Tension Headaches: Difference between revisions
| Line 64: | Line 64: | ||
== Systemic Involvement == | == Systemic Involvement == | ||
Gastrointestinal (GI) involvement is a common side effect of the drugs which are most often used to treat tension-type headaches (14). These side effects include: GI ulcers, abdominal pain, upset stomach, cramping, nausea, diarrhea, heartburn, bleeding, bloating, constipation, and gas. Another possible side effect of these drugs is symptoms of the headache can worsen. This is most often seen when headaches are severe and an individual overuses the drug. If an individual experience these or any other symptoms after taking medication for a tension-type headache, then they should seek medical attention. | |||
== Medical Management (current best evidence) == | == Medical Management (current best evidence) == | ||
Revision as of 18:53, 12 April 2017
Original Editors - Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Grite Apanaviciute, Simisola Ajeyalemi, Jacquelyn Brockman, Vidya Acharya, Eugenie Lamprecht, Elaine Lonnemann and WikiSysop
Definition/Description[edit | edit source]
Tension-type headaches (TTH) are the most common type benign headache. They can affect all aspects of one’s life including work, school, and home life (1). TTH may result in disability, missed workdays, and decreased quality of life (2). They are characterized by how often an individual experience them in a given month. If an individual experiences tension-type headaches 14 or less days out of a month then it is considered episodic. If they experience these headaches 15 or more days out of a month for 3 consecutive months, then they are considered to be chronic. The etiology behind these headaches is still unknown. It is believed that changes in levels of neurotransmitters may be a contributing factor.
Prevalence[edit | edit source]
Episodic tension type headaches (TTH) are the most prevalent type of headache. Research has found that approximately 38% of individual’s experience TTHs in a given year (1,2,3). In Denmark, it was found that 78% of the population experienced TTHs at some point in their lifetime (4). Approximately 24% to 37% of individual’s experience TTHs multiple times a month (4). According to Schwartz study in 1998, women are more likely to experience TTHs in every race, age group, and educational level. Tension-type headaches usually begin in an individual’s teenage years, and those between the age of 30 and 39 are at the highest risk (1). Schwartz found that 40.1% of Caucasian men and 46.8% of Caucasian women experienced TTHs in a single year. In the African American population, the prevalence of TTHs in a year was 22.8% in men and 30.9% in women. There is a positive correlation between educational levels and prevalence of TTHs with graduate students being most at risk.
Characteristics/Clinical Presentation[edit | edit source]
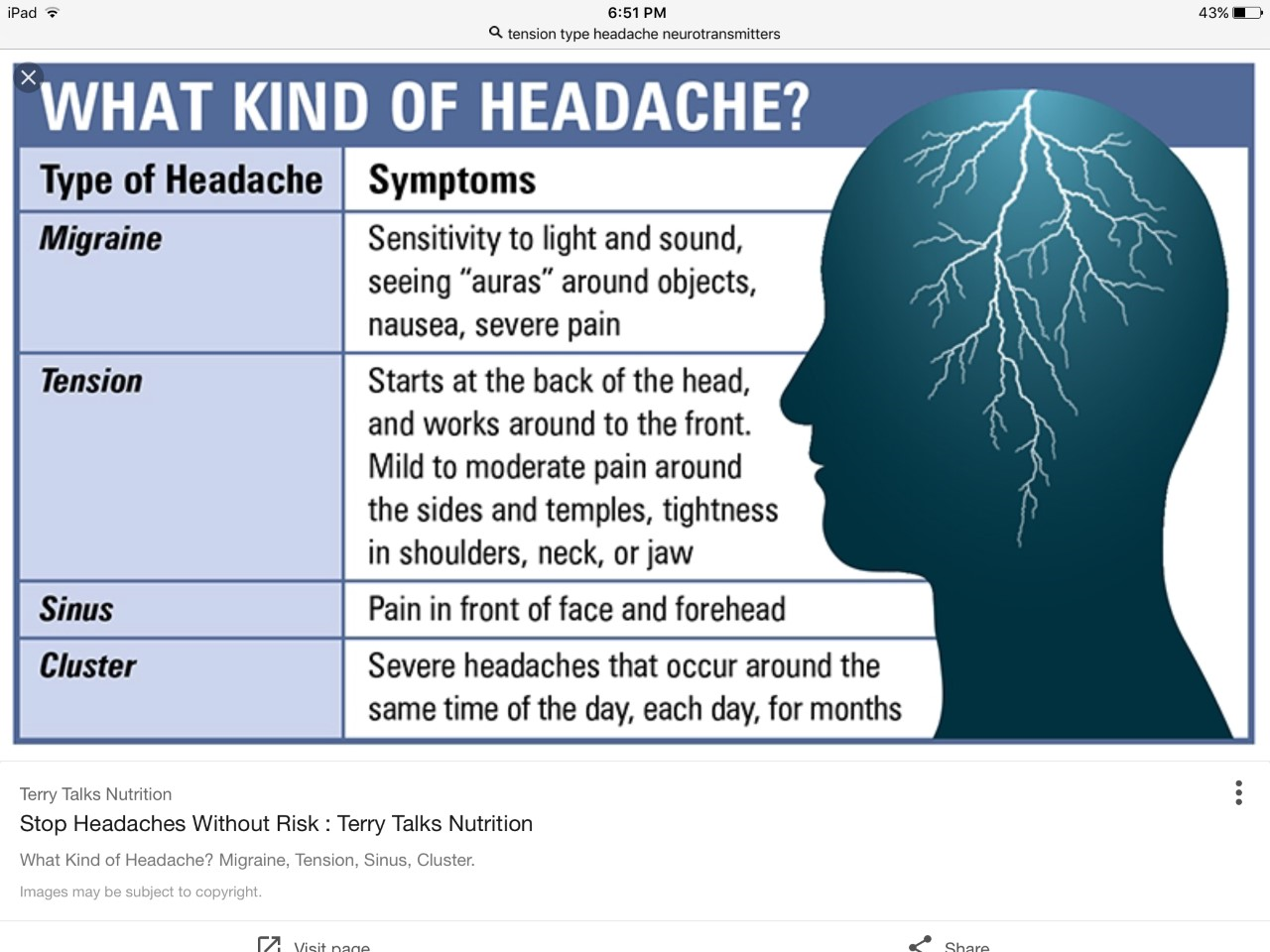
There are two types of tension-type headaches: episodic and chronic. Episodic TTHs are characterized by occurring less than 15 days out of a month (5). They can last anywhere from a few hours to several days. Patients usually report feeling symptoms such as a tight band or pressure around their head and/or neck. These headaches are most often bilateral but can be unilateral. They range from mild to moderate in intensity and do not have any of the associated symptoms which are found in migraines.
TTHs are characterized as chronic when their symptoms persist for 15 or more days within a month for three consecutive months. Because of the moderate to severe intensity of chronic TTHs, this type of headache is more debilitating than the episodic TTHs. In addition to feeling pressure around the head and/or neck, patients with chronic TTHs may experience mild nausea.
Associated Co-morbidities[edit | edit source]
Generalized anxiety disorder (6,7), major depression disorder (6,7,8), impairment in quality of life and functional abilities (8), suicidal ideation (9), dementia (10).
Medications[edit | edit source]
A review of the literature shows that there are several medications which are taken for TTH5 (11). Medication is much more effective in patients with episodic TTH than chronic TTH. Acutely, individuals will use over-the-counter analgesics such as Ibuprofen (400-800mg), Acetylsalicylic acid (600-1000 mg), and Paracetamol (1000mg) when they experience pain one or two days out of the week. Ibuprofen and Acetylsalicylic acid have been found to be much more effective than Paracetamol at treating the pain. Individuals experiencing these headaches should stay away from the use of opioids such as dextropropoxyphene, codeine, and dihydrocodeine. Barbiturates should not be used to treat TTHs.
If an individual experiences episodic TTHs more than twice a week, then their acute intervention should be replaced with prophylactic intervention5 (11). These individuals are often prescribed 10-100 mg of Amitriptyline at night. Amitriptyline is also used to treat chronic TTHs. Nortriptyline is less effective at treating these headaches than Amitriptyline but also produces less anticholinergic side-effects. With the use of pain inhibiting drugs comes the increased risk for medication overuse headaches. A psychological approach is often needed to treat patients with chronic TTHs.
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
If an individual is experiencing frequent headaches, then a medical professional may perform physical and neurological exams to try to determine what is causing them (12). Taking a thorough history may be the most important diagnostic tool in determining a TTH (5). It is important to understand how long an individual has been experiencing these headaches, how long they last, their intensity, and if there are any associated symptoms that accompany the headache. For example, auras are associated with migraines and one can rule out TTH if these symptoms are described. A medical professional may also ask if there are any known triggers and what, if anything, can be done to eliminate the symptoms. A physician may also choose to order a computed tomography (CT) scan, magnetic resonance imaging (MRI), X-Ray, or electroencephalogram (EEG) to rule out other possible causes of the headaches. The HALT index, or headache-attributed lost time index, is a patient reported outcome measure used to determine how headaches are affecting the individual's life. This outcome measurement can help steer decisions in medical treatment. After medical intervention, the Headache and Assessment of Response to Treatment (HART) is used to assess the effectiveness of the treatment. Lastly, individuals are given pamphlets of information describing what a TTH is, the symptoms, and possible treatment options.
Etiology/Causes[edit | edit source]
It is unclear as to what causes tension type headaches. It was once believed that these headaches could be due to either psychological stress factors or muscular contractions of the shoulder, neck, scalp, and jaw but these theories have since been rejected (2). It is now believed that TTH are a result of neurotransmitter (including serotonin) imbalances. Researchers are still trying to determine what could cause the fluctuation in neurotransmitters, but they hypothesize that the imbalances are triggering pain pathways in the brain. There may be an association between tight muscles and changes in neurotransmitters but it is still undetermined if tight muscles are causing the fluctuation in neurotransmitters or vise versa (13).
The following list of possible triggers for TTH was taken from University of Maryland Medical Center: • Stress • Depression • Anxiety • Holding your head in one position for a long time • Sleeping in an awkward position or in a cold room • Eye strain • Drugs or alcohol • Over-exertion • Skipping meals • Head and neck injury, even years after the injury • Clenching your jaw or grinding your teeth (bruxism) • Medications, including some headache medications (leading to rebound headaches) • Arthritis • Hormonal changes (primarily among women)
Systemic Involvement[edit | edit source]
Gastrointestinal (GI) involvement is a common side effect of the drugs which are most often used to treat tension-type headaches (14). These side effects include: GI ulcers, abdominal pain, upset stomach, cramping, nausea, diarrhea, heartburn, bleeding, bloating, constipation, and gas. Another possible side effect of these drugs is symptoms of the headache can worsen. This is most often seen when headaches are severe and an individual overuses the drug. If an individual experience these or any other symptoms after taking medication for a tension-type headache, then they should seek medical attention.
Medical Management (current best evidence)[edit | edit source]
add text here
Physical Therapy Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
add text here
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: addfeedhere|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.