Subacromial Pain Syndrome: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 12: | Line 12: | ||
Subacromial (SA) impingement is defined as the clamping of subacromial structures between the coraco-acromial arch and the humerus during the active elevation of the arm above shoulder high. | Subacromial (SA) impingement is defined as the clamping of subacromial structures between the coraco-acromial arch and the humerus during the active elevation of the arm above shoulder high. | ||
== Clinically Relevant Anatomy [[Image:Subacromial structures.jpg|thumb|right]] == | == Clinically Relevant Anatomy [[Image:Subacromial structures.jpg|thumb|right|Subacromial structures.jpg]] == | ||
• the coracoacromial arch<br> --> composed of : acromion, processus coracoideus and ligamentum coracoacromiale<br>• the humerus<br>• the tendons of the [[ | • the coracoacromial arch<br> --> composed of : acromion, processus coracoideus and ligamentum coracoacromiale<br>• the humerus<br>• the tendons of the [[Rotator_Cuff]] <br>• the long head of de M. biceps brachii <br>• the subacromial bursa.[1] <br>• Shoulder capsule | ||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
Revision as of 21:04, 27 June 2011
Original Editor - David Drinkard, Dorien De Strijcker
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Search Strategy[edit | edit source]
Key Words: Complications - Diagnosis - Drug therapy - Epidemiology - Etiology - Pathology - Prevention and control - Rehabilitation - Surgery - Therapy - Ultrasonography / Subacromial impingement
Search engines : Pubmed (http://www.ncbi.nlm.nih.gov/pubmed) / web of knowledge
Limits : Humans - Published in the Last: 3 years
Free text words: Hawkins-Kennedy test
Definition/Description[edit | edit source]
Subacromial (SA) impingement is defined as the clamping of subacromial structures between the coraco-acromial arch and the humerus during the active elevation of the arm above shoulder high.
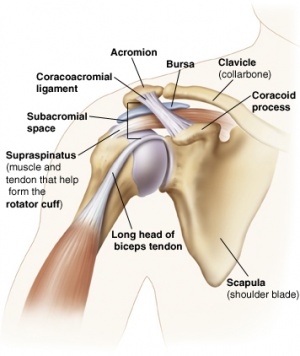
Clinically Relevant Anatomy [edit | edit source]
• the coracoacromial arch
--> composed of : acromion, processus coracoideus and ligamentum coracoacromiale
• the humerus
• the tendons of the Rotator_Cuff
• the long head of de M. biceps brachii
• the subacromial bursa.[1]
• Shoulder capsule
Epidemiology /Etiology[edit | edit source]
The shape of the acromion can cause irritation of the subacromial structures. There are 3 types:
1. Type I: Flat (Least likely to contribute)
2. Type II: Curved
3. Type III: Hooked shape (Most likely to contribute)
A variety of causes could acting together and be on the origin of the impingement syndrome, causes like:
• inflexibility, fatigue, mechanical errors and even technique errors [3]
• Rotator cuff weakness, causing the humeral head to drift more superior
• Chronic rotator cuff irritation due to overuse
• Posterior GH capsule tightness
• Anatomical variations such as narrow SA space, Type II or III Acromion, or subacromial osteophyte
• Poor posture (forward shoulder posture can cause functional narrowing of SA space)
• Abnormal muscle activiation
Clinical Presentation[edit | edit source]
Individuals with subacromial impingement will usually complain of pain with active elevation of the shoulder. This shoulder pain is usually reported at the anterior or lateral side of the shoulder. Activities performed with the involved arm below shoulder level are often not painful because the subacromial structure are not impinged when the shoulder is in anatomic position. These individuals often do not remember a traumatic incident as the onset is more of a gradual, degenerative condition rather than due to a strong external force. People with subacromial impingement syndrome complain in the first stage of moderate pain that occurs during exercise. However, there is no loss of strength and no limitation in movement. At this stage, the damage to the structures may well be fixed with a conservative treatment. The second stage will involve pain that occurs during ADL-activities and especially during the night. From here on, there’s a loss of mobility occurred. In the final phase, calcifications occur that provide a strong restriction in movement and less muscle strength. There could be ruptures in tendons of rotator cuff muscles as well. [1]
Diagnostic Procedures[edit | edit source]
The specific diagnosis is often made, based on the history of the patient and a clinical examination. But there are a few technical examination methods to detect this syndrome as well.[2]
X-rays may be used as an extra test which can confirm the diagnosis, but you can’t trust on it as only test. Using X-rays, you can observe sclerosis and osteophyte-formation on the acromion. You can even perceive if the distance between the acromion and the proximal humeral head has become smaller.
Magnetic resonance imaging can show full or partial tears in the tendons of the rotator cuff. Cracks in the capsule may be detected as well. You can also perceive an inflammation of the subacromial bursa and the tendon of the M. supraspinatus.
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
Also see Impingement Cluster page
An accurate history is often one of the best indicators in diagnosing subacromial impingement. However, many diagnostic procedures can be used to validate this diagnosis. The following are a few special tests for the presence of subacromial impingement or tests that are helpful to confirm this SAI:
- Hawkins-Kennedy
- Neer impingement test (useful screening test to rule out SIA)
- Painful Arc (between 60° and 120°) (useful screening and helpful confirming test to rule out SIA)
- Empty can (Jobe) (helpful test to confirm SIA)
- External rotation resistance tests (useful screening and helpful confriming test to rule out SIA)
All these tests are reliable enough for clinical use. But the Painful arc, External rotation resistance test and the Empty can are the most clinical useful tests, based on reliability and diagnostic accuracy.[3]
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
Initially the use of the RICE-method (Rest, Ice, Compression and Elevation) is recommended. Further on, the patient can have non-steroidal anti-inflammatory drugs (NSAIDs) or analgesics as needed. [4]
Treatment of subacromial impingement can be managed either operatively or non-operatively.
Medical Management (current best evidence)[edit | edit source]
Operative treatment usually includes repair of any tissues that have been damaged due to repetitive trauma. Such structures often involve the supraspinatus muscle and/or tendon, proximal biceps tendon, or joint capsule. Removal of the subacromial bursa is a procedure known as a bursectomy. A procedure known as a subacromial decompression (SAD), a surgical decrompession of the subacromial space, is often performed to increase the available space by removing bony spurs, removing the coracoacromial ligament, and even occasionally removing the most inferior portion of the acromion (acromioplasty). Acromioplasty was often used to relieve the pain en increase the range of motion again. The Neer (open) acriomioplasty requires a longer rehabilitation than the arthroscopic acromioplasty, so we prefer the last one. But in addition to surgery, non-operative rehabilitation is good option as well. There is evidence that non-operative rehabilitation, which is supervised, and arthroscopic subacromial decompression both decrease pain in the shoulder and increase function.[5] It can be that some people respond better on physical therapy management, while others respond better on surgery (medical management).
Physical Therapy Management (current best evidence)[edit | edit source]
Non-operative treatment is typically attempted first, assuming there is no significant biceps or rotator cuff tear that will require surgery. There are a lot of conservative treatments available. We can use the RICE-method, NSAIDs (nonsteroidal anti-inflammatory drugs), corticosteroid injections, physical and manual therapy and acupuncture.[4] Shoulder manual therapy techniques have been shown in multiple studies to be effective for treatment of subacromial impingement. In particular, manual therapy techniques have been shown to have a significant effect on improving pain levels in patients with SAI. Although exercise therapy alone has been shown to bring decreased pain, the addition of manual therapy further augments those gains and also aids in greater strength gains than exercise alone[6]. Thoracic spine thrust manipulation has been shown to be effective in producing short-term increases in subjective reports of function and decreases in pain in individuals with SAI[7]
There are other modalities as well to relieve the pain, but we don’t know if these modalities speed up the healing. We can use electronic stimulation, these impulses stimulates the muscles and therefore these muscles get more blood. Another common used modality is ultrasound. These ultrasonic waves goes through the skin and the muscles and bounces back on the bones. This causes a mechanical vibration in the muscle, that gives the patient a soothing effect. Low-level laser-therapy can be used as well, which seems to have a positive influence on all the symptoms except for muscle strength. [8]Acromioplasty and/or manual therapy may be used alongside therapeutic exercise to improve functional and impairment-level gains, depending on severity of anatomic dysfunction involved. Although exercise treatment is a vital part of treatment for this condition, results showed no significant difference between home-based exercises and clinical exercise. Once manual therapy is no longer necessary and the patient has an adequate home exercise program, forma therapy is often no longer necessary. A website on which a physiotherapist easily can find some simple exercises a patient can do at home is: Revalidatie Herentals. This is a website of a Belgian hospital that is specialized in shoulder disorders. Therapeutic exercise should include rotator cuff strengthening, lower and middle trapezius strengthening, and anterior and posterior shoulder stretching.[9]. It’s all about strengthening and stretching those muscles. Lower trap strengthening is important because individuals with impingement syndrome have been shown to demonstrate greater ratios of upper trap/lower trap activation than asymptomatic individuals[10]. Soft tissue mobilization to normalize muscle spasm and other soft tissue dysfunction has been shown to be effective alongside joint mobilizations to restore motion in treatment of SAI[11] There are no data available which can guarantee that surgical treatment is more effective than conservative treatment.[12]
Differential Diagnosis
[edit | edit source]
There are a variety of shoulder conditions that can initially be confused with subacromial impingement, although a thorough examination is usually sufficient for identifying this condition. There are many conditions that could give a positive impingement test while there's no subacromial impingement. Partial and full rotator cuff tears are or rotator cuff tendinitis are often the result of subacromial impingement syndrome, but can occur without impingement and usually demonstrate some sort of lag sign upon evaluation. Adhesive capsulitis, or "frozen shoulder", can also present with limitation of active shoulder elevation and significant shoulder pain; however, adhesive capsulitis usually presents with glenohumeral motion loss in a capsular pattern, meaning that external rotation and abduction are the two directions with the greatest magnitude of motion lost. Although subacromial impingement syndrome is often confused with adhesive capsulitis. Further on, calcific tendinitis and an acute or chronic inflammation of the bursa subacromialis could be differential diagnosis, as well as a subluxating shoulder or thoracic outlet syndrome. [1]
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1VsHRGSo3HXVCiE3YsXdoVtjngMaV1dlFS8HD8_1UNglqkq9z-|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 Cite error: Invalid
<ref>tag; no text was provided for refs namedboek - ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedKromer et al - ↑ MICHENER L.A., WALSWORTH M.K., DOUKAS W.C., MURPHY K.P. Reliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests for Subacromial Impingement. Archives of Physical Medicine and Rehabilitation. 2009 Nov; 90(11): 1898-903
- ↑ 4.0 4.1 DORRESTIJN O., STEVENS M., WINTERS J.C., VAN DER MEER C., DIERCKS R.l. Conservative or surgical treatment for subacromial impingement syndrome? A systematic review. Journal of shoulder and elbow surgery board of trustees. 2009 Jul-Aug;18(4):652-60
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedTate et al - ↑ Bang MD, Deyle GD. Comparison of Supervised Exercise With and Without Manual Physical Therapy for Patients with Shoulder Impingement Syndrome. Journal of Orthopaedic and Sports Physical Therapy. 2000;30(3):126-137.
- ↑ Boyles RE, Ritland BM, Miracle BM, Barclay DM, Faul MS, Moore JH, Koppenhaver SL, Wainner RS. The Short-term effects of thoracic spine thrust manipulation on patients with shoulder impingement syndrome. Manual Therapy. 2009, 14: 375-380.
- ↑ YELDAN I., CETIN E., OZDINCLER A.R. The effectiveness of low-level laser therapy on shoulder function in subacromial impingement syndrome. Disability and rehabilitation. 2009; 31(11): 935–940
- ↑ Kuhn JE. Exercise in the treatment of rotator cuff impingement: A systematic review and synthesized evidence-based rehabilitation protocol. Journal fo Shoulder and Elbow Surgery. 2009;18:138-160.
- ↑ Smith M, Sparkes V, Busse M, Enright S. Upper and Lower trapezius muscle activity in subjects with subacromial impingement symptoms: Is there imbalance and can taping change it? Physical Therapy in Sport. 2009:10, 45-50.
- ↑ Senbursa G, Baltaci G, Atay A. Comparison of conservative treatment with and without manual physical therapy for patients with shoulder impingement syndrome: a prospective, randomized clinical trial. Knee Surg Sports Traumatol Arthoscop. 2007;15:915-921.
- ↑ KUHN J.E. Current evidence fails to show differences in effectiveness between conservative and surgical treatment of subacromial impingement syndrome. The Journal of Bone and Joint Surgery. 2010;92:474
[Category:Musculoskeletal/Orthopaedics]]