Sundowning: Difference between revisions
No edit summary |
(Added new information and refrences) |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Akano Oluwadara Tomisin]] | '''Original Editor '''- [[User:Akano Oluwadara Tomisin]] | ||
| Line 9: | Line 7: | ||
== Introduction == | == Introduction == | ||
[[File:Sundowning 2.jpg|thumb]] | [[File:Sundowning 2.jpg|thumb]] | ||
Sundowning refers to a group of neuropsychiatric symptoms | Sundowning refers to a group of neuropsychiatric symptoms which develop late afternoon or during the evening and night time ( periods of diminishing daylight). It is commonly seen in individuals diagnosed with dementia or neurocognitive decline due to parkinson's or alzheimer's disease and in elderly institutionalized patients<ref name=":0">Khachiyants N, Trinkle D, Son S, Kim K. Sundown syndrome in persons with dementia: an update. Psychiatry investig, 2011; 8:275-87</ref>. | ||
Some of the common symptoms associated with sundowning include:<ref>Menegardo CS, Friggi FA, Scardini JB, Rossi TS, Vieira TD, Tieppo A, Morelato RL. Sundown syndrome in patients with Alzheimer’s disease dementia. Dementia & neuropsychologia. 2019 Dec 9;13:469-74. | |||
BibTeXEndNoteRefManRefWorks</ref> Confusion, Anxiety, Aggression, Irritability ,Hallucination, Pacing, Wanderin, Changes in demeanour and affect,Motor changes like restlessness, dyskinesia | |||
Sundowning can negatively impact patient safety and wellbeing and results in considerable caregiver burnout, it also poses increased demands on the health care providers especially the nursing staff.<ref>Canevelli M, Valletta M, Trebbastoni A, Sarli G, D’Antonio F, Tariciotti L, de Lena C, Bruno G. Sundowning in dementia: clinical relevance, pathophysiological determinants, and therapeutic approaches. Frontiers in medicine. 2016 Dec 27;3:73.</ref> | |||
== Etiology of Sundowning == | |||
The etiology of Sundowning is complex and poorly understood.Changes in the normal circadian rhythm is one of the most common cause of sundowning however other factors like medications, environmental changes, comorbidities all play a significant role in development of disruptive behaviours seen in sundowning. | |||
Some of the common factors are summarized in Table 1. | |||
[[File:Fmed-03-00073-t001.jpg|alt=|556x556px]] | |||
Table 1 Table 1." Factors that have been associated with the pathophysiology and clinical occurrence of sundowning among persons with dementia" ( Canevelli M, Valletta M, Trebbastoni A, Sarli G, D’Antonio F, Tariciotti L, de Lena C, Bruno G. Sundowning in dementia: clinical relevance, pathophysiological determinants, and therapeutic approaches. Frontiers in medicine. 2016 Dec 27;3:73. | |||
== Treatment of Sundowning == | == Treatment of Sundowning == | ||
The treatment for sundowning requires a team based approach. Coordination between the health care providers, patient and the family members is quintessential. The treatment can be broadly divided between Pharmacologic and Nonpharmacologic approaches. | |||
* Pharmacological Treatments: The three groups of drugs that have shown some promise for the management of sundowning are: Melatonin supplementation, cholinesterase inhibitors and antipsychotics<ref name=":1">Canevelli M, Valletta M, Trebbastoni A, Sarli G, D’Antonio F, Tariciotti L, de Lena C, Bruno G. Sundowning in dementia: clinical relevance, pathophysiological determinants, and therapeutic approaches. Frontiers in medicine. 2016 Dec 27;3:73.</ref>. However, more research is required. | |||
* | * Non Pharmacological Treatments: This should be the first line of treatment for the management of sundowning. These include environmental modifications, physical activity, alternate therapy like music, acupuncture, taichi , light therapy, consistent routines, caregiver education etc<ref name=":1" /> | ||
* | |||
== References == | == References == | ||
Revision as of 03:53, 16 November 2021
Original Editor - User:Akano Oluwadara Tomisin
Top Contributors - Adhira Mahajan, Akano Oluwadara Tomisin and Kim Jackson
Introduction[edit | edit source]
Sundowning refers to a group of neuropsychiatric symptoms which develop late afternoon or during the evening and night time ( periods of diminishing daylight). It is commonly seen in individuals diagnosed with dementia or neurocognitive decline due to parkinson's or alzheimer's disease and in elderly institutionalized patients[1].
Some of the common symptoms associated with sundowning include:[2] Confusion, Anxiety, Aggression, Irritability ,Hallucination, Pacing, Wanderin, Changes in demeanour and affect,Motor changes like restlessness, dyskinesia
Sundowning can negatively impact patient safety and wellbeing and results in considerable caregiver burnout, it also poses increased demands on the health care providers especially the nursing staff.[3]
Etiology of Sundowning[edit | edit source]
The etiology of Sundowning is complex and poorly understood.Changes in the normal circadian rhythm is one of the most common cause of sundowning however other factors like medications, environmental changes, comorbidities all play a significant role in development of disruptive behaviours seen in sundowning.
Some of the common factors are summarized in Table 1.
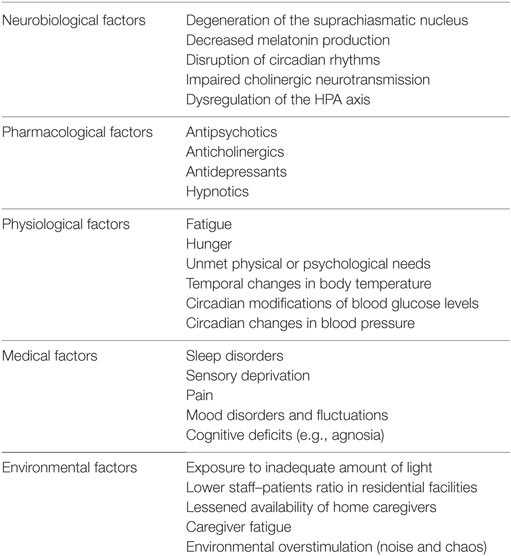 Table 1 Table 1." Factors that have been associated with the pathophysiology and clinical occurrence of sundowning among persons with dementia" ( Canevelli M, Valletta M, Trebbastoni A, Sarli G, D’Antonio F, Tariciotti L, de Lena C, Bruno G. Sundowning in dementia: clinical relevance, pathophysiological determinants, and therapeutic approaches. Frontiers in medicine. 2016 Dec 27;3:73.
Table 1 Table 1." Factors that have been associated with the pathophysiology and clinical occurrence of sundowning among persons with dementia" ( Canevelli M, Valletta M, Trebbastoni A, Sarli G, D’Antonio F, Tariciotti L, de Lena C, Bruno G. Sundowning in dementia: clinical relevance, pathophysiological determinants, and therapeutic approaches. Frontiers in medicine. 2016 Dec 27;3:73.
Treatment of Sundowning[edit | edit source]
The treatment for sundowning requires a team based approach. Coordination between the health care providers, patient and the family members is quintessential. The treatment can be broadly divided between Pharmacologic and Nonpharmacologic approaches.
- Pharmacological Treatments: The three groups of drugs that have shown some promise for the management of sundowning are: Melatonin supplementation, cholinesterase inhibitors and antipsychotics[4]. However, more research is required.
- Non Pharmacological Treatments: This should be the first line of treatment for the management of sundowning. These include environmental modifications, physical activity, alternate therapy like music, acupuncture, taichi , light therapy, consistent routines, caregiver education etc[4]
References[edit | edit source]
- ↑ Khachiyants N, Trinkle D, Son S, Kim K. Sundown syndrome in persons with dementia: an update. Psychiatry investig, 2011; 8:275-87
- ↑ Menegardo CS, Friggi FA, Scardini JB, Rossi TS, Vieira TD, Tieppo A, Morelato RL. Sundown syndrome in patients with Alzheimer’s disease dementia. Dementia & neuropsychologia. 2019 Dec 9;13:469-74. BibTeXEndNoteRefManRefWorks
- ↑ Canevelli M, Valletta M, Trebbastoni A, Sarli G, D’Antonio F, Tariciotti L, de Lena C, Bruno G. Sundowning in dementia: clinical relevance, pathophysiological determinants, and therapeutic approaches. Frontiers in medicine. 2016 Dec 27;3:73.
- ↑ 4.0 4.1 Canevelli M, Valletta M, Trebbastoni A, Sarli G, D’Antonio F, Tariciotti L, de Lena C, Bruno G. Sundowning in dementia: clinical relevance, pathophysiological determinants, and therapeutic approaches. Frontiers in medicine. 2016 Dec 27;3:73.







