Synovial Fluid Analysis
Original Editor - User Name
Top Contributors - Shwe Shwe U Marma, Kim Jackson, Lucinda hampton and Rishika Babburu
Introduction[edit | edit source]
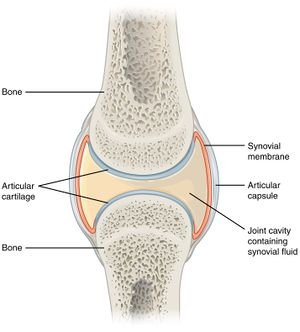
Synovial fluid or joint fluid is physiologic collection of lubricant fluid within a joint space. It acts as source of nutrition for surrounding structures including cartilage, meniscus, labrum etc.[1]Synovial fluid is ultrafiltrate of blood plasma and is primarily composed of proteoglycan 4 or lubricin, hyaluronan and phospholipids.[2]
Purpose[edit | edit source]
Physiologic changes in synovial fluid volume and content occur in response to trauma, inflammation, and bacterial, fungal, or viral penetrance. When patients present with acutely painful joints with suspicion of infection, inflammation or non-inflammatory causes of effusion, synovial fluid aspiration and analysis is imperative to aid in diagnosis and direct treatment modality.[1]
Procedure[edit | edit source]
For analysis, synovial fluid is collected by Arthrocentesis, the procedure to collect synovial fluid from joint by using a needle.[3]
Indication[edit | edit source]
- Presentation of acute painful joint with surrounding warmth/erythema
- Suspicion of septic arthritis
- Suspicion for subacute or chronic periprosthetic joint infection
- Acute exacerbation of chronic knee pain from osteoarthritis or non-inflammatory arthritis, or
- Acute trauma with painful effusion
- A definitive diagnosis of gout or pseudogout
- Effusions of unknown etiology[1]
- In some cases with excess fluid, simply removing some fluid can help relieve pain in the affected joint
- Sometimes synovial fluid analysis is used to monitor people with known joint disorders.[4]
Potential Diagnosis[edit | edit source]
- Inflammatory arthritis including
- gout
- pseudogout,
- infection
- spondylarthritis
- non-inflammatory arthritis which can include effusion from osteoarthritis or meniscal tears
- Septic arthropathy
- acute septic arthropathy
- subacute or chronic septic arthropathy
- periprosthetic joint infection
- Hemorrhagic
- traumatic, often seen with tendon, meniscal or ligament injury[1]
Expected Values per Category[edit | edit source]
| Normal | Non-inflammatory | Inflammatory | Infectious | |
|---|---|---|---|---|
| Color | Clear | Yellow | Yellow | Yellow-green |
| Clarity | Transparent | Transparent | Cloudy | Cloudy |
| Viscosity | High | High | Moderate | Low |
| WBCs | <200 | <2000 | >2000 | >2000 |
| %Polymorphonuclear leucocytes (PMNs) | <25% | <25% | >50% | >75% |
| Crystals | None | None | Possible | None |
| Gram stain | Negative | Negative | Negative | Positive |
| Culture | Negative | Negative | Negative | Positive |
Differential Diagnosis[edit | edit source]
| Non-inflammatory | Inflammatory | Infectious |
|---|---|---|
| Osteoarthritis | Rheumatoid arthritis | Bacterial infection |
| Trauma | Crystal synovitis | Rheumatoid arthritis |
| Avascular necrosis | Spondyloarthropathy | Crystal synovitis |
| Systemic lupus | Reactive arthritis | |
| Acute rheumatic fever | Connective tissue disorders | |
| Endocrine arthropathy | Acute rheumatic fever
Juvenile arthritis Sarcoidosis Tuberculosis Viral infection Fungal infection Bacterial infection |
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Seidman AJ, Limaiem F. Synovial fluid analysis.
- ↑ Blewis ME, Nugent-Derfus GE, Schmidt TA, Schumacher BL, Sah RL. A model of synovial fluid lubricant composition in normal and injured joints. Eur Cell Mater. 2007 Mar 6;13(1):26-39
- ↑ Mackie JW. Joint aspiration: arthrocentesis. Canadian Family Physician. 1987 Sep;33:2057.
- ↑ Healthline. Synovial Fluid Analysis. Available from: www.healthline.com/health/synovial-fluid-analysis (accessed 18 September 2020)
- ↑ TAMING THE SRU. Joint Fluid Analysis in the ED. Available from: www.tamingthesru.com/blog/2016/10/10/joint-fluid-analysis (accessed 18 September 2020)
- ↑ Faryna A, Goldenberg K. Joint fluid.