receive sufficient oxygen and nutrients.
- Myofibroblasts cause the wound to contract by gripping the wound edges and pulling them together using a mechanism similar to that of smooth muscle cells.
- In healthy stages of wound healing, granulation tissue is pink or red and uneven in texture. Healthy granulation tissue does not bleed easily.
- Dark granulation tissue can be a sign of infection, ischemia, or poor perfusion.
- Finally epithelial cells resurface the injury.
- Epithelialization happens faster when wounds are kept moist and hydrated.
- Generally, when occlusive or semiocclusive dressings are applied within 48 hours after injury, they will maintain correct tissue humidity to optimize epithelialization.
4. Maturation Phase (remodeling stage)
- Collagen is remodeled from type III to type I and the wound fully closes.
- The cells that had been used to repair the wound but which are no longer needed are removed by apoptosis, or programmed cell death.
- The collagen laid down during the proliferative phase, it is disorganized and the wound is thick.
- Collagen is remodeled into a more organized structure along lines of stress, thereby increasing the tensile strength of the healing tissues. Fibroblasts secrete matrix metalloproteinases. The enzymes facilitate remodeling of type III collagen to type I collagen.[3]
- Generally, remodeling begins about 21 days after an injury and can continue for a year or more.
- Even with cross-linking, healed wound areas continue to be weaker than uninjured skin, generally only having 80% of the tensile strength of unwounded skin[2].
Factors affecting the wound healing[edit | edit source]
Intrinsic factors include :age, nutrition, and hydration levels, location and depth of the wound, medications, and co-morbidities.
Extrinsic factors include: support surfaces, friction, and shear and effective repositioning schedules.
also there are other local factors like :[4]
- Moisture; keeping a wound moist rather than dry makes wound healing more rapid and with less pain and less scarring
- Mechanical factors
- Edema
- Ionizing radiation
- Faculty technique of wound closure
- Ischemia and necrosis
- Foreign bodies.
- Low oxygen tension
- Perfusion
and another systemic factors:
- Inflammation
- Diabetes .
- Nutrients.
- Metabolic diseases.
- Immunosuppression.
- Connective tissue disorders.
- Smoking.
- Alcohol .
Complications of wound healing[edit | edit source]
- Deficient scar formation.
- Excessive scar formation:
- Exuberant granulation.
- Deficient contraction (in skin grafts) or excessive contraction (in burns).
- Others: Dystrophic calcification, pigmentary changes, painful scars, incisional hern.[4]
Wound care in Physiotherapy[edit | edit source]
The most common wounds that are treated by wound care physical therapist are:[5]
- Necrotic wounds.
- Stage III, IV or unstageable pressure ulcers.
- Diabetic wounds.
- Chronic wounds.
- Venous and/or arterial wounds.
- Extremity wounds with edema.
- Non-healing surgical wounds.
Physiotherapy role[edit | edit source]
Patients must be referred by their physician to physical therapy wound care.Physical therapy wound care begins with a comprehensive evaluation and development of an individualized care plan. [5]
Common treatment approaches can include:
- Measurement and documentation of the wound characteristics
- Cleaning of the wound
- Debridement (removal) of any dead tissue
- Selection and application of wound dressing
- Application of compression if necessary
- Education of the patient, caregivers and/or family members regarding wound care and dressing changes.
and the available treatment modalities may include:
- Ultrasound mist therapy
- Electrical stimulation
- Pulsed lavage
- Whirlpool
- Negative pressure vacuum therapy
- Compression therapy.
Related Resources[edit | edit source]
References[edit | edit source]
- ↑ Yousef H, Alhajj M, Sharma S. Anatomy, skin (integument), epidermis.2017 Available from:https://www.ncbi.nlm.nih.gov/books/NBK470464/ (last accessed 24.10.2020)
- ↑ 2.0 2.1 2.2 Kangal MK, Regan JP. Issues of Concern.2020 Available from:https://www.ncbi.nlm.nih.gov/books/NBK535406/ (last accessed 24.10.2020)
- ↑ 3.0 3.1 David J Magee, James E. Zachazewski, and William S. Quillen,Pathology and intervention of muscloskeletal disorders.2nd ed,2008.
- ↑ 4.0 4.1 https://en.wikipedia.org/wiki/Wound_healing
- ↑ 5.0 5.1 https://my.clevelandclinic.org/departments/rehabilitation/services/wound-care