Supracondylar Humeral Fracture: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
</div> | </div> | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
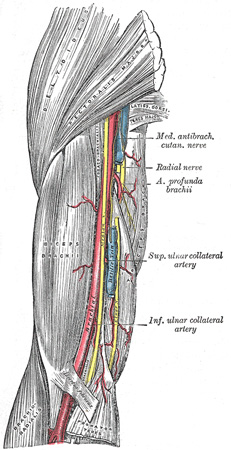
[[File:The Brachial Artery.jpeg|thumb|Relation of distal end of arm with brachial artery and median nerve.]] | |||
The Supracondylar fracture of the [[humerus]] is the fracture of distal end of humerus just above the elbow joint. The transverse section of shaft of humerus is somewhat circular in shape which gets more flattered as it descends down to meet distal end of humerus.<ref name=":2" /> | |||
The distal end of humerus comprises of both articular and non-articular structures. Non- articular structure comprises of the medial epicondyle, lateral epicondyle, anterior coronoid and radial fossa and posterior olecranon fossa.Whereas articular structure includes the lateral capitulum articulating with radial head and the medial trochlea articulate with ulna. The medial epicondyle is the site for the common origin of flexor musculature of the forearm and the [[Ulnar Nerve|ulnar nerv]]<nowiki/>e runs in a groove on the back of this epicondyle. The lateral epicondyle is the site for the common origin of extensor musculature of forearm. These muscles attachment are responsible for the displacement and rotation of distal fragment.<ref name=":0" /> In the anterior aspect of distal humerus allow the passage of [https://www.ncbi.nlm.nih.gov/books/NBK537145/ brachial artery] and [[Median Nerve|median nerve.]]<ref name=":2">Gray H. [https://www.bartleby.com/107/51.html Anatomy of the human body.] Lea & Febiger; 1878.</ref> Brachial artery which commonly gets involved in supracondylar fracture of humerus lies along the antero-medial aspect of distal humerus just superficial to the brachialis muscle.<ref name=":0">Kumar V, Singh A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5296534/ Fracture supracondylar humerus: A review.] Journal of clinical and diagnostic research: JCDR. 2016 Dec;10(12):RE01.</ref> The radial nerve runs between the brachialis and brachioradialis muscles before crossing the elbow and penetrating the supinator muscle.<ref name=":0" /> | |||
== Epidemiology<ref name=":1" /><ref name=":3" /> == | |||
The distal end of humerus comprises of both articular and non-articular structures. Non- articular structure comprises of the medial epicondyle, lateral epicondyle, anterior coronoid and radial fossa and posterior olecranon fossa.Whereas articular structure includes the lateral capitulum articulating with radial head and the medial trochlea articulate with ulna. The medial epicondyle is the site for the common origin of flexor musculature of the forearm and the [[Ulnar Nerve|ulnar nerv]]<nowiki/>e runs in a groove on the back of this epicondyle. The lateral epicondyle is the site for the common origin of extensor musculature of forearm. These muscles attachment are responsible for the displacement and rotation of distal fragment. In the anterior aspect of distal humerus allow the passage of [https://www.ncbi.nlm.nih.gov/books/NBK537145/ brachial artery] and [[Median Nerve|median nerve.]]<ref>Gray H. [https://www.bartleby.com/107/51.html Anatomy of the human body.] Lea & Febiger; 1878.</ref> Brachial artery which commonly gets involved in supracondylar fracture of humerus lies along the antero-medial aspect of distal humerus just superficial to the brachialis muscle.<ref name=":0">Kumar V, Singh A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5296534/ Fracture supracondylar humerus: A review.] Journal of clinical and diagnostic research: JCDR. 2016 Dec;10(12):RE01.</ref> | |||
== Epidemiology == | |||
* Supracondylar fractures of the humerus are the most frequent fractures of the [[Pediatric Humeral Fracture|pediatric humerus]], with median age being 6 years and a peak incidence at the ages of five to eight years. | * Supracondylar fractures of the humerus are the most frequent fractures of the [[Pediatric Humeral Fracture|pediatric humerus]], with median age being 6 years and a peak incidence at the ages of five to eight years. | ||
* It is the second most common bony injury in pediatric population.<ref>Zhang XN, Yang JP, Wang Z, Qi Y, Meng XH. [https://josr-online.biomedcentral.com/articles/10.1186/s13018-018-0806-1 A systematic review and meta-analysis of two different managements for supracondylar humeral fractures in children.] Journal of orthopaedic surgery and research. 2018 Dec 1;13(1):141.</ref> | * It is the second most common bony injury in pediatric population.<ref name=":3">Zhang XN, Yang JP, Wang Z, Qi Y, Meng XH. [https://josr-online.biomedcentral.com/articles/10.1186/s13018-018-0806-1 A systematic review and meta-analysis of two different managements for supracondylar humeral fractures in children.] Journal of orthopaedic surgery and research. 2018 Dec 1;13(1):141.</ref> | ||
* It accounts for 55% to 80% of total elbow fractures in children and up to two-thirds of pediatric elbow injuries requiring hospitalization. | * It accounts for 55% to 80% of total elbow fractures in children and up to two-thirds of pediatric elbow injuries requiring hospitalization. | ||
* Their incidence has been estimated at 177.3 per 100 000. | * Their incidence has been estimated at 177.3 per 100 000. | ||
| Line 22: | Line 20: | ||
== Mechanism of Injury / Etiology == | == Mechanism of Injury / Etiology == | ||
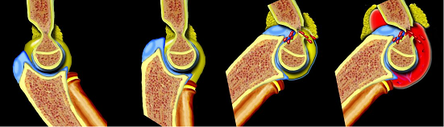
[[File:Hyperextension Injury.png|thumb| | [[File:Hyperextension Injury.png|thumb|444x444px|Extension type of Supracondylar fracture of humerus]] | ||
Pediatric population predisposed, especially during ages when the supracondylar bone is undergoing skeletal maturation and has a thin and weak cortex.The ossification process of distal humerus occurs at different ages.The supracondylar area undergoes remodeling between 6 to 7 years of age and is typically thinner with a more slender cortex, predisposing this area to fracture.<ref name="Brubacher et al">Brubacher JW, Dodds SD. Pediatric supracondylar fractures of the distal humerus. Curr Rev Musculoskelet Med 2008;1:190-196.</ref><ref name=":0" /> | Pediatric population predisposed, especially during ages when the supracondylar bone is undergoing skeletal maturation and has a thin and weak cortex.The ossification process of distal humerus occurs at different ages.The supracondylar area undergoes remodeling between 6 to 7 years of age and is typically thinner with a more slender cortex, predisposing this area to fracture.<ref name="Brubacher et al">Brubacher JW, Dodds SD. Pediatric supracondylar fractures of the distal humerus. Curr Rev Musculoskelet Med 2008;1:190-196.</ref><ref name=":0" /> | ||
| Line 31: | Line 29: | ||
Extension type injury (97% to 99%) is more common than flexion type(1-3%). <ref name=":1" /> | Extension type injury (97% to 99%) is more common than flexion type(1-3%). <ref name=":1" /> | ||
When a fall on the outstretched hand occurs, the olecranon engages on the olecranon fossa and if elbow extension progresses, the olecranon finally acts as a fulcrum on the fossa. While the anterior elbow joint capsule produces an anterior tensile load, resulting in fracture and disruption of anterior periosteum. Therefore, the bone begins to break at first anteriorly and the fracture progresses posteriorly. If the energy is high, the posterior cortex disrupts, and finally complete posterior displacement of the distal fragment occurs with the posterior periosteum acting as a hinge. This is the mechanism of extension-type fractures. | When a fall on the outstretched hand occurs, the olecranon engages on the olecranon fossa and if elbow extension progresses, the olecranon finally acts as a fulcrum on the fossa. While the anterior elbow joint capsule produces an anterior tensile load, resulting in fracture and disruption of anterior periosteum. Therefore, the bone begins to break at first anteriorly and the fracture progresses posteriorly. If the energy is high, the posterior cortex disrupts, and finally complete posterior displacement of the distal fragment occurs with the posterior periosteum acting as a hinge. This is the mechanism of extension-type fractures.<ref name=":1" /> | ||
Flexion-type fractures are usually caused by direct trauma to the flexed elbow. In these cases, the anterior periosteum acts as a hinge, and the progression of the injury goes from the posterior to the anterior part of the distal humerus. The distal fragment also tends to be translated in the coronal plane.<ref name=":1" /><ref name=":0" /> | Flexion-type fractures are usually caused by direct trauma to the flexed elbow. In these cases, the anterior periosteum acts as a hinge, and the progression of the injury goes from the posterior to the anterior part of the distal humerus. The distal fragment also tends to be translated in the coronal plane.<ref name=":1" /><ref name=":0" /> | ||
| Line 37: | Line 35: | ||
== Clinical Presentation == | == Clinical Presentation == | ||
Supracondylar fracture often present with associated forearm fractures, soft tissue damage, neurologic injury, and significant risk for developing compartment syndrome, thus examination of the entire upper extremity should be performing | Supracondylar fracture often present with associated forearm fractures, soft tissue damage, neurologic injury, and significant risk for developing compartment syndrome, thus examination of the entire upper extremity should be performing thoroughly. It includes:<ref name="Omid et al">Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am 2008;90:1121-32.</ref> | ||
* | '''History''' | ||
* Classical history of fall on an out stretched hand followed by pain and swelling over the elbow with loss of function of upper limb, onset of pain holds special consideration. | |||
* It is very important to know whethere pain is due to fracture or because of muscle ischemia which has a late onset (hours after the injury).<ref name=":0" /> | |||
'''Observation''' | |||
*Painful swollen elbow and forearm with hesitant to move.<ref name=":0" /> | |||
*Ecchymosis, skin puckering (this sign appears when the proximal fragment transects the brachialis muscle, ‘puckering’ the deep dermis), bruises<ref name=":1" /> | |||
*Bleeding puncture wound (indicates open fracture) | *Bleeding puncture wound (indicates open fracture) | ||
*Vascular status | *In displaced extension-type fractures, the so-called ‘S-deformity’ is usually present.<ref name=":1" /> | ||
'''Vascular status evaluation:''' | |||
Vascular compromise exists in up to 10% to 20% of displaced fractures. Both radial and ulnar pulses must be palpated at the wrist of injured extremity. In case of pulselessness ( Pulseless hand), other signs of perfusion must be checked viz., color (the hand should be pink), temperature, capillary refill ( less than 2 seconds) and oxygen saturation on pulse oximeter. <ref name=":0" /> | |||
*Compartment syndrome | Classification: | ||
*Class I - well perfused (warm and red) with radial pulse | |||
*Class II – well perfused but radial pulse absent | |||
*Class III – poorly perfused (cool and blue or blanched) and radial pulse absent | |||
'''Neurologic status:''' | |||
The degree of involvement and possible progression/ regression of symptoms of the nerve is a must before and after treatment. Neuropraxias is common and generally resolve with restoration of normal alignment and lengths.<ref name=":0" /> | |||
* Anterior Interosseous Nerve Branch (AIN) of the median nerve is most prone to get involved in postero-lateral displacement of the distal fracture fragment. Child may present with no sensory loss in hand but a weak" OK sign" (e.g., more of a pincer grasp than an OK sign) on physical examination. | |||
* Radial nerve impingement most commonly occurs when the distal fracture fragment is displaced postero-medially. It can be examined with decrease sensation in dorsal aspect of hand and weak wrist extensors. | |||
* Ulnar nerve is prone to injury following flexion type of supracondylar fractures and loss of sensation in its distribution can be examined following weakness of intrinsic muscles of hand.<ref name=":0" /><ref name=":1" /> | |||
'''Compartment syndrome:''' severe swelling and/or ecchymosis, anterior skin puckering, and vascular compromise with severe pain. | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
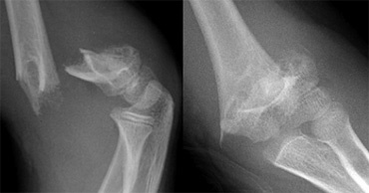
[[File:Supracondylar fractures.png|thumb|Displaced Supracondylar fracture in X-ray|369x369px]] | |||
Radiographs should include true AP of distal humerus (not elbow) and true lateral elbow views. If signs of osseous injury (fat pad sign) present the following 2 parameters used to assess for supracondylar fracture.<ref name="Omid et al" /><u></u> | |||
'''On lateral view''' | |||
The lateral view also allows assessing the degree of displacement and the integrity of the posterior cortex. | |||
On the lateral view, the following radiological parameters are looked for: (a) Anterior humeral line; (b) Coronoid line; (c) Fish tail sign; (d) Fat pad sign; (Anterior and Posterior). | |||
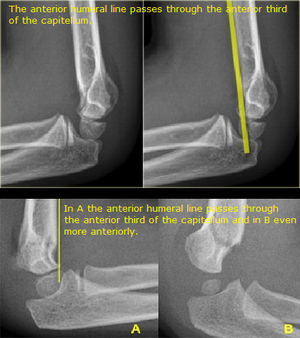
[[File:Anterior humeral line abnormal.png|thumb|Anterior Humeral Line Abnormal]] | |||
<u>[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6335593/#!po=14.1026 Anterior humeral line] to capitulum orientation on a lateral view</u> | |||
*Normal elbow - line continues the anterior cortical of the humerus and should traverse the capitulum in its middle third line. | |||
*Extension type injury: capitulum posterior to line | |||
*Flexion type injury: capitulum anterior to the line | |||
'''On AP view''' | |||
It helps to evaluate the direction of displacement, the presence of varus or valgus alignment, and the extent of the fracture comminution. | |||
<u>The Baumann angle (Humeral | <u>[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6335593/#!po=16.6667 The Baumann angle] (Humeral capitular angle) on AP view</u><br> | ||
*Angle between line perpendicular to long axis of humeral shaft and | *Angle between line perpendicular to long axis of humeral shaft and the physeal line of the capitulum, is used to assess varus or valgus alignment of the distal humerus. | ||
*Normal range – | *Normal range – 64º to 82º degrees | ||
*Decrease in angle – varus angulated fracture with possible medial column comminution <br> | *Decrease in angle – varus angulated fracture with possible medial column comminution <br> | ||
<u>The Ulnohumeral angle or radiological carrying angle on AP view</u> | |||
* The angle formed by the diaphyseal axis of the humerus and the axis of the proximal third of the ulna. | |||
* It is also used to assess varus or valgus deformity and it is more accurate and useful than Baumann’s angle <ref name=":1" /> | |||
'''<u>Modified Gartland classification of supracondylar fractures (based on lateral radiograph):<ref name="Omid et al" /><ref name="Brubacher et al" /></u>''' | == Classification of Supracondylar fracture == | ||
'''<u>Modified Gartland classification( 2006)of supracondylar fractures (based on lateral radiograph):<ref name="Omid et al" /><ref name="Brubacher et al" /></u>''' | |||
'''Type I''' | '''Type I''' | ||
*Nondisplaced or minimally displaced (<2mm) with intact anterior humeral line | *Nondisplaced or minimally displaced (<2mm) with intact anterior humeral line | ||
| Line 71: | Line 101: | ||
*Fat pad signs may be only finding | *Fat pad signs may be only finding | ||
'''Type II''' | '''Type II''' | ||
*Displaced (>2mm) with hinged intact posterior cortex | *Displaced (>2mm) with hinged intact posterior cortex | ||
| Line 77: | Line 107: | ||
*No rotational deformity on AP radiograph | *No rotational deformity on AP radiograph | ||
'''Type III''' | '''Type III''' | ||
*Displaced with no meaningful cortical contact, usually sagittal plane extension and frontal/horizontal plane rotation | *Displaced with no meaningful cortical contact, usually sagittal plane extension and frontal/horizontal plane rotation | ||
| Line 83: | Line 113: | ||
*Medial column comminution and collapse with malrotation in frontal plane | *Medial column comminution and collapse with malrotation in frontal plane | ||
'''Type IV ''' | '''Type IV ''' | ||
*Multidirectional instability | *Multidirectional instability | ||
Revision as of 07:52, 21 June 2020
Original Editor - Peter Sheehy
Top Contributors - Manisha Shrestha, Andeela Hafeez, Admin, Kim Jackson, Peter Sheehy, WikiSysop, Karen Wilson and Rishika Babburu
One Page Owner Manisha Shrestha
Clinically Relevant Anatomy[edit | edit source]
The Supracondylar fracture of the humerus is the fracture of distal end of humerus just above the elbow joint. The transverse section of shaft of humerus is somewhat circular in shape which gets more flattered as it descends down to meet distal end of humerus.[1]
The distal end of humerus comprises of both articular and non-articular structures. Non- articular structure comprises of the medial epicondyle, lateral epicondyle, anterior coronoid and radial fossa and posterior olecranon fossa.Whereas articular structure includes the lateral capitulum articulating with radial head and the medial trochlea articulate with ulna. The medial epicondyle is the site for the common origin of flexor musculature of the forearm and the ulnar nerve runs in a groove on the back of this epicondyle. The lateral epicondyle is the site for the common origin of extensor musculature of forearm. These muscles attachment are responsible for the displacement and rotation of distal fragment.[2] In the anterior aspect of distal humerus allow the passage of brachial artery and median nerve.[1] Brachial artery which commonly gets involved in supracondylar fracture of humerus lies along the antero-medial aspect of distal humerus just superficial to the brachialis muscle.[2] The radial nerve runs between the brachialis and brachioradialis muscles before crossing the elbow and penetrating the supinator muscle.[2]
Epidemiology[3][4][edit | edit source]
- Supracondylar fractures of the humerus are the most frequent fractures of the pediatric humerus, with median age being 6 years and a peak incidence at the ages of five to eight years.
- It is the second most common bony injury in pediatric population.[4]
- It accounts for 55% to 80% of total elbow fractures in children and up to two-thirds of pediatric elbow injuries requiring hospitalization.
- Their incidence has been estimated at 177.3 per 100 000.
- Higher incidence of supracondylar fractures is in boys, affecting the non-dominant arm 1.5 times more frequently.A
- About 10% to 20% of displaced supracondylar fractures present with alterations in vascular status. In most cases, fracture reduction restores perfusion.
- Neural injuries occur in 6.5% to 19% of cases involving displaced fractures. Most of them are neurapraxias. [3]
Mechanism of Injury / Etiology[edit | edit source]
Pediatric population predisposed, especially during ages when the supracondylar bone is undergoing skeletal maturation and has a thin and weak cortex.The ossification process of distal humerus occurs at different ages.The supracondylar area undergoes remodeling between 6 to 7 years of age and is typically thinner with a more slender cortex, predisposing this area to fracture.[5][2]
The distal humerus anatomy is especially predisposed to injury because its configuration in two columns connected by thin bone represents a zone of weakness.[3]
Supracondylar fractures usually occur as result of a fall from height or from sports or leisure or fall on out stretched hand( FOOSH).
Extension type injury (97% to 99%) is more common than flexion type(1-3%). [3]
When a fall on the outstretched hand occurs, the olecranon engages on the olecranon fossa and if elbow extension progresses, the olecranon finally acts as a fulcrum on the fossa. While the anterior elbow joint capsule produces an anterior tensile load, resulting in fracture and disruption of anterior periosteum. Therefore, the bone begins to break at first anteriorly and the fracture progresses posteriorly. If the energy is high, the posterior cortex disrupts, and finally complete posterior displacement of the distal fragment occurs with the posterior periosteum acting as a hinge. This is the mechanism of extension-type fractures.[3]
Flexion-type fractures are usually caused by direct trauma to the flexed elbow. In these cases, the anterior periosteum acts as a hinge, and the progression of the injury goes from the posterior to the anterior part of the distal humerus. The distal fragment also tends to be translated in the coronal plane.[3][2]
Clinical Presentation[edit | edit source]
Supracondylar fracture often present with associated forearm fractures, soft tissue damage, neurologic injury, and significant risk for developing compartment syndrome, thus examination of the entire upper extremity should be performing thoroughly. It includes:[6]
History
- Classical history of fall on an out stretched hand followed by pain and swelling over the elbow with loss of function of upper limb, onset of pain holds special consideration.
- It is very important to know whethere pain is due to fracture or because of muscle ischemia which has a late onset (hours after the injury).[2]
Observation
- Painful swollen elbow and forearm with hesitant to move.[2]
- Ecchymosis, skin puckering (this sign appears when the proximal fragment transects the brachialis muscle, ‘puckering’ the deep dermis), bruises[3]
- Bleeding puncture wound (indicates open fracture)
- In displaced extension-type fractures, the so-called ‘S-deformity’ is usually present.[3]
Vascular status evaluation:
Vascular compromise exists in up to 10% to 20% of displaced fractures. Both radial and ulnar pulses must be palpated at the wrist of injured extremity. In case of pulselessness ( Pulseless hand), other signs of perfusion must be checked viz., color (the hand should be pink), temperature, capillary refill ( less than 2 seconds) and oxygen saturation on pulse oximeter. [2]
Classification:
- Class I - well perfused (warm and red) with radial pulse
- Class II – well perfused but radial pulse absent
- Class III – poorly perfused (cool and blue or blanched) and radial pulse absent
Neurologic status:
The degree of involvement and possible progression/ regression of symptoms of the nerve is a must before and after treatment. Neuropraxias is common and generally resolve with restoration of normal alignment and lengths.[2]
- Anterior Interosseous Nerve Branch (AIN) of the median nerve is most prone to get involved in postero-lateral displacement of the distal fracture fragment. Child may present with no sensory loss in hand but a weak" OK sign" (e.g., more of a pincer grasp than an OK sign) on physical examination.
- Radial nerve impingement most commonly occurs when the distal fracture fragment is displaced postero-medially. It can be examined with decrease sensation in dorsal aspect of hand and weak wrist extensors.
- Ulnar nerve is prone to injury following flexion type of supracondylar fractures and loss of sensation in its distribution can be examined following weakness of intrinsic muscles of hand.[2][3]
Compartment syndrome: severe swelling and/or ecchymosis, anterior skin puckering, and vascular compromise with severe pain.
Diagnostic Procedures[edit | edit source]
Radiographs should include true AP of distal humerus (not elbow) and true lateral elbow views. If signs of osseous injury (fat pad sign) present the following 2 parameters used to assess for supracondylar fracture.[6]
On lateral view
The lateral view also allows assessing the degree of displacement and the integrity of the posterior cortex.
On the lateral view, the following radiological parameters are looked for: (a) Anterior humeral line; (b) Coronoid line; (c) Fish tail sign; (d) Fat pad sign; (Anterior and Posterior).
Anterior humeral line to capitulum orientation on a lateral view
- Normal elbow - line continues the anterior cortical of the humerus and should traverse the capitulum in its middle third line.
- Extension type injury: capitulum posterior to line
- Flexion type injury: capitulum anterior to the line
On AP view
It helps to evaluate the direction of displacement, the presence of varus or valgus alignment, and the extent of the fracture comminution.
The Baumann angle (Humeral capitular angle) on AP view
- Angle between line perpendicular to long axis of humeral shaft and the physeal line of the capitulum, is used to assess varus or valgus alignment of the distal humerus.
- Normal range – 64º to 82º degrees
- Decrease in angle – varus angulated fracture with possible medial column comminution
The Ulnohumeral angle or radiological carrying angle on AP view
- The angle formed by the diaphyseal axis of the humerus and the axis of the proximal third of the ulna.
- It is also used to assess varus or valgus deformity and it is more accurate and useful than Baumann’s angle [3]
Classification of Supracondylar fracture[edit | edit source]
Modified Gartland classification( 2006)of supracondylar fractures (based on lateral radiograph):[6][5]
Type I
- Nondisplaced or minimally displaced (<2mm) with intact anterior humeral line
- No disruption of periosteum – stable fracture
- Fat pad signs may be only finding
Type II
- Displaced (>2mm) with hinged intact posterior cortex
- Anterior humeral line does not pass through middle third of capitellum on lateral radiographs
- No rotational deformity on AP radiograph
Type III
- Displaced with no meaningful cortical contact, usually sagittal plane extension and frontal/horizontal plane rotation
- Significant periosteum disrupture, soft tissue and neurovascular injuries common
- Medial column comminution and collapse with malrotation in frontal plane
Type IV
- Multidirectional instability
- Incompetent periosteal hinge circumferentially, with instability in flexion and extension
Outcome Measures[edit | edit source]
add links to outcome measures here (see <a href="Outcome Measures">Outcome Measures Database</a>)
Management / Interventions[edit | edit source]
Closed reduction and pin fixation is the most common treatment and is the indicated initial treatment for nearly all displaced closed fractures. Criteria for successful reduction include Braumann angle >10 degrees, intact medial and lateral columns, and anterior humeral line through middle third of capitellum.[6] Kirschner wires are commonly used to hold reduced fracture and arm is immobilized (between 40-60 degrees flexion).[6] With failed closed reduction, open fractures, and limb vascular compromise open reduction is the indicated treatment method. Anterior or lateral approach may be used, while posterior approach is not recommended due to significant rates of limited motion and osteonecrosis of trochlea. In-hospital traction is no longer a commonly used treatment technique given the outcomes and minimal hospital stay with closed reduction.[6]
Type I
- Immobilization with long cast (60-90 degrees flexion) for ~3weeks
- Radiographic check at 1 and 2 weeks
Types II, III, and IV
- Operative reduction and pin fixation
Differential Diagnosis[edit | edit source]
Common complications and associated injuries:
- Vascular injury
- Compartment syndrome
- Neurologic injury
- Open or associated forearm fractures
- Medial or lateral column collapse
- Cubitus varus deformity
Physiotherapy for a supracondylar fracture[edit | edit source]
Physiotherapy treatment is vital in all patients with a supracondylar fracture to hasten healing and ensure an optimal outcome. Treatment may comprise:[7]
soft tissue massage
joint mobilization
electrotherapy (e.g. ultrasound)
taping or bracing
exercises to improve strength and flexibility
education
activity modification
a graduated return to activity plan
Exercises for a supracondylar fracture[edit | edit source]
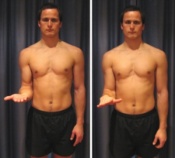
The following exercises are commonly prescribed to patients with a supracondylar fracture following confirmation that the fracture has healed, and that the orthopaedic specialist has indicated it is safe to begin mobilization. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 3 times daily and only provided they do not cause or increase symptoms.
Elbow Bend to Straighten[edit | edit source]
Bend and straighten your elbow as far as possible pain free (figure 3). Aim for no more than a mild to moderate stretch. Repeat 10 times provided there is no increase in symptoms.
Forearm Rotations[edit | edit source]
Begin this exercise with your elbow at your side and bent to 90 degrees (figure 4). Slowly rotate your palm up and down as far as possible pain free. Aim for no more than a mild to moderate stretch. Repeat 10 times provided there is no increase in symptoms.
Tennis Ball Squeeze[edit | edit source]
Begin this exercise holding a tennis ball (figure 5). Squeeze the tennis ball as hard as possible and comfortable without pain. Hold for 5 seconds and repeat 10 times.
References[edit | edit source]
- ↑ 1.0 1.1 Gray H. Anatomy of the human body. Lea & Febiger; 1878.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Kumar V, Singh A. Fracture supracondylar humerus: A review. Journal of clinical and diagnostic research: JCDR. 2016 Dec;10(12):RE01.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Vaquero-Picado A, González-Morán G, Moraleda L. Management of supracondylar fractures of the humerus in children. EFORT open reviews. 2018 Oct;3(10):526-40.
- ↑ 4.0 4.1 Zhang XN, Yang JP, Wang Z, Qi Y, Meng XH. A systematic review and meta-analysis of two different managements for supracondylar humeral fractures in children. Journal of orthopaedic surgery and research. 2018 Dec 1;13(1):141.
- ↑ 5.0 5.1 Brubacher JW, Dodds SD. Pediatric supracondylar fractures of the distal humerus. Curr Rev Musculoskelet Med 2008;1:190-196.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am 2008;90:1121-32.
- ↑ http://www.physioadvisor.com.au/13642350/supracondylar-fracture-fractured-humerus-physi.htm physio advisor take control of your injury