Tackling Overprescription
Introduction[edit | edit source]
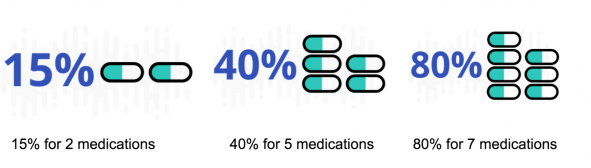
Over the last 30 years, people have been prescribed increasing number of medicines, in particular older people. The reasons are manifold and include:
- A rise in multimorbidity and ageing populations
- Use of of evidence-based medicine
- Greater expectations for outcomes from patients and their families[1]
The dangers of using multiple medicines include greater chances of:
- Adverse drug experiences
- Hospital admissions and health care costs
- Non-adherence to medication[1]
Overprescribing may occur when:
- A better alternative is available but not suggested
- The drug is suitable for a condition but not the individual.
- A condition alters and the medicine is no longer suitable/relevant.
- The patient has ceased needing the medicine but it continues to be prescribed.[2]
Deprescribing[edit | edit source]
Deprescribing is the complicated process undertaken for the safe and effective withdrawal of inappropriate medication.
A lot of of the evidence underpinning deprescribing is from observation, being based on the patient’s physical functioning, co-morbidities, preferences and lifestyle.
Deprescribing
- Should be part of good prescribing, with re-evaluation of dosages periodically.
- Involves health care professional direction and supervision with the same level of expertise and attention that prescribing entails [3].
The following videos provides an easy to follow in-depth discussion regarding the concept (6 minutes)
Overprescribing[edit | edit source]
Overprescribing is when people are prescribed medicines:
- They no longer need or want
- The medicine has greater possible harmful than beneficial effects.
- When a more effective alternative is not prescribed
- Where the medicine is correct for a condition but not the individual.
- When a condition alters and the medicine is no longer appropriate.[1]
The Potential Role of the Physiotherapist in Deprescribing[edit | edit source]
Available literature linking physiotherapy with deprescribing has focused only on the role of physiotherapy as a supplementary treatment for pain relief when reducing opioid dosage.
General advice that may be given on the effects of medication. For example the general side effects of non-steroidal anti-inflammatory drugs (NSAIDs). While providing advice it should also be recommended that the patient should seek advice from a pharmacist or independent prescriber before altering any medication they currently take[4].
Other non-pharmacological (only with doctors input) interventions to help with deprescribing include:
- Encouraging low-salt diets and exercise to reduce prescription of antihypertensives,
- Psychotherapy and changing sleep habits to reduce or avoid prescription of antidepressants,[5][6].
The majority of physiotherapists should be able to signpost patients to where they could obtain appropriate medication advice[7].
Patient taking their medication incorrectly? Advice non-prescribers can give:
If a non-prescriber physiotherapist notices a patient is not taking their medication correctly, they can refer the patient to the medications instructions and remind them how and when/ dose they should be taking their medication as prescribed[4]. This can also apply to medication devices, e.g. an inhaler, advice can be given how to use it according to guidelines. Expected adverse effects of medication? What non-prescribers can do: Physiotherapists can refer the patient back to the GP/pharmacists or can contact the GP directly providing information on their concerns [9].
Common Populations at Risk[edit | edit source]
The use of multiple drugs is not always an indicator of poor drug treatment or overmedication[10]. Appropriate medication depends on whether or not the advantages outweigh the disadvantages which is subjective to both the individual and their given condition(s). It can be very hard to predict the side-effects or clinical effects of a drug combination without testing it on the specific individual as the effects all very based on the individual's genome-specific pharmocokinetics[10]. At risk populations include:
- Elderly Populations
- Psychiatric Patients
- Multimorbidity
- Recent hospitalizations/major surgery
- People seeing multiple doctors
- Terminally ill patients
Non-Pharmacological Interventions[edit | edit source]
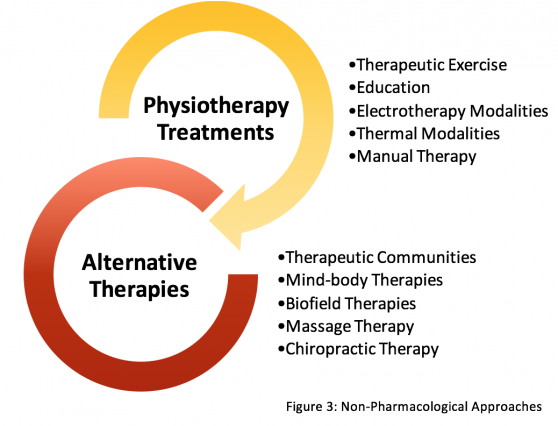
The use of non-pharmacological options in tackling overprescription should be considered across all allied health professionals. For physiotherapists, the vast majority of interventions utilized in practice are non-pharmacological as most clinicians are non-prescribers. It is important for physiotherapists and other relevant health care providers to be aware of the wide array of treatment options for sufficient provision of holistic patient care, to be used on their own or in conjunction with drug therapies, in effort to address clinical scenarios where overprescription may be an issue. The most common treatment for chronic pain is traditionally pharmacological[11]. Health care professionals should be aware of the benefits of non-pharmacological options with sufficient evidence bases for a range of relevant domains such as improvements in pain and functional status, as well as cognitive and emotional states.
A recent 2017 study has discovered barriers to non-pharmacological options with regards to chronic pain[12]. Top ranked patient-reported barriers included high cost, transportation problems, and low motivation. While top provider-reported barriers include scepticism about efficacy of the non-pharmacological options[12]. For this reason, the authors of this Physiopedia page have constructed a non-exhaustive list of common Non-Pharmacological Approaches, accompanied with descriptions and mechanisms of the interventions, brief summary of the evidence base, and suggestions for referrals and signposting patients for options outside the scope of physiotherapy. Some of these options listed are covered under the National Health Service, others can be used for self-management, and some address beliefs and cognitive effects. Therefore, this resource should be used in hopes to address the high cost, transportation, and low motivation barriers of patients, while providing a brief population dependent evidence base for a wide array of non-pharmacological options so healthcare providers can be confident in their choice of treatment option in accordance with the individual values of their patient[12].
The decision to seek non-pharmacological options outside conventional care, should be discussed with a patient’s general practitioner or wider multidisciplinary team, and include patient preferences and values, in order to provide safe and optimal patient-centred care. Non-Pharmacological approaches are listed for both inside and outside the scope of physiotherapy (Figure 3).
References[edit | edit source]
- ↑ 1.0 1.1 1.2 NHS UK Understanding polypharmacy, overprescribing and deprescribing Available:https://www.sps.nhs.uk/articles/understanding-polypharmacy-overprescribing-and-deprescribing/ (accessed 29.12.2022)
- ↑ BBC news Overprescribing of medicines must stop, says government Available:https://www.bbc.com/news/health-58639253 (accessed 28.12.2022)
- ↑ Reeve E, Thompson W, Farrell B. Deprescribing: A narrative review of the evidence and practical recommendations for recognizing opportunities and taking action. European Journal of Internal Medicine.2017;38:3-11.
- ↑ 4.0 4.1 Chartered Society of Physiotherapy. Medicines, prescribing and physiotherapy [Internet]. CSP; 2016. Available from: http://www.csp.org.uk/publications/medicines-prescribing-physiotherapy-4th-edition
- ↑ Kahan M, Mailis-gagnon A, Wilson L, Srivastava A. Canadian guideline for safe and effective use of opioids for chronic noncancer pain Clinical summary for family physicians. Part 1: general population. Canadian Family Physician 2011;57:1257-1266.
- ↑ Berna C, Kulich R.J, Rathmell J.P. Tapering Long-term Opioid Therapy in Chronic Noncancer Pain: Evidence and Recommendations for Everyday Practice. Mayo Clinic Proceedings 2015;90:828-842
- ↑ Chartered Society of Physiotherapy. Practice Guidance for Physiotherapist Supplementary and/or Independent Prescribers in the safe use of medicines. [Internet]. London: CSP; 2016. Available from: http://www.csp.org.uk/publications/practice-guidance-physiotherapist-supplementary-prescribers
- ↑ Youtube. What is Pharmacokinetics? - A simple Introduction! [Internet]. 2017 [cited 15 April 2018]. Available from: https://www.youtube.com/watch?v=caoCN-J5FEE
- ↑ Reznik J, Keren O, Morris J, Biran I. Pharmacology Handbook for Physiotherapists. Australia: Elsevier; 2016.
- ↑ 10.0 10.1 Tamminga C. When Is Polypharmacy an Advantage?. American Journal of Psychiatry. 2011;168(7):663-663.
- ↑ Nalamachu S. An overview of pain management: the clinical efficacy and value of treatment. American journal of managed care 2013;19:261-266
- ↑ 12.0 12.1 12.2 Becker W.C, Dorflinger L, Edmond S.N, Islam L, Heapy A.A, Fraenkel L. Barriers and facilitators to use of non-pharmacological treatments in chronic pain. BMC Family Practice 2017;18 [online] [viewed 18/04/2018]. Available from: http://doi.org/10.1186/s12875-017-0608-2.