Supracondylar Humeral Fracture: Difference between revisions
No edit summary |
No edit summary |
||
| Line 9: | Line 9: | ||
The Supracondylar fracture of the [[humerus]] is the fracture of distal end of humerus just above the elbow joint. The transverse section of shaft of humerus is somewhat circular in shape which gets more flattered as it descends down to meet distal end of humerus.<ref name=":2" /> | The Supracondylar fracture of the [[humerus]] is the fracture of distal end of humerus just above the elbow joint. The transverse section of shaft of humerus is somewhat circular in shape which gets more flattered as it descends down to meet distal end of humerus.<ref name=":2" /> | ||
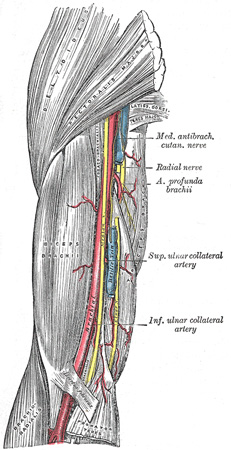
The distal end of humerus comprises of both articular and non-articular structures. Non- articular structure comprises of the medial epicondyle, lateral epicondyle, anterior coronoid and radial fossa and posterior olecranon fossa.Whereas articular structure includes the lateral capitulum articulating with radial head and the medial trochlea articulate with ulna. The medial epicondyle is the site for the common origin of flexor musculature of the forearm and the [[Ulnar Nerve|ulnar nerv]]<nowiki/>e runs in a groove on the back of this epicondyle. The lateral epicondyle is the site for the common origin of extensor musculature of forearm. These muscles attachment are responsible for the displacement and rotation of distal fragment.<ref name=":0" /> In the anterior aspect of distal humerus allow the passage of [https://www.ncbi.nlm.nih.gov/books/NBK537145/ brachial artery] and [[Median Nerve|median nerve.]]<ref name=":2">Gray H. [https://www.bartleby.com/107/51.html Anatomy of the human body.] Lea & Febiger; 1878.</ref> Brachial artery which commonly gets involved in supracondylar fracture of humerus lies along the antero-medial aspect of distal humerus just superficial to the brachialis muscle.<ref name=":0">Kumar V, Singh A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5296534/ Fracture supracondylar humerus: A review.] Journal of clinical and diagnostic research: JCDR. 2016 Dec;10(12):RE01.</ref> The radial nerve runs between the brachialis and brachioradialis muscles before crossing the elbow and penetrating the supinator muscle.<ref name=":0" /> | The distal end of humerus comprises of both articular and non-articular structures. Non- articular structure comprises of the medial epicondyle, lateral epicondyle, anterior coronoid and radial fossa and posterior olecranon fossa.Whereas articular structure includes the lateral capitulum articulating with radial head and the medial trochlea articulate with ulna. | ||
The medial epicondyle is the site for the common origin of flexor musculature of the forearm and the [[Ulnar Nerve|ulnar nerv]]<nowiki/>e runs in a groove on the back of this epicondyle. The lateral epicondyle is the site for the common origin of extensor musculature of forearm. These muscles attachment are responsible for the displacement and rotation of distal fragment.<ref name=":0" /> In the anterior aspect of distal humerus allow the passage of [https://www.ncbi.nlm.nih.gov/books/NBK537145/ brachial artery] and [[Median Nerve|median nerve.]]<ref name=":2">Gray H. [https://www.bartleby.com/107/51.html Anatomy of the human body.] Lea & Febiger; 1878.</ref> Brachial artery which commonly gets involved in supracondylar fracture of humerus lies along the antero-medial aspect of distal humerus just superficial to the brachialis muscle.<ref name=":0">Kumar V, Singh A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5296534/ Fracture supracondylar humerus: A review.] Journal of clinical and diagnostic research: JCDR. 2016 Dec;10(12):RE01.</ref> The radial nerve runs between the brachialis and brachioradialis muscles before crossing the elbow and penetrating the supinator muscle.<ref name=":0" /> | |||
== Epidemiology<ref name=":1" /><ref name=":3" /> == | == Epidemiology<ref name=":1" /><ref name=":3" /> == | ||
* Supracondylar fractures of the humerus are the most frequent fractures of the [[Pediatric Humeral Fracture|pediatric humerus]], with median age being 6 years and a peak incidence at the ages of five to eight years. | * Supracondylar fractures of the humerus are the most frequent fractures of the [[Pediatric Humeral Fracture|pediatric humerus]], with median age being 6 years and a peak incidence at the ages of five to eight years. | ||
| Line 20: | Line 22: | ||
== Mechanism of Injury / Etiology == | == Mechanism of Injury / Etiology == | ||
[[File:Hyperextension Injury.png|thumb| | [[File:Hyperextension Injury.png|thumb|473x473px|Extension type of Supracondylar fracture of humerus]] | ||
Pediatric population predisposed, especially during ages when the supracondylar bone is undergoing skeletal maturation and has a thin and weak cortex.The ossification process of distal humerus occurs at different ages.The supracondylar area undergoes remodeling between 6 to 7 years of age and is typically thinner with a more slender cortex, predisposing this area to fracture.<ref name="Brubacher et al">Brubacher JW, Dodds SD. Pediatric supracondylar fractures of the distal humerus. Curr Rev Musculoskelet Med 2008;1:190-196.</ref><ref name=":0" /> | Pediatric population predisposed, especially during ages when the supracondylar bone is undergoing skeletal maturation and has a thin and weak cortex.The ossification process of distal humerus occurs at different ages.The supracondylar area undergoes remodeling between 6 to 7 years of age and is typically thinner with a more slender cortex, predisposing this area to fracture.<ref name="Brubacher et al">Brubacher JW, Dodds SD. Pediatric supracondylar fractures of the distal humerus. Curr Rev Musculoskelet Med 2008;1:190-196.</ref><ref name=":0" /> | ||
| Line 28: | Line 30: | ||
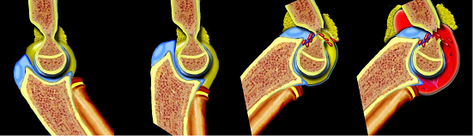
Extension type injury (97% to 99%) is more common than flexion type(1-3%). <ref name=":1" /> | Extension type injury (97% to 99%) is more common than flexion type(1-3%). <ref name=":1" /> | ||
[[File:Fall on out-stretched hand.png|thumb|Fall on outstretched hand ( FOOSH)]] | |||
When a fall on the outstretched hand occurs, the olecranon engages on the olecranon fossa and if elbow extension progresses, the olecranon finally acts as a fulcrum on the fossa. While the anterior elbow joint capsule produces an anterior tensile load, resulting in fracture and disruption of anterior periosteum. Therefore, the bone begins to break at first anteriorly and the fracture progresses posteriorly. If the energy is high, the posterior cortex disrupts, and finally complete posterior displacement of the distal fragment occurs with the posterior periosteum acting as a hinge. This is the mechanism of extension-type fractures.<ref name=":1" /> | When a fall on the outstretched hand occurs, the olecranon engages on the olecranon fossa and if elbow extension progresses, the olecranon finally acts as a fulcrum on the fossa. While the anterior elbow joint capsule produces an anterior tensile load, resulting in fracture and disruption of anterior periosteum. Therefore, the bone begins to break at first anteriorly and the fracture progresses posteriorly. If the energy is high, the posterior cortex disrupts, and finally complete posterior displacement of the distal fragment occurs with the posterior periosteum acting as a hinge. This is the mechanism of extension-type fractures.<ref name=":1" /> | ||
| Line 38: | Line 40: | ||
'''History''' | '''History''' | ||
* Classical history of fall on an | * Classical history of fall on an outstretched hand followed by pain and swelling over the elbow with loss of function of upper limb, onset of pain holds special consideration. | ||
* It is very important to know whethere pain is due to fracture or because of muscle ischemia which has a late onset (hours after the injury).<ref name=":0" /> | * It is very important to know whethere pain is due to fracture or because of muscle ischemia which has a late-onset (hours after the injury).<ref name=":0" /> | ||
'''Observation''' | '''Observation''' | ||
| Line 62: | Line 64: | ||
'''[[Compartment Syndrome of forearm|Compartment syndrome:]]''' severe swelling and/or ecchymosis, anterior skin puckering, and vascular compromise with severe pain. | '''[[Compartment Syndrome of forearm|Compartment syndrome:]]''' severe swelling and/or ecchymosis, anterior skin puckering, and vascular compromise with severe pain. | ||
== Diagnostic Procedures == | == Diagnostic Procedures<ref name=":0" /><ref name=":1" /> == | ||
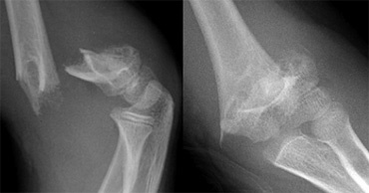
[[File:Supracondylar fractures.png|thumb|Displaced Supracondylar fracture in X-ray|369x369px]] | [[File:Supracondylar fractures.png|thumb|Displaced Supracondylar fracture in X-ray|369x369px]] | ||
Radiographs should include true AP of distal humerus (not elbow) and true lateral elbow views. If | Radiographs should include true AP of distal humerus (not elbow) and true lateral elbow views.If there is only minimal or no displacement these fractures can be occult on radiographs. The only sign will be a positive fat pad sign.<ref name="Omid et al" /><u></u> | ||
'''On lateral view''' | '''On lateral view''' | ||
| Line 120: | Line 122: | ||
== Complications of supracondylar fracture<ref name=":0" /> == | == Complications of supracondylar fracture<ref name=":0" /> == | ||
Immediate complications are associated with neurovascular involvement including | Immediate complications are associated with neurovascular involvement including | ||
# Vascular insufficiency / pink pluseless hand- involvement of brachial artery is most commonly associated with Type II and III supracondylar fractures, frequently encountered in posterolaterally displaced fracture. | |||
# [[Compartment Syndrome of forearm|Compartment syndrome]]: It can occur in 0.1% to 0.3% of cases.Associated forearm fractures and elbow flexion > 90° increase compartment pressures.To minimize the risk of compartment syndrome, the elbow should be immobilized in about 30° of flexion in the emergency room and 60° to 70° of after surgery. | |||
# Neurologic deficit-10 to 20 percent of supracondylar fracture and mainly associated with Type III supracondylar fractures. | |||
# Open or associated forearm fractures | |||
Long term complications in Pediatric population is due to the fact that bones in this age group have an enormous growth as well as remodeling ability. So that long term functional outcome and radiological appearance of a fracture may be quiet different than that of immediate post-management status. | Long term complications in Pediatric population is due to the fact that bones in this age group have an enormous growth as well as remodeling ability. So that long term functional outcome and radiological appearance of a fracture may be quiet different than that of immediate post-management status. | ||
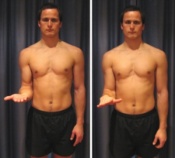
# [https://www.slideshare.net/ramachandrareddy5/cubitus-varus-deformity Cubitus varus deformity:] It occurs due to the malunion and also known as "gunstock” deformity. Posttraumatic cubitus varus deformity has important problems, which are associated with tardy ulnar nerve palsy, tardy Postero-Lateral Rotatory Instability (PLRI), shift of the medial head of the triceps and secondary distal humeral fractures. Modern surgical techniques (e.g., closed reduction with percutaneous pinning) have reduced its frequency from 58 percent to approximately 3 percent in children treated for supracondylar fractures. Humeral osteotomy is used to correct this deformity and to avoid such later complications. | |||
# [[Volkmann's Contracture|Volkmann’s ischemic contracture]]: If compartment syndrome is not treated timely, the associated ischemia may progress to infarction and subsequent development of Volkmann's ischemic contracture: fixed flexion of the elbow, pronation of the forearm, flexion at the wrist, and joint extension of the metacarpal-phalangeal joint. | |||
== Management / Interventions == | == Management / Interventions == | ||
| Line 133: | Line 135: | ||
Management of supracondylar fracture is determined based on type of fracture based on Modified Gartland Classification. | Management of supracondylar fracture is determined based on type of fracture based on Modified Gartland Classification. | ||
<br>'''Type I ( Non-displaced fracture)''' | |||
*Immobilization with a long-arm cast or splint. | *Immobilization with a long-arm cast or splint. | ||
*With elbow flexion up to 80° to 90° and mid pronation-supination are well toleratable for ~3weeks. | *With elbow flexion up to 80° to 90° and mid pronation-supination are well toleratable for ~3weeks. | ||
| Line 149: | Line 150: | ||
# When there is soft-tissue entrapment (i.e. muscle, median nerve, brachial artery) or | # When there is soft-tissue entrapment (i.e. muscle, median nerve, brachial artery) or | ||
# When a cold hand remains without perfusion after an attempt at closed reduction has been performed. | # When a cold hand remains without perfusion after an attempt at closed reduction has been performed. | ||
There is increase incidence of infection,stiffness and myositis ossificans. The anterior approach is the most widely used approach for open reduction mainly when vascular repair is necessary. The lateral approach increases the risk of radial nerve injury and stiffness. The bilaterotricipital posterior approach (Alonso-Llames approach) is not recommended as it has high rate of complications described, such as stiffness, unsightly scarring and risk of trochlea osteonecrosis. | There is increase incidence of infection,stiffness and myositis ossificans in opend reduction. The anterior approach is the most widely used approach for open reduction mainly when vascular repair is necessary. The lateral approach is standard for elbow surgery but in supracondylar fracture increases the risk of radial nerve injury and stiffness. The bilaterotricipital posterior approach (Alonso-Llames approach) is not recommended as it has high rate of complications described, such as stiffness, unsightly scarring and risk of trochlea osteonecrosis. | ||
=== Physiotherapy Management === | === Physiotherapy Management === | ||
Physiotherapy treatment is vital in all patients with a supracondylar fracture to hasten healing and ensure an optimal outcome. The goal of physiotherapy treatment is: | Physiotherapy treatment is vital in all patients with a supracondylar fracture to hasten healing and ensure an optimal outcome. The goal of physiotherapy treatment is: | ||
* To achieve painless and full mobility of the elbow joint. | * To achieve painless and full mobility of the elbow joint. | ||
* To | * To enhance healing process. | ||
* To improve functional abilities of children.<br> | * To strength the affected musculature. | ||
* To improve overall functional abilities of children.<br> | |||
Outcome measures that can be used to compare and evaluate the outcome of treatment are : | Outcome measures that can be used to compare and evaluate the outcome of treatment are : | ||
* Numerical pain rating scale (NPRS)/ [https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1519#:~:text=The%20Faces%20Pain%20Scale%20%E2%80%93%20Revised,pain%20intensity%20developed%20for%20children.&text=Numerical%20self%2Drating%20scales%20(0,to%20provide%20a%20self%2Dreport. Faces Pain Scale] | * Numerical pain rating scale (NPRS)/ [https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1519#:~:text=The%20Faces%20Pain%20Scale%20%E2%80%93%20Revised,pain%20intensity%20developed%20for%20children.&text=Numerical%20self%2Drating%20scales%20(0,to%20provide%20a%20self%2Dreport. Faces Pain Scale] | ||
| Line 161: | Line 163: | ||
* Manual muscle testing ( MMT) | * Manual muscle testing ( MMT) | ||
* [http://www.activitiesscaleforkids.com/ ASK-p (Activities Scale for Kids-performance version)]<ref name=":4" /> | * [http://www.activitiesscaleforkids.com/ ASK-p (Activities Scale for Kids-performance version)]<ref name=":4" /> | ||
'''Evidences''' | |||
The physical therapy management in the paediatric population is very controversial, both its effect and its necessity. A randomized controlled trial done by Schmale et all in 2014, had shown that children with supracondylar fracture treated with either casting or CR with percutaneous pining followed by casting were not benefited by a short course of physical therapy (six sessions of physical therapy performed by any of three therapists over a five-week period beginning the week after cast removal) in terms of either return of function or motion. | |||
In contrary, | |||
== Exercises for a supracondylar fracture == | == Exercises for a supracondylar fracture == | ||
Revision as of 17:05, 21 June 2020
Original Editor - Peter Sheehy
Top Contributors - Manisha Shrestha, Andeela Hafeez, Admin, Kim Jackson, Peter Sheehy, WikiSysop, Karen Wilson and Rishika Babburu
One Page Owner Manisha Shrestha
Clinically Relevant Anatomy[edit | edit source]
The Supracondylar fracture of the humerus is the fracture of distal end of humerus just above the elbow joint. The transverse section of shaft of humerus is somewhat circular in shape which gets more flattered as it descends down to meet distal end of humerus.[1]
The distal end of humerus comprises of both articular and non-articular structures. Non- articular structure comprises of the medial epicondyle, lateral epicondyle, anterior coronoid and radial fossa and posterior olecranon fossa.Whereas articular structure includes the lateral capitulum articulating with radial head and the medial trochlea articulate with ulna.
The medial epicondyle is the site for the common origin of flexor musculature of the forearm and the ulnar nerve runs in a groove on the back of this epicondyle. The lateral epicondyle is the site for the common origin of extensor musculature of forearm. These muscles attachment are responsible for the displacement and rotation of distal fragment.[2] In the anterior aspect of distal humerus allow the passage of brachial artery and median nerve.[1] Brachial artery which commonly gets involved in supracondylar fracture of humerus lies along the antero-medial aspect of distal humerus just superficial to the brachialis muscle.[2] The radial nerve runs between the brachialis and brachioradialis muscles before crossing the elbow and penetrating the supinator muscle.[2]
Epidemiology[3][4][edit | edit source]
- Supracondylar fractures of the humerus are the most frequent fractures of the pediatric humerus, with median age being 6 years and a peak incidence at the ages of five to eight years.
- It is the second most common bony injury in pediatric population.[4]
- It accounts for 55% to 80% of total elbow fractures in children and up to two-thirds of pediatric elbow injuries requiring hospitalization.
- Their incidence has been estimated at 177.3 per 100 000.
- Higher incidence of supracondylar fractures is in boys, affecting the non-dominant arm 1.5 times more frequently.A
- About 10% to 20% of displaced supracondylar fractures present with alterations in vascular status. In most cases, fracture reduction restores perfusion.
- Neural injuries occur in 6.5% to 19% of cases involving displaced fractures. Most of them are neurapraxias. [3]
Mechanism of Injury / Etiology[edit | edit source]
Pediatric population predisposed, especially during ages when the supracondylar bone is undergoing skeletal maturation and has a thin and weak cortex.The ossification process of distal humerus occurs at different ages.The supracondylar area undergoes remodeling between 6 to 7 years of age and is typically thinner with a more slender cortex, predisposing this area to fracture.[5][2]
The distal humerus anatomy is especially predisposed to injury because its configuration in two columns connected by thin bone represents a zone of weakness.[3]
Supracondylar fractures usually occur as result of a fall from height or from sports or leisure or fall on out stretched hand( FOOSH).
Extension type injury (97% to 99%) is more common than flexion type(1-3%). [3]
When a fall on the outstretched hand occurs, the olecranon engages on the olecranon fossa and if elbow extension progresses, the olecranon finally acts as a fulcrum on the fossa. While the anterior elbow joint capsule produces an anterior tensile load, resulting in fracture and disruption of anterior periosteum. Therefore, the bone begins to break at first anteriorly and the fracture progresses posteriorly. If the energy is high, the posterior cortex disrupts, and finally complete posterior displacement of the distal fragment occurs with the posterior periosteum acting as a hinge. This is the mechanism of extension-type fractures.[3]
Flexion-type fractures are usually caused by direct trauma to the flexed elbow. In these cases, the anterior periosteum acts as a hinge, and the progression of the injury goes from the posterior to the anterior part of the distal humerus. The distal fragment also tends to be translated in the coronal plane.[3][2]
Clinical Presentation[edit | edit source]
Supracondylar fracture often present with associated forearm fractures, soft tissue damage, neurologic injury, and significant risk for developing compartment syndrome, thus examination of the entire upper extremity should be performing thoroughly. It includes:[6]
History
- Classical history of fall on an outstretched hand followed by pain and swelling over the elbow with loss of function of upper limb, onset of pain holds special consideration.
- It is very important to know whethere pain is due to fracture or because of muscle ischemia which has a late-onset (hours after the injury).[2]
Observation
- Painful swollen elbow and forearm with hesitant to move.[2]
- Ecchymosis, skin puckering (this sign appears when the proximal fragment transects the brachialis muscle, ‘puckering’ the deep dermis), bruises[3]
- Bleeding puncture wound (indicates open fracture)
- In displaced extension-type fractures, the so-called ‘S-deformity’ is usually present.[3]
Vascular status evaluation:
Vascular compromise exists in up to 10% to 20% of displaced fractures. Both radial and ulnar pulses must be palpated at the wrist of injured extremity. In case of pulselessness ( Pulseless hand), other signs of perfusion must be checked viz., color (the hand should be pink), temperature, capillary refill ( less than 2 seconds) and oxygen saturation on pulse oximeter. [2]
Classification:
- Class I - well perfused (warm and red) with radial pulse
- Class II – well perfused but radial pulse absent
- Class III – poorly perfused (cool and blue or blanched) and radial pulse absent
Neurologic status:
The degree of involvement and possible progression/ regression of symptoms of the nerve is a must before and after treatment. Neuropraxias is common and generally resolve with restoration of normal alignment and lengths.[2]Neuropraxias that usually resolve within two to three months.
- Anterior Interosseous Nerve Branch (AIN) of the median nerve is most prone to get involved in postero-lateral displacement of the distal fracture fragment. Child may present with no sensory loss in hand but a weak" OK sign" (e.g., more of a pincer grasp than an OK sign) on physical examination.
- Radial nerve impingement most commonly occurs when the distal fracture fragment is displaced postero-medially. It can be examined with decrease sensation in dorsal aspect of hand and weak wrist extensors.
- Ulnar nerve is prone to injury following flexion type of supracondylar fractures and loss of sensation in its distribution can be examined following weakness of intrinsic muscles of hand.[2][3]
Compartment syndrome: severe swelling and/or ecchymosis, anterior skin puckering, and vascular compromise with severe pain.
Diagnostic Procedures[2][3][edit | edit source]
Radiographs should include true AP of distal humerus (not elbow) and true lateral elbow views.If there is only minimal or no displacement these fractures can be occult on radiographs. The only sign will be a positive fat pad sign.[6]
On lateral view
The lateral view also allows assessing the degree of displacement and the integrity of the posterior cortex.
On the lateral view, the following radiological parameters are looked for: (a) Anterior humeral line; (b) Coronoid line; (c) Fish tail sign; (d) Fat pad sign; (Anterior and Posterior).
Anterior humeral line to capitulum orientation on a lateral view
- Normal elbow - line continues the anterior cortical of the humerus and should traverse the capitulum in its middle third line.
- Extension type injury: capitulum posterior to line
- Flexion type injury: capitulum anterior to the line
On AP view
It helps to evaluate the direction of displacement, the presence of varus or valgus alignment, and the extent of the fracture comminution.
The Baumann angle (Humeral capitular angle) on AP view
- Angle between line perpendicular to long axis of humeral shaft and the physeal line of the capitulum, is used to assess varus or valgus alignment of the distal humerus.
- Normal range – 64º to 82º degrees
- Decrease in angle – varus angulated fracture with possible medial column comminution
The Ulnohumeral angle or radiological carrying angle on AP view
- The angle formed by the diaphyseal axis of the humerus and the axis of the proximal third of the ulna.
- It is also used to assess varus or valgus deformity and it is more accurate and useful than Baumann’s angle [3]
Classification of Supracondylar fracture[edit | edit source]
Modified Gartland classification( 2006)of supracondylar fractures (based on lateral radiograph):[6][5][3][7]
Type I
- Nondisplaced or minimally displaced (<2mm) with intact anterior humeral line
- No disruption of periosteum – stable fracture
- Fat pad signs may be only finding
Type II
- Displaced (>2mm) with hinged intact posterior cortex
- Anterior humeral line does not pass through middle third of capitellum on lateral radiographs
- No rotational deformity on AP radiograph
Type III
- Displaced with no meaningful cortical contact, usually sagittal plane extension and frontal/horizontal plane rotation
- Significant periosteum disrupture, soft tissue and neurovascular injuries common
- Medial column comminution and collapse with malrotation in frontal plane
Type IV
- Multidirectional instability
- Incompetent periosteal hinge circumferentially, with instability in flexion and extension
Complications of supracondylar fracture[2][edit | edit source]
Immediate complications are associated with neurovascular involvement including
- Vascular insufficiency / pink pluseless hand- involvement of brachial artery is most commonly associated with Type II and III supracondylar fractures, frequently encountered in posterolaterally displaced fracture.
- Compartment syndrome: It can occur in 0.1% to 0.3% of cases.Associated forearm fractures and elbow flexion > 90° increase compartment pressures.To minimize the risk of compartment syndrome, the elbow should be immobilized in about 30° of flexion in the emergency room and 60° to 70° of after surgery.
- Neurologic deficit-10 to 20 percent of supracondylar fracture and mainly associated with Type III supracondylar fractures.
- Open or associated forearm fractures
Long term complications in Pediatric population is due to the fact that bones in this age group have an enormous growth as well as remodeling ability. So that long term functional outcome and radiological appearance of a fracture may be quiet different than that of immediate post-management status.
- Cubitus varus deformity: It occurs due to the malunion and also known as "gunstock” deformity. Posttraumatic cubitus varus deformity has important problems, which are associated with tardy ulnar nerve palsy, tardy Postero-Lateral Rotatory Instability (PLRI), shift of the medial head of the triceps and secondary distal humeral fractures. Modern surgical techniques (e.g., closed reduction with percutaneous pinning) have reduced its frequency from 58 percent to approximately 3 percent in children treated for supracondylar fractures. Humeral osteotomy is used to correct this deformity and to avoid such later complications.
- Volkmann’s ischemic contracture: If compartment syndrome is not treated timely, the associated ischemia may progress to infarction and subsequent development of Volkmann's ischemic contracture: fixed flexion of the elbow, pronation of the forearm, flexion at the wrist, and joint extension of the metacarpal-phalangeal joint.
Management / Interventions[edit | edit source]
Medical[edit | edit source]
Management of supracondylar fracture is determined based on type of fracture based on Modified Gartland Classification.
Type I ( Non-displaced fracture)
- Immobilization with a long-arm cast or splint.
- With elbow flexion up to 80° to 90° and mid pronation-supination are well toleratable for ~3weeks.
- Flexion of the elbow within the cast should not pass 90° because it can increase forearm pressures and impede distal vascular flow.
- Radiographic check at 1 and 2 weeks
Types II
- A closed reduction and percutaneous pinning fixation is recommended than CR and immobilization as the risk of complication is low. Pins are removed in the hospital approximately three weeks after surgery.[8]
Type III and Type IV
- Closed reduction and percutaneous pinning is the gold standard for all displaced fractures and is widely used in Type III and IV fractures.
- Open reduction is indicated:
- When the surgeon is not able to reduce the fracture by closed means
- When there is soft-tissue entrapment (i.e. muscle, median nerve, brachial artery) or
- When a cold hand remains without perfusion after an attempt at closed reduction has been performed.
There is increase incidence of infection,stiffness and myositis ossificans in opend reduction. The anterior approach is the most widely used approach for open reduction mainly when vascular repair is necessary. The lateral approach is standard for elbow surgery but in supracondylar fracture increases the risk of radial nerve injury and stiffness. The bilaterotricipital posterior approach (Alonso-Llames approach) is not recommended as it has high rate of complications described, such as stiffness, unsightly scarring and risk of trochlea osteonecrosis.
Physiotherapy Management[edit | edit source]
Physiotherapy treatment is vital in all patients with a supracondylar fracture to hasten healing and ensure an optimal outcome. The goal of physiotherapy treatment is:
- To achieve painless and full mobility of the elbow joint.
- To enhance healing process.
- To strength the affected musculature.
- To improve overall functional abilities of children.
Outcome measures that can be used to compare and evaluate the outcome of treatment are :
- Numerical pain rating scale (NPRS)/ Faces Pain Scale
- Range of motion- Goniometry
- Manual muscle testing ( MMT)
- ASK-p (Activities Scale for Kids-performance version)[8]
Evidences
The physical therapy management in the paediatric population is very controversial, both its effect and its necessity. A randomized controlled trial done by Schmale et all in 2014, had shown that children with supracondylar fracture treated with either casting or CR with percutaneous pining followed by casting were not benefited by a short course of physical therapy (six sessions of physical therapy performed by any of three therapists over a five-week period beginning the week after cast removal) in terms of either return of function or motion.
In contrary,
Exercises for a supracondylar fracture[edit | edit source]
The following exercises are commonly prescribed to patients with a supracondylar fracture following confirmation that the fracture has healed, and that the orthopaedic specialist has indicated it is safe to begin mobilization. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 3 times daily and only provided they do not cause or increase symptoms.
Elbow Bend to Straighten[edit | edit source]
Bend and straighten your elbow as far as possible pain free (figure 3). Aim for no more than a mild to moderate stretch. Repeat 10 times provided there is no increase in symptoms.
Forearm Rotations[edit | edit source]
Begin this exercise with your elbow at your side and bent to 90 degrees (figure 4). Slowly rotate your palm up and down as far as possible pain free. Aim for no more than a mild to moderate stretch. Repeat 10 times provided there is no increase in symptoms.
Tennis Ball Squeeze[edit | edit source]
Begin this exercise holding a tennis ball (figure 5). Squeeze the tennis ball as hard as possible and comfortable without pain. Hold for 5 seconds and repeat 10 times.
Conclusion[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Gray H. Anatomy of the human body. Lea & Febiger; 1878.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Kumar V, Singh A. Fracture supracondylar humerus: A review. Journal of clinical and diagnostic research: JCDR. 2016 Dec;10(12):RE01.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 Vaquero-Picado A, González-Morán G, Moraleda L. Management of supracondylar fractures of the humerus in children. EFORT open reviews. 2018 Oct;3(10):526-40.
- ↑ 4.0 4.1 Zhang XN, Yang JP, Wang Z, Qi Y, Meng XH. A systematic review and meta-analysis of two different managements for supracondylar humeral fractures in children. Journal of orthopaedic surgery and research. 2018 Dec 1;13(1):141.
- ↑ 5.0 5.1 Brubacher JW, Dodds SD. Pediatric supracondylar fractures of the distal humerus. Curr Rev Musculoskelet Med 2008;1:190-196.
- ↑ 6.0 6.1 6.2 Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am 2008;90:1121-32.
- ↑ Alton TB, Werner SE, Gee AO. Classifications in brief: the Gartland classification of supracondylar humerus fractures.
- ↑ 8.0 8.1 Schmale GA, Mazor S, Mercer LD, Bompadre V. Lack of benefit of physical therapy on function following supracondylar humeral fracture: a randomized controlled trial. The Journal of Bone and Joint surgery. American Volume. 2014 Jun 4;96(11):944.