Shoulder Bursitis
Top Contributors - Matthias Proost, Dries Meeusen, Lucinda hampton, Vanderpooten Willem, Mariam Hashem, Fasuba Ayobami, Rachael Lowe, Naomi O'Reilly, Kim Jackson, Admin, Wanda van Niekerk, Venus Pagare, Bouzarpour Faryân and Claire Knott </div>
Search strategy
[edit | edit source]
Databases:
Physiopedia: “Gout”; “Osteo-Arthritis”; “Frozen Shoulder”; “Rotator Cuff Tears”; “Dash questionnaire”; “Constant Murley score”; “Adhesive Capsulitis”
PubMed: “Prevalence Shoulder Bursitis”; “Shoulder Bursitis”; “Subacromial Bursitis”; “Scapulothoracic bursitis”; “Therapy Management Shoulder Bursitis”; “Upper Extremity Bursitis”; “Snapping Scapula”
Pedro: “ Shoulder Bursitis”
ResearchGate: “SPADI”;
University of Washington: “SST questionnaire”;
Search words:
shoulder, shoulder bursitis, shoulder bursitis treatment
Definition
[edit | edit source]
Bursitis is a medical condition where a bursa is inflamed and painful. This can lead to reduced mobility and cause problems in daily activities . Bursitis can be the result of a trauma or an overload. In and around the shoulder joint we can distinguish 4 bursae.They function as gliding surfaces to reduce friction between moving tissues of the body and to aid in movement. These tissues can be bone, ligament, muscles and joint capsule. For more information about bursitis, see the physiopedia page of bursitis.
Clinically relevant anatomy[edit | edit source]
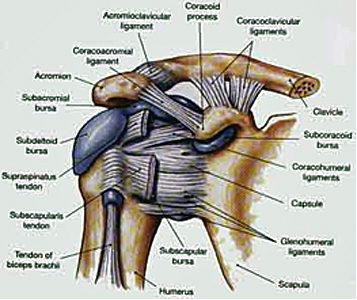
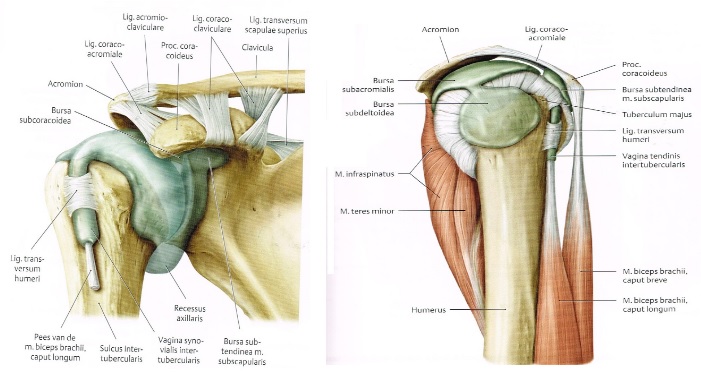
There are 6 bursae in and around the shoulder joint:
1) The subscapular bursa or the scapulothoracic bursa: between the tendon of the subscapularis muscle and the shoulder joint capsule.
2) The Subdeltoid bursa: between the deltoid muscle and the shoulder joint cavity.
3) The Subacromial bursa: below the acromion process and above the greater tubercle of the humerus.
4) The Subcoracoid bursa: between the coracoid process of the scapula and the shoulder joint capsule.
5) The Infraspinatus bursa: between the infraspinatus tendon and the capsule of the joint.
6) The subcutaneous acromial bursa: is located above the acromion just beneath the skin.
The subacromial and the subdeltoid bursa are often taken as a single bursa, the subacromial deltoid bursa.[1 (Level 4)]
Epidemiology/ etiology[edit | edit source]
Several factors can be related to shoulder bursitis: [2 (Level 4)],[3 (Level 4)]
We can distinguish two major kind of causes: Aseptic and septic. In case the bursitis is caused by the presence of bacteria in the bursa, we speak of a septic bursitis.
There are several conditions to get a bursitis;
- Overload: the repetition of a certain motion too often can lead to the inflammation of the bursa because of the friction between the bursa on the one hand and another structure on the other hand. This can be a tendon, bone, a ligament, …
- Trauma: Due to an accident, the bursa could become irritated and become inflamed.
- Inflamed joint: When the whole joint is inflamed, the bursa can become inflamed as well as other structures. We keep in mind arthritis and gout.
A bursitis could also be related to some professional activities (e.g. painter, …), although, this is not always the case in shoulder bursitis.
Characteristics/ clinical presentation[edit | edit source]
Bursitis of the shoulder occurs commonly in people over 30 years old with a greater incidence in females. Younger and middle-aged patients are much more likely to experience acute bursitis than older patients with chronic rotator cuff syndrome. [4 (Level 4)]
No significant difference of incidence was found between men and women specific for subacromial bursitis. [5 (Level 4)]
Subacromial bursitis typically present with lateral or anterior shoulder pain. Patients only occasionally report a single macro traumatic event leading to persistent pain. Overhead lifting or reaching activities are uncomfortable, and the pain is often worse at night, interrupting sleep. In a study focused on the treatment of subacromial bursitis they state that this type of bursitis has the presence of following symptoms: shoulder pain and limitation of movement for longer than one month but less than one year (after one year it becomes chronic bursitis), the presence of pain during at least one activity (such as sleep, dress, work, grooming and sports) and at the end range of at least one ROM test (scapulothoracic tilting, scapulothoracic abduction, glenohumeral flexion, glenohumeral abduction, internal rotation, external rotation) with also a loss of 10 degrees or more in one or more of these tests. [6 (Level 2B)]
Patient who suffer from subacromial bursitis should have a glenohumeral abduction greater than 45 degrees to distinguish from patients with established "frozen shoulders".
Patients who suffer subacromial deltoid or subcoracoid bursitis will experience painful shoulder movements, particularly during activities requiring abduction and extension.
The pain starts gradual, originating deep inside your shoulder and develops over a few weeks or months. The pain is on the outside of the shoulder and may spread towards the elbow.
Activities like washing, where you raise your arm above your head, will worse the pain.
Patients suffering shoulder bursitis may also have interrupted sleep patterns. Rolling over the affected shoulder during sleeping can cause pressure on the inflamed bursa increasing the pain. The pain depends on the degree of inflammation in the shoulder, the range of motion of patients with shoulder bursitis is increased and the shoulder muscles are weaker. [7 (Level 5)], [8 (Level 4)]
Differential diagnosis
[edit | edit source]
Bursitis is frequently caused by another medical condition. For example, patients who suffer from subacromial bursitis, are likely to suffer from adhesive capsulitis, rotator cuff tendinitis, supraspinatus tendinitis or bicipital tendinitis. [9 (Level 4)]
Therefore it is hard to distinguish whether a patient is suffering from bursitis, tendinitis or another injury that usually occurs when the bursa is inflamed. This makes it hard to determine the cause of bursitis when a patient seeks for medical help. One of the methods used by doctors is by extending the arm in front of the body actively. The doctor will try to extend the arm even further away from the patient's body while the patient has to resist this force. If pain occurs, a bursa injury may be the cause of this pain. Nonetheless, this may also mean that indicate a rotator cuff injury or tendinitis, which can give the same kind of pain. The positive impingement test is another example of a diagnostic test, although it doesn’t exclude the other medical conditions that can be confused with bursitis.
To differentiate a bursitis from a supraspinatus tendinitis, which are often confused, we can perform a test to where we isolate the supraspinatus muscle. The patient abducts the arms to 90 degrees with the elbows extended and the arms internally rotated. The arms are placed 30 degrees anteriorly (in the coronal plane), and the patient resists as the examiner forces the arms downward. This is often referred to as the "empty beer can" test.
Frozen shoulder is another medical condition which can be confused with bursitis. In this case, we can differentiate the two symptoms with an easy test: if the patient cannot abduct the arm (glenohumeral abduction), this means the patient has a frozen shoulder. The downside of this test: we can not say with certainty that this patient is suffering from bursitis, only whether this person has a frozen shoulder or not. [10 (Level 2B)]
Diagnostic procedures[edit | edit source]
Bursitis can often be diagnosed by physically examining of the patient. By (visual) inspection it is possible to notice some redness and warmth, local tenderness or stiffness in the joint with some swelling when the inflammation is worse.
By x-ray it is possible to confirm the presence of gout crystals and calcification (which means that the bursitis is chronic or recurrent).
With bursa fluid puncture is it possible to rule out infections.
The subacromial deltoid bursa comes into conflict with the acromion. By executing the painful arc, pain will be felt between 70 and 120 degrees of abduction. When the test is positive, we speak of a bursitis sub acromiodeltoid. The movement restriction is not in accordance with the capsular pattern. This means that the abduction is more restricted than the exorotation.
The subcoracoid bursa stands in relation with the anterior joint capsule. We speak of an subcoracoid bursa when the passive exorotation in 90 degrees of abduction is negative and the passive exorotation on 0 degrees is positive.
A test for the scapulothoracic bursa focusses on the strength of the scapular muscles—including the trapezius (upper, middle, and lower), levator scapula, serratus anterior, latissimus dorsi, deltoids, and rotator cuff muscles. A loss of muscle tone or an alteration of scapulothoracic rhythm may lead to increased friction between the medial border of the scapula and the rib cage, resulting in crepitus or snapping.
Snapping scapula is a painful crepitus of the scapulothoracic articulation. This crepitus is a grinding or snapping noise with scapulothoracic motion that may or may not accompany pain. This condition is commonly seen in overhead-throwing athletes. Treatment of patients with this syndrome begins with nonoperative methods; when nonoperative treatment fails, several surgical options exist. [11 (Level 1A)], [12 (Level 3A)]
Outcome measures[edit | edit source]
The Visual Analogue Scale is filled in by the patient. It is a scale used to describe the pain after the joint is palpated by the physiotherapist.
The DASH-questionnaire, Disability in Arm, Shoulder and Hand-questionnaire, is a 30-item questionnaire that looks at the ability of a patient to perform certain upper extremity activities. This questionnaire is a self-report questionnaire where patients can rate difficulty and interference with daily life on a 5 point Likert scale.
The Shoulder Pain and Disability Index (SPADI) was made to measure shoulder pain and disability. The SPADI contains thirteen items: five of them question pain, eight of them measure disability. The second version of this questionnaire was established to make the tool easier, and the tests take less than 5 minutes to complete.
The Constant-Murley score (CMS) is a 100-points scale composed of a number of individual parameters. These parameters define the level of pain and the ability to carry out the normal daily activities of the patient. The Constant-Murley score was introduced to determine the functionality after the treatment of a shoulder injury. The test is divided into four subscales: pain (15 points), activities of daily living (20 points), strength (25 points) and range of motion: forward elevation, external rotation, abduction and internal rotation of the shoulder (40 points). The higher the score, the higher the quality of the function.
Another scale which we can use is the Shoulder Disability Questionnaire (SDQ). It contains 16 questions about your daily life where shoulder pain can occur. The scale questions you physical, social and emotional restrictions. Using this questionnaire, a functional status of symptoms (pain and / or restricted movement) in the shoulder region can be made.
We can also use the Simple Shoulder Test questionnaire (SST). This is a 12-questions scale about the functioning of the shoulder which the patient must answer with yes or no. The results of this test gives us the possibility to compare the functioning of the shoulder before and after treatment.
Physical examination
[edit | edit source]
Bursitis can often be diagnosed by physically examining of the patient. By (visual) inspection it is possible to notice some redness and warmth, local tenderness or stiffness in the joint with some swelling when the inflammation is worse.
Physical examination of the subacromial bursitis reveals a reduced active range of motion with decreased elevation, internal rotation and abduction, primarily because of pain. The most painful arc of motion is between 70 and 120 degrees of abduction. Tenderness is found laterally below the acromion, anteriorly at the insertion of the supraspinatus tendon on the greater tuberosity and, occasionally, along the supraspinatus muscle belly beneath the trapezius. Strength testing may reveal weakness with internal and external rotation, a finding that demonstrates an important factor in the etiology of these injuries: functional instability due to rotator cuff weakness.
The impingement signs are usually positive. The Neer's sign is performed by forcibly forward flexing the internally rotated arm maximally above 90 degrees. The Hawkin's impingement sign refers to forced internal rotation of the arm performed during forward elevation to 90 degrees. Both tests are considered positive if they produce pain.
Medical management[edit | edit source]
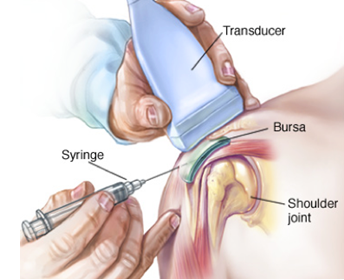
A common treatment for bursitis is the use of injections with or without the use of ultrasound guidance or palpation. These injections could contain steroids or other analgesic substances.
One study examined the use and effectiveness of botulinum toxin type B in the treatment of subacromial bursitis or shoulder impingement syndrome. The conclusion was that botulinum type B can be a useful strategy and that it has a great potential for replacing steroids as a treatment for subacromial bursitis or shoulder impingement syndrome. [13 (Level 1B)]
Inflammation can also be treated with anti-inflammatory medications such as Motrin, Advil, Aleve, Celebrex, or one of many others. These all fall within the category of 'non-steroidal anti-inflammatory medications.' Taken by mouth, these medications help with the inflammation of the tendons and bursa, and also help reduce the discomfort. [14 (Level 4)]
Since the appearance of bursitis is due to another medical condition, treating the cause of this bursitis should be the first step. But since the bursa is still painful, injection is often used to cure this pain. This injection can be in the bursa, or in the muscle itself. A recent study has shown that both methods reduce the pain, but there’s no significant difference between the two methods. [15 (Level 1B)]
Physical therapy management
[edit | edit source]
Immediate treatment: discontinue all activity, RICE regime to reduce inflammation and treat pain. Then heat to promote blood flow and healing. [16 (Level 4)]
The aim of the therapy:
1) Reduce the symptoms
2) Minimize damage
3) Maintain rotator cuff motion and strength
The first step in treating bursitis is applying cold to the bursa. It will help decrease the swelling and redness around the bursa.
Apply ice every day 12-20 minutes.
In the acute stage, also use Codman’s pendulum exercises and AAROM exercises. [17 (Level 4)]
Once the inflammation has been reduced, you can begin using ultrasound therapy to continue the healing process. [18 (Level 2A)]
For the best of the recovery, it is designated to keep the joint in motion. This will prevent that the joint becomes stiff and the recovery process is slowed down.
Since the appearance of bursitis is due to another medical condition, treating the cause of this bursitis should be the first step. One of these causes can be a rotator cuff tendinopathy, and so we first have to treat this pathology.
But since the bursa is still painful, injection is often used to cure this pain. This injection can be in the bursa, or in the muscle itself. A recent study has shown that both methods reduce the pain, but there’s no significant difference between the two methods. [19 (Level 1B)]
We can use ultrasound-guided injection or palpation-guided injection. Study shows us that the ultrasound-guided injection is more precisely to find the exact location of the bursa/muscle which we are planning to inject in. [20 (Level 1B)], [21 (Level 1B)]
The best initial approach for a scapulothoracic bursitis is a nonoperative treatment plan that combines scapular strengthening, postural reeducation, and core strength endurance. The addition of local modalities, nonsteroidal antiinflammatory drugs, and localized injections may also be helpful. If an appropriate trial of nonoperative management proves unsuccessful, surgical correction can produce good results. [22 (Level 3A)]
One study focusing on the treatment of subacromial bursitis they examined the difference between one group treated with ultrasound-guided injection (UGI) and another group with ultrasound-guided injection and home exercise program (UGI-exercise) for 1 month. The exercises included exercises for shoulder lowering with decoaptation that the patient must remember to reproduce during all the common daily activities. Another exercise is assisted active self-mobilization for the recovery of range of motion in all directions. Also isometric strengthening with elastic bands of rotator cuff muscles and deltoid was an exercise given to this patients. A last exercise is the stretching in elevation, abduction and rotation performed statically by placing the patient-specific postures that allow the lengthening of the shortened muscles and the recovery of the last degrees of movement. The conclusion in this article is that ultrasound-guided injection combined with shoulder exercises in the treatment of subacromial bursitis is effective to relieve pain in the short and medium term. [23 (Level 1B)]
Once the pain starts to diminish, the physiotherapist will set up an individualized shoulder strengthening and stretching exercise program. It is important to strengthen your muscles properly as they may have weakened during the period of non-use.
Patients with shoulder bursitis can learn ways to move the shoulder that will not cause inflammation. [24 (Level 4)]
Key Evidence[edit | edit source]
Gasparre, Giuseppe, et al. "Effectiveness of ultrasound-guided injections combined with shoulder exercises in the treatment of subacromial adhesive bursitis." Musculoskeletal surgery 96.1 (2012): 57-61. Level of evidence: 1B
Resources[edit | edit source]
Websites:
http://www.webmd.com/pain-management/understanding-bursitis-basics#1
http://www.medicinenet.com/shoulder_bursitis/patient-comments-763-page4.htm
http://www.orthopaedicscore.com/scorepages/disabilities_of_arm_shoulder_hand_score_dash.html
http://www.orthop.washington.edu/?q=patient-care/articles/shoulder/simple-shoulder-test.html
www.err.eg.net/articles/2014/41/4/images/EgyptRheumatolRehabil_2014_41_4_172_147360_t4.jpg
http://www.orthopaedicscore.com/scorepages/constant_shoulder_score.html
http://www.drplace.com/Upper_extremity_bursitis.16.23039.htm
Book:
Moore, et al. Clinical oriented anatomy, 2014, 7th edition
Clinical bottom line[edit | edit source]
Shoulder bursitis is a common cause of shoulder pain. This bursitis is in most cases caused by an overload, trauma, an inflamed joint or elder age as it lays between different structures such as muscles, bones or other structures. Since it’s mostly caused by another pathology nearby, it is very difficult to differentiate these many shoulder pathologies. Pain, a decrease in range of motion, loss of strength and loss of functionality are the main complaints of the patients. There is evidence that injection of pain reducers by using ultrasound guided-injection in combination with physical therapy are beneficial for the recovery.
[edit | edit source]
Warth, Ryan J., Ulrich J. Spiegl, and Peter J. Millett. "Scapulothoracic Bursitis and Snapping Scapula Syndrome A Critical Review of Current Evidence." The American journal of sports medicine 43.1 (2015): 236-245.
Level of evidence: 1A
References[edit | edit source]
[1] Hitzrot, James Morley. "Surgical diseases of the shoulder bursae." Annals of surgery 98.2 (1933): 273.
Level of evidence: 4
[2] Van Alfen N, Van Engelen B, Van Der Tas P, Walravens C, onderzoek en behandeling van de schouder, Bohn stafleu van Loghum,2007.
Level of evidence: 4
[3] H. B. Skinner, Current Diagnosis & treatment in orthopaedics, the McGraw-Hills companies, 2008.
Level of evidence: 4
[4] J. Willis Hurst, Douglas C. Morris, Chest pain, Futura publishing company, 2001.
Level of evidence: 4
[5] Walker-Bone K, Palmer KT, Reading I, Coggon D, Cooper C: Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Rheum 2004, 51:642–651.
Level of evidence: 4
[6] Downing, Deborah Swan, and Arthur Weinstein. "Ultrasound therapy of subacromial bursitis A double blind trial." Physical therapy 66.2 (1986): 194-199.
Level of evidence: 2B
[7] Salzman, Keith L., W. A. Lillegard, and J. D. Butcher. "Upper extremity bursitis." American family physician 56 (1997): 1797-1814.
Level of evidence: 5
[8] Walker‐Bone, Karen, et al. "Prevalence and impact of musculoskeletal disorders of the upper limb in the general population." Arthritis Care & Research 51.4 (2004): 642-651.
Level of evidence: 4
[9] Walker‐Bone, Karen, et al. "Prevalence and impact of musculoskeletal disorders of the upper limb in the general population." Arthritis Care & Research 51.4 (2004): 642-651.
Level of evidence: 4
[10] Downing, Deborah Swan, and Arthur Weinstein. "Ultrasound therapy of subacromial bursitis A double blind trial." Physical therapy 66.2 (1986): 194-199.
Level of evidence: 2B
[11] Warth, Ryan J., Ulrich J. Spiegl, and Peter J. Millett. "Scapulothoracic Bursitis and Snapping Scapula Syndrome A Critical Review of Current Evidence." The American journal of sports medicine 43.1 (2015): 236-245.
Level of evidence: 1A
[12] Conduah, Augustine H., and Champ L. Baker. "Clinical management of scapulothoracic bursitis and the snapping scapula." Sports Health: A Multidisciplinary Approach 2.2 (2010): 147-155.
Level of evidence: 3A
[13] Lee, Jung Hwan, Sang-Ho Lee, and Sun Hong Song. "Clinical effectiveness of botulinum toxin type B in the treatment of subacromial bursitis or shoulder impingement syndrome." The Clinical journal of pain 27.6 (2011): 523-528.
Level of evidence: 1B
[14] Cluett J., Shoulder bursitis treatment, 2009.
Level of evidence: 4
[15] Chang, Won Hyuk, et al. "Comparison of the therapeutic effects of intramuscular subscapularis and scapulothoracic bursa injections in patients with scapular pain: a randomized controlled trial." Rheumatology international34.9 (2014): 1203-1209.
Level of evidence: 1B
[16] Walker B., The anatomy of sports injuries, lotus publishing, 2007, p 131-132
Level of evidence: 4
[17] O. Dreeben, physical therapy clinical handbook, Jones and Barlett, 2008, p209-211.
Level of evidence: 4
[18] Williams, bursitis of the shoulder, home therapy, 2001
Level of evidence: 2A
[19] Chang, Won Hyuk, et al. "Comparison of the therapeutic effects of intramuscular subscapularis and scapulothoracic bursa injections in patients with scapular pain: a randomized controlled trial." Rheumatology international34.9 (2014): 1203-1209.
Level of evidence: 1B
[20] Hsieh, Lin-Fen, et al. "Is ultrasound-guided injection more effective in chronic subacromial bursitis?." Medicine and science in sports and exercise 45.12 (2013): 2205-2213.
Level of evidence: 1B
[21] Chen, Max JL, et al. "Ultrasound-guided shoulder injections in the treatment of subacromial bursitis." American journal of physical medicine & rehabilitation 85.1 (2006): 31-35.
Level of Evidence: 1B
[22] Conduah, Augustine H., and Champ L. Baker. "Clinical management of scapulothoracic bursitis and the snapping scapula." Sports Health: A Multidisciplinary Approach 2.2 (2010): 147-155.
Level of evidence: 3A
[23] Gasparre, Giuseppe, et al. "Effectiveness of ultrasound-guided injections combined with shoulder exercises in the treatment of subacromial adhesive bursitis." Musculoskeletal surgery 96.1 (2012): 57-61.
Level of evidence: 1B
[24] O. Dreeben-Irimia, introduction to physical therapy for physical therapist assistants, 2011, p 84-85.
Level of evidence: 4