Shoulder Mobilization
Original Editor - David Drinkard, Dana Tew.
Top Contributors - Dana Tew, Nupur Smit Shah, David Drinkard, Braden Osman, Admin, Jacob Bischoff, Kim Jackson, Lucinda hampton, Aminat Abolade, 127.0.0.1, Kai A. Sigel, WikiSysop, Tony Varela, Rachael Lowe and Mariam Hashem
Introduction[edit | edit source]
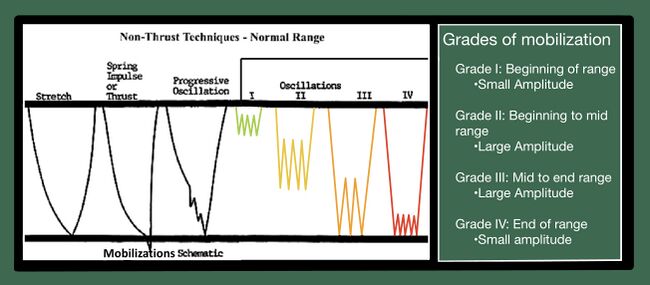
Shoulder mobilization are a key examination tool to assess the integrity of accessory joint motion. Shoulder mobilizations, often utilized in manual therapy, also serve as a treatment procedure and are commonly administered in cases where joint range of motion is restricted. Specific grades of mobilization are described below. Further, a sample of the many mobilization techniques available is described on this page.
The shoulder joint complex is formed by four separate and unique joints, the glenohumeral joint, scapulothoracic joint, sternoclavicular joint, and acromioclavicular joint. The synergistic arthrokinematic movement at each joint allows the shoulder to move through its full range of motion. Passive accessory motion assessment techniques and mobilization techniques for the glenohumeral joint will also be demonstrated and discussed.
Manual therapy interventions for the shoulder have proven to be effective in managing pain and restoring function in individuals with:
- Subacromial Pain Syndrome,
- Adhesive capsulitis
- Rotator cuff tendinopathy.
- Postoperative cases of humerus/clavicle fracture
- Post-traumatic cases of humerus/clavicle fractures
The following techniques are examples of mobilizations that may be seen in clinical practice.
Glenohumeral Mobilizations[edit | edit source]
The humeral head is convex while the glenoid fossa is concave. The treatment plane for mobilizations will often follow the concave surface of the joint. Therefore, the glenoid fossa will be the treatment plane for the glenohumeral joint. Isolating the mobilization to the joint and the joint capsule requires a loose packed position. The loose pack position of the glenohumeral joint is roughly 20° of abduction, 20° of horizontal adduction, slight external rotation or neutral. However, to make sure loose pack position is achieved, palpate the greater tubercle and lesser tubercle at the proximal humerus to ensure joint alignment.
Glenohumeral Distraction[edit | edit source]
Distractions at any joint in loose pack position will facilitate greater mobility with all movements and potentially reduce pain.
Position of the patient: the patient is supine with the shoulder supported in the loose pack position.
Hand placement: The therapist's hand is placed in the axilla with the thumb distal to the joint margin anteriorly and fingers posteriorly. The other hand blocks accessory motion the scapula with the thumb over the coracoid and the fingers on the spine of the scapula.
Direction of Force: The therapists manipulating hand located in the axilla will produce an anterolateral force perpendicular to the glenoid fossa. The therapist can sustain the mobilization or perform oscillations for treatment.
Glenohumeral Inferior Glide[edit | edit source]
Inferior glenohumeral glides facilitate arthrokinematic motions associated with shoulder abduction. Inferior glides may also be used to treat subacromial impingement.
Patient Position: Supine with shoulder in loose pack pack position with the elbow fully extended.
Therapist position: The therapist sits on the plinth placing the patient's UE between the arm of the trunk. The therapist has the option of standing if the patient is brought closer to the edge of the table.
Hand placement: The stabilizing hand will be the more cephalic hand. The hand is to be placed at the radial border and the proximal second phalynx will contact the inferior glenoid margin. The manipulating hand will grasp the distal humerus and secure the patient't extremity to their own trunk.
Direction of force: The therapist will turn their own trunk to impart an inferior force along the long axis of the humerus.
Glenohumeral Inferior Glide (progression)[edit | edit source]
Glenohumeral Posterior Glide[edit | edit source]
Posterior glenohumeral glides facilitate the arthrokinematic motions of flexion and internal rotation of the shoulder.
Patient Position: The patient is supine with the shoulder in loose pack position.
Therapist Position: The therapist is standing to the side of the patient in a lunge position leaning forward.
Hand Position: The therapist provides stabilization with the cephalic hand. The cephalic hand will contact the scapula sandwiching it with a thumb on the coracoid and fingers on the spine of the scapula. The stabilization will resist posterior motion of the scapula. The manipulating hand is placed over the humeral head with the thenar and hypothenar eminence of the hand.
Direction of Force: The therapist departs a posterolateral force consistent with the plane of the glenoid fossa.
Glenohumeral Posterior Glide (progression)[edit | edit source]
The posterior glide of the glenohumeral joint can be progressed to increase horizontal adduction or to increase posterior gliding when flexion approaches 90 degrees.
Patient Position: Supine lying position, shoulder flexion up to 90 degrees and internal rotation with elbow flexion.
Hand Placement: The scapula is supported by placing a towel roll beneath it. The therapist places one hand over the proximal humerus for applying grade 1 distraction. Another hand is placed over the elbow joint. The therapist places around the pelvis to distract the humerus.
Direction of Force: The glide is applied on the humerus in the posterior direction by pushing the elbow along the long axis of the humerus.
Glenohumeral Anterior Glide[edit | edit source]
Anterior glenohumeral glides facilitate the arthrokinematic motions of extension and external rotation of the shoulder.
Patient Position: Patient is supine with the shoulder in the loose pack position.
Therapist Position: The therapist stands to the side of the patient in a lunge position leaning forward.
Hand Position: The therapist provides two points of stabilization. The arm closest to the patients body will contact the scapula and coracoid process. The hip closest to the patient's body will contact the distal humerus laterally stabilizing against humeral flexion. The manipulating hand will be on the radial side of the humerus. The second digit and web space between the first two digits contacts the neck of the humerus.
Direction of Force: The therapist imparts a anteromedial force consistent with the plane of the glenoid fossa.
Scapulothoracic Mobilization[edit | edit source]
Scapulothoracic mobilization is performed when there is dysfunction of the scapulothoracic articulation (e.g. restriction of upward rotation or lateral glide). Mobilizations that are commonly used include medial/lateral glides, superior/inferior glides, upward and downward rotation, and diagonal patterns.
- Patient position- typically, the patient is lying side-lying with the involved side up and the arm resting on the therapist's arm. The therapist stands in front of the patient, facing them. Hand contacts for these glides are the inferior angle of the scapula and the acromion. Direction and magnitude of force depend upon the technique being utilized and the desired amount of motion.[2]
References[edit | edit source]
- ↑ Posterior Glide to increase flexion and internal rotation. Available from: https://www.youtube.com/watch?v=At5YYf-LtjU
- ↑ Hertling D, Kessler RM. Management of Common Musculoskeletal Disorders: Physical Therapy Principles and Methods. 4th ed. LW&W, Philadephia, 2006.