Sundowning
Original Editor - User:Akano Oluwadara Tomisin
Top Contributor- ADHIRA MAHAJAN
Introduction[edit | edit source]
Sundowning refers to a group of neuropsychiatric symptoms which develop late afternoon or during the evening and night time ( periods of diminishing daylight). It is commonly seen in individuals diagnosed with dementia or neurocognitive decline due to parkinson's or alzheimer's disease and in elderly institutionalized patients[1].
Some of the common symptoms associated with sundowning include:[2]
- Confusion
- Anxiety
- Aggression
- Irritability
- Hallucination
- Pacing
- Wandering
- Changes in demeanour and affect
- Motor changes like restlessness, dyskinesia
Sundowning can negatively impact patient safety and wellbeing and results in considerable caregiver burnout. It also poses increased demands on the health care providers especially nursing staff.[3]
Etiology of Sundowning[edit | edit source]
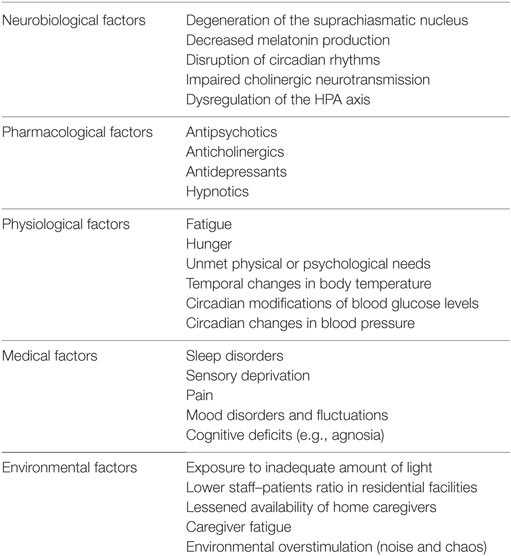
The etiology of Sundowning is complex and poorly understood.Changes in the normal circadian rhythm is one of the most common cause of sundowning, however other factors like medications, environmental changes, comorbidities all play a significant role in development of disruptive behaviours seen in sundowning. Some of the common factors are summarized in Table 1.
Table 1." Factors that have been associated with the pathophysiology and clinical occurrence of sundowning among persons with dementia" ( Canevelli M, Valletta M, Trebbastoni A, Sarli G, D’Antonio F, Tariciotti L, de Lena C, Bruno G. Sundowning in dementia: clinical relevance, pathophysiological determinants, and therapeutic approaches. Frontiers in medicine. 2016 Dec 27;3:73.
Treatment of Sundowning[edit | edit source]
The treatment for sundowning requires a team based approach. Coordination between the health care providers, patient and the family members is quintessential. The treatment can be broadly divided between Pharmacologic and Nonpharmacologic approaches.
- Pharmacological Treatments: The three groups of drugs that have shown some promise for the management of sundowning are: Melatonin supplementation, cholinesterase inhibitors and antipsychotics[3]. However, more research is required.
- Non Pharmacological Treatments: This should be the first line of treatment for the management of sundowning. The premise of non pharmacological treatments is to design individualised programs and strategies that are tailored to meet patient needs[4]. These include environmental modifications, physical activity, alternate therapy like music, reminiscence therapy, horticulture, spatial and reality orientation.[5]Environmental modifications include: installing sky like tiles, progressive dimming of lights in the evening, avoiding loud noise like television during bed time, maintaining consistent routine, avoiding caffeine, installing big clocks, different coloured clothing for bed time and day time wear, soothing music during evening time can help with managing symptoms of sundowning.[4]A combination of aerobic exercise and cognitive training has shown some promise in reducing cortisol levels and thus improving the Hypothalamic Pituitary axis responsible for circadian rhythm.[6]
Physiotherapy Management[edit | edit source]
- Physiotherapists can help by educating caregivers and family members on environmental modifications, maintaining symptom logs to assess for common themes or patterns associated with sundowning.
- Incorporating fall prevention strategies to help keep the patient safe.
- Designing functional exercise interventions.
- Using two dimensional floor and door patterns or adding stop signs to to prevent wandering or exit seeking behaviour[7].
- Pain management.
References[edit | edit source]
- ↑ Khachiyants N, Trinkle D, Son S, Kim K. Sundown syndrome in persons with dementia: an update. Psychiatry investig, 2011; 8:275-87
- ↑ Menegardo CS, Friggi FA, Scardini JB, Rossi TS, Vieira TD, Tieppo A, Morelato RL. Sundown syndrome in patients with Alzheimer’s disease dementia. Dementia & neuropsychologia. 2019 Dec 9;13:469-74. BibTeXEndNoteRefManRefWorks
- ↑ 3.0 3.1 Canevelli M, Valletta M, Trebbastoni A, Sarli G, D’Antonio F, Tariciotti L, de Lena C, Bruno G. Sundowning in dementia: clinical relevance, pathophysiological determinants, and therapeutic approaches. Frontiers in medicine. 2016 Dec 27;3:73.
- ↑ 4.0 4.1 Bautrant T, Grino M, Peloso C, Schiettecatte F, Planelles M, Oliver C, Franqui C. Impact of environmental modifications to enhance day-night orientation on behavior of nursing home residents with dementia. Journal of the American Medical Directors Association. 2019 Mar 1;20(3):377-81.
- ↑ Hsu TJ, Tsai HT, Hwang AC, Chen LY, Chen LK. Predictors of non‐pharmacological intervention effect on cognitive function and behavioral and psychological symptoms of older people with dementia. Geriatrics & gerontology international. 2017 Apr;17:28-35.
- ↑ Venturelli M, Sollima A, Cè E, Limonta E, Bisconti AV, Brasioli A, Muti E, Esposito F. Effectiveness of exercise-and cognitive-based treatments on salivary cortisol levels and sundowning syndrome symptoms in patients with Alzheimer’s disease. Journal of Alzheimer's Disease. 2016 Jan 1;53(4):1631-40.
- ↑ Hewawasam L. Floor patterns limit wandering of people with Alzheimer's. Nursing Times. 1996 May 1;92(22):41-4.