Therapeutic Alliance
Original Editor - Laura Ritchie, posting on behalf of Wei Seah, MPT Class of 2017 at Western University, project for PT9584.
Top Contributors - Laura Ritchie, Ewa Jaraczewska, Kim Jackson, Mandy Roscher, Wanda van Niekerk, Robin Tacchetti, Naomi O'Reilly, Jess Bell, Evan Thomas and Vidya Acharya
Introduction[edit | edit source]
The therapeutic alliance (also referred to as the working alliance) is a description of the interaction between the physiotherapist and their patients. By establishing a therapeutic alliance, the therapist then seeks to provide patient-centered care, in which the therapist as seen as a facilitator for the patient to achieve their goals, rather than an authority figure.[1] Previous research has highlighted the importance of providing patient-centered care not only in physiotherapy, but other medical professions as well. [2] This is accomplished by encouraging the patient to become more active in their treatment to engage them in a collaborative, active approach to recovery.[3] By establishing a strong therapeutic alliance and encouraging patient participation, therapists can also seek to address psychosocial aspects of pain, [4] which are often overlooked in traditional unidirectional patient-therapist interactions. This is especially important as recent research supports that the physical treatment alone cannot fully account for improvement of patient outcomes. [5]
| [6] |
Background[edit | edit source]
The therapeutic alliance was first described by Freud in 1912, in which he outlined the concepts of transference and countertransference, which are the unconscious feelings or emotions that a patient feels towards their therapist, and vice-versa. [7] Further research by Rogers (1951) was the first to highlight empathy as a core characteristic of this therapeutic alliance and Anderson (1962) conceptualized both empathy and rapport as qualities within the “therapeutic bond”.[8] [9] Hougaard (1994) consolidated previous data into a conceptual structure composed of two branches, the personal relationship area and the collaborative area. [10]The personal relationship area focuses on the socio-emotional aspect of the therapist-patient relationship, while the collaborative relationship area consists of more task-related aspects, such as goal-setting and treatment planning. It was Martin, Garske and Davis (2000) concretely described the therapeutic alliance as “…the collaborative and affective bond between therapist and patient – is an essential element of the therapeutic process.” [11]
Establishing a Therapeutic Alliance[edit | edit source]
Good communicative skills are an integral tool to achieving a strong therapeutic alliance and research has shown that effective communication also leads to increased patient adherence and satisfaction. [12] Mead and Bower (2000) [2] identified five key dimensions of patient-centered care which have been associated with a positive therapeutic alliance: [13]
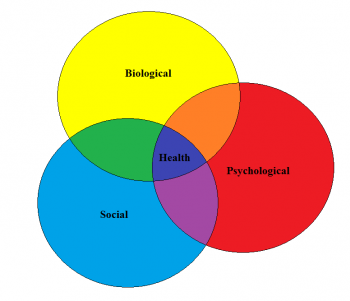
- Utilizing a biopsychosocial perspective: Several conditions treated by physical therapists appear to have little relation to structural or physiological changes, which can themselves be interpreted with high variability. [14] [15] [16] Thus, an approach that considers not only biological, but also psychological and sociological factors as well, is needed to appreciate the full scope of the problems presented and provide patient-centered care. [17]
- The ‘patient-as-person': Although the biopsychosocial model seeks to address all of the factors surrounding the patient, it may not be sufficient to fully appreciate the patient experience. [18] We need to understand that each patient may perceive the same pain experience differently and that eliciting the individual patient’s fears, expectations and feelings of illness should be one of our primary concerns [19]
- Sharing power and responsibility: The patient-practitioner relationship has always been fundamentally seen as a ‘paternalistic’ relationship, which some see as an inevitability due to the competence gap between them. [20] By shifting patients from ‘consumers’ to active ‘participants’, we can help place patients in control of their own illness, and this has been correlated with better health outcomes. [21]
- The therapeutic alliance: Just as patient-centered care can strengthen the therapeutic alliance, the reciprocal relationship can also occur. Bordin (1979) described the three main components of the therapeutic alliance as 1) agreement on goals, 2) agreement on interventions, 3) effective bond between patient and therapist. [22] The only difference is that patient-centeredness has traditionally focused on the doctor’s role, whereas the therapeutic alliance is the relationship between doctor-patient. [23] [24] In practice, the two concepts are intertwined and difficult to elicit as separate distinct components.
- The ‘doctor-as-person’: Since both the therapeutic alliance and patient-centered care acknowledge the relationship between both therapist and patient, it is thus logical to also place importance of the qualities of the therapist. The interaction between therapist and patient is constant, and the subjectivity of the therapist is something that cannot be separated from this interaction. [25]
Effect on patient outcomes[edit | edit source]
The therapeutic alliance has previously been shown to improve patient outcomes in both medicine as well as psychology. [26] [27] [28] [29] It is only recently that investigation has been made into its effects in other rehabilitative sciences. Burns and Evon (2007) studied its effect in cardiac rehabilitation and found that increased self-efficacy is not enough of a factor to predict increase cardiorespiratory fitness, weight reduction and return to work. [30] Instead, it must be combined with a strong therapeutic alliance to achieve these outcomes, and a poor therapeutic alliance can undermine the potential for improvement. Ferreira and colleagues (2012) examined the relationship between therapeutic alliance and patient outcomes on rehabilitation of patients with chronic low back pain. [31] They found that a strong therapeutic alliance leads to increased perceived changes following a variety of conservative treatments. Interestingly, a strong therapeutic alliance was associated with improved disability and function outcome measures, but not pain. Fuentes et al (2013) also conducted a study utilizing patients with low back pain, this time measuring the therapeutic alliance’s effect on pain intensity and muscle pain sensitivity. [32] The results showed that a strong therapeutic alliance can significantly modify perceived pain intensity after IFC treatments, which are displayed below. Another point of interest is the active IFC with limited therapeutic alliance was not statistically different than a sham IFC with a strong therapeutic alliance.
Measuring the therapeutic alliance[edit | edit source]
Popular outcome measures for the therapeutic alliance include the Working Alliance Theory of Change Inventory, which itself is derived from the Working Alliance Inventory. [33] Hall et al (2011) found that there was some room for improvement in the WATOCI, specifically relating to the wording in certain sections. [34] The nine items that remained were found to be a uni-dimensional tool for measuring the therapeutic alliance, despite demonstrating a ceiling effect. Due to the complexity of the therapeutic alliance it may be difficult to find a perfect measurement, however patient-administered outcomes are a step in the right direction as patient perception of the therapeutic alliance has been found to be a better predictor of outcome than therapist perception. [35]
References[edit | edit source]
- ↑ Walton D, Dhir J, Millard J. Introduction and Application of the CARE Model in Physiotherapy Practice. Presentation presented at; 2016; London, Ontario, Canada
- ↑ 2.0 2.1 Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Social Science and Medicine. 2000;51(7):1087-1110.
- ↑ Epstein R, Street R. The Values and Value of Patient-Centered Care. The Annals of Family Medicine. 2011;9(2):100-103
- ↑ Gatchel R, Peng Y, Peters M, Fuchs P, Turk D. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychological Bulletin. 2007;133(4):581-624.
- ↑ Ambady N, Koo J, Rosenthal R, Winograd C. Physical therapists' nonverbal communication predicts geriatric patients' health outcomes. Psychology and Aging. 2002;17(3):443-452.
- ↑ PsychotherapyNet. Clinical Interviewing: Intake, Assessment and Therapeutic Alliance Video. Available from: https://www.youtube.com/watch?v=ViQeF1Glz34 [last accessed 26/05/2017]
- ↑ Freud S. The Dynamics of Transference. The Standard Edition of the Complete Psychological Works of Sigmund Freud. 1912;XII (1911-1913):97-108.
- ↑ Rogers C. Client-centered therapy. 1st ed. Boston: Houghton Mifflin; 1951
- ↑ Anderson R, Anderson G. Development of an instrument for measuring rapport. The Personnel and Guidance Journal. 1962;41(1):18-24
- ↑ Hougaard E. The therapeutic alliance–A conceptual analysis. Scandinavian Journal of Psychology. 1994;35(1):67-85.
- ↑ Martin D, Garske J, Davis M. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2000;68(3):438-450
- ↑ Gyllensten A, Gard G, Salford E, Ekdahl C. Interaction between patient and physiotherapist: a qualitative study reflecting the physiotherapist's perspective. Physiotherapy Research International. 1999;4(2):89-109.
- ↑ Pinto R, Ferreira M, Oliveira V, Franco M, Adams R, Maher C et al. Patient-centred communication is associated with positive therapeutic alliance: a systematic review. Journal of Physiotherapy. 2012;58(2):77-87.
- ↑ Rogers A, Nicolaas G, Hassell K. Demanding patients?. 1st ed. Buckingham [etc.]: Open University Press; 1999
- ↑ Deyo R, Weinstein J. Low Back Pain. New England Journal of Medicine. 2001;344(5):363-370
- ↑ Herzog R, Elgort D, Flanders A, Moley P. Variability in diagnostic error rates of 10 MRI centers performing lumbar spine MRI examinations on the same patient within a 3-week period. The Spine Journal. 2017;17(4):554-561
- ↑ Silverman D. Communication and medical practice. 1st ed. Inglaterra: Sage Publications; 1987.
- ↑ Armstrong D. The emancipation of biographical medicine. Social Science and Medicine Part A: Medical Psychology and Medical Sociology. 1979;13:1-8
- ↑ Levenstein J, McCracken E, McWhinney I, Stewart M, Brown J. The Patient-Centred Clinical Method. 1. A Model for the Doctor-Patient Interaction in Family Medicine. Family Practice. 1986;3(1):24-30
- ↑ Parsons T, Smelser N. The social system. 1st ed. New Orleans, La.: Quid Pro Books; 2012
- ↑ Kaplan S, Greenfield S, Ware J. Assessing the Effects of Physician-Patient Interactions on the Outcomes of Chronic Disease. Medical Care. 1989;27(Supplement):S110-S127
- ↑ Bordin E. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research and Practice. 1979;16(3):252-260
- ↑ Lipkin M. The Medical Interview: A Core Curriculum for Residencies in Internal Medicine. Annals of Internal Medicine. 1984;100(2):277
- ↑ Smith R. The Patient's Story: Integrating the Patient- and Physician-centered Approaches to Interviewing. Annals of Internal Medicine. 1991;115(6):470
- ↑ Balint E., Courtenay M., Elder A., Hull S., Julian P. The doctor, the patient and the group: Balint re-visited. 1st ed. London: Routledge; 1993
- ↑ Kao A, Green D, Davis N, Koplan J, Cleary P. Patients’ trust in their physicians. Journal of General Internal Medicine. 1998;13(10):681-686
- ↑ Bachelor A. Comparison and relationship to outcome of diverse dimensions of the helping alliance as seen by client and therapist. Psychotherapy: Theory, Research, Practice, Training. 1991;28(4):534-549
- ↑ Barber J, Connolly M, Crits-Christoph P, Gladis L, Siqueland L. Alliance predicts patients' outcome beyond in-treatment change in symptoms. Journal of Consulting and Clinical Psychology. 2000;68(6):1027-1032
- ↑ Gaston L, Piper W, Debbane E, Bienvenu J, Garant J. Alliance and Technique for Predicting Outcome in Short-and Long-Term Analytic Psychotherapy. Psychotherapy Research. 1994;4(2):121-135
- ↑ Burns J, Evon D. Common and specific process factors in cardiac rehabilitation: Independent and interactive effects of the working alliance and self-efficacy. Health Psychology. 2007;26(6):684-692
- ↑ Ferreira P, Ferreira M, Maher C, Refshauge K, Latimer J, Adams R. The Therapeutic Alliance Between Clinicians and Patients Predicts Outcome in Chronic Low Back Pain. Physical Therapy. 2012;93(4):470-478
- ↑ Fuentes J, Armijo-Olivo S, Funabashi M, et al. Enhanced therapeutic alliance modulates pain intensity and muscle pain sensitivity in patients with chronic low back pain: an experimental controlled study. Phys Ther. 2013;94:477-489
- ↑ Horvath A, Greenberg L. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36(2):223-233
- ↑ Hall A, Ferreira M, Clemson L, Ferreira P, Latimer J, Maher C. Assessment of the therapeutic alliance in physical rehabilitation: a RASCH analysis. Disability and Rehabilitation. 2011;34(3):257-266
- ↑ Castonguay L, Constantino M, Holtforth M. The working alliance: Where are we and where should we go?. Psychotherapy: Theory, Research, Practice, Training. 2006;43(3):271-279