Secondary Progressive Multiple Sclerosis - A Case Study: Difference between revisions
Eliana Stein (talk | contribs) No edit summary |
Eliana Stein (talk | contribs) No edit summary |
||
| Line 3: | Line 3: | ||
'''Introduction''' | '''Introduction''' | ||
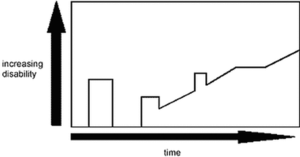
Mrs. X is a 40 year old female with Secondary Progressive Multiple Sclerosis (SPMS). She came into the Multiple Sclerosis (MS) Clinic at Kingston General Hospital (KGH) as an outpatient to seek progression management and manage her current diagnosis of MS. Mrs. X lives with her husband and two adolescent children in a bungalow. Currently, she is equipped with home assisted devices provided by the Occupational Therapist (i.e., raised toilet seat, shower chair, grab bars). Since her diagnosis of MS 10 years ago, Mrs. X has complained of episodes of dizziness and fatigue for years and has noticed some changes in her balance and coordination, along with muscle weakness and spasticity. Due to this, she has experienced recent falls and has increasing difficulty in her ambulation. Mr. X’s disease progression is a characteristic of the disease trajectory and prognosis for someone with SPMS (Figure | Mrs. X is a 40 year old female with Secondary Progressive Multiple Sclerosis (SPMS). She came into the Multiple Sclerosis (MS) Clinic at Kingston General Hospital (KGH) as an outpatient to seek progression management and manage her current diagnosis of MS. Mrs. X lives with her husband and two adolescent children in a bungalow. Currently, she is equipped with home assisted devices provided by the Occupational Therapist (i.e., raised toilet seat, shower chair, grab bars). Since her diagnosis of MS 10 years ago, Mrs. X has complained of episodes of dizziness and fatigue for years and has noticed some changes in her balance and coordination, along with muscle weakness and spasticity. Due to this, she has experienced recent falls and has increasing difficulty in her ambulation. Mr. X’s disease progression is a characteristic of the disease trajectory and prognosis for someone with SPMS (Figure 1). She has also noticed increased pain and reduced sensory deficits. She scored 5.5 on the estimated disability disease steps scale (EDDS) (Figure 2). Mrs. X has also reported a sensitivity to heat and has often complained that she doesn’t enjoy exercising as it makes her tired and is worried it will exacerbate her symptoms. | ||
Many studies have shown to support Mrs. X’s symptoms. Approximately, throughout the course of MS, it is estimated that between 52% and 70% of patients will experience some form of sensory disturbance (Galey et al, 2004). A study done by Galey et al. (2004) studied sensory disturbance in people with MS and found that pain and temperature and vibration deficits were found in the lower extremities, torso and the upper extremities. The study also noted that some of the subjects experienced no sensory deficits; however, for most body parts, the number was quite small (<30%). | Many studies have shown to support Mrs. X’s symptoms. Approximately, throughout the course of MS, it is estimated that between 52% and 70% of patients will experience some form of sensory disturbance (Galey et al, 2004). A study done by Galey et al. (2004) studied sensory disturbance in people with MS and found that pain and temperature and vibration deficits were found in the lower extremities, torso and the upper extremities. The study also noted that some of the subjects experienced no sensory deficits; however, for most body parts, the number was quite small (<30%). | ||
| Line 9: | Line 9: | ||
The literature also showed that people with MS experience visual disturbance, muscle weakness, spasticity and balance issues (Cosh & Carslaw, 2017). | The literature also showed that people with MS experience visual disturbance, muscle weakness, spasticity and balance issues (Cosh & Carslaw, 2017). | ||
The purpose | The purpose of this report is to provide research-derived physiotherapy management for a multiple sclerosis patient. The objectives of this report is to discuss the patient's characteristics, assessment findings, and treatment. | ||
[[File:60198535 1079354775608861 7750295827393806336 n.png|thumb|Figure 1: Increasing disability of secondary progressive Multiple Sclerosis (SPMS). ]] | |||
'''Client Characteristics''' | '''Client Characteristics''' | ||
Revision as of 19:59, 9 May 2019
Abstract
Introduction
Mrs. X is a 40 year old female with Secondary Progressive Multiple Sclerosis (SPMS). She came into the Multiple Sclerosis (MS) Clinic at Kingston General Hospital (KGH) as an outpatient to seek progression management and manage her current diagnosis of MS. Mrs. X lives with her husband and two adolescent children in a bungalow. Currently, she is equipped with home assisted devices provided by the Occupational Therapist (i.e., raised toilet seat, shower chair, grab bars). Since her diagnosis of MS 10 years ago, Mrs. X has complained of episodes of dizziness and fatigue for years and has noticed some changes in her balance and coordination, along with muscle weakness and spasticity. Due to this, she has experienced recent falls and has increasing difficulty in her ambulation. Mr. X’s disease progression is a characteristic of the disease trajectory and prognosis for someone with SPMS (Figure 1). She has also noticed increased pain and reduced sensory deficits. She scored 5.5 on the estimated disability disease steps scale (EDDS) (Figure 2). Mrs. X has also reported a sensitivity to heat and has often complained that she doesn’t enjoy exercising as it makes her tired and is worried it will exacerbate her symptoms.
Many studies have shown to support Mrs. X’s symptoms. Approximately, throughout the course of MS, it is estimated that between 52% and 70% of patients will experience some form of sensory disturbance (Galey et al, 2004). A study done by Galey et al. (2004) studied sensory disturbance in people with MS and found that pain and temperature and vibration deficits were found in the lower extremities, torso and the upper extremities. The study also noted that some of the subjects experienced no sensory deficits; however, for most body parts, the number was quite small (<30%).
The literature also showed that people with MS experience visual disturbance, muscle weakness, spasticity and balance issues (Cosh & Carslaw, 2017).
The purpose of this report is to provide research-derived physiotherapy management for a multiple sclerosis patient. The objectives of this report is to discuss the patient's characteristics, assessment findings, and treatment.
Client Characteristics
Mrs. X is a 40 year old female with Secondary Progressive Multiple Sclerosis (SPMS) and lives in Kingston, Ontario. She doesn’t have any genetic dispositions as MS is not in her family history. Currently, she is working part-time as an accountant due to her limitations in mobility. Mrs. X could benefit from physiotherapy services to help with gait, balance, muscle strength, pain, and a home exercise program. In addition, Physiotherapy services would be able to target functional endurance with day-to-day activities, support independent living, and quality of life in order to reduce her fatigue symptoms.
Examination Findings
Clinical Impression
Physiotherapy Diagnosis:
Secondary Progressive Multiple Sclerosis (SPMS) presenting with decreased balance/coordination, strength, muscle weakness mainly in the LE and fatigue-like symptoms with declining functional mobility.
Problem list
- Fatigue
- Muscle cramps/spasms/weakness/stiffness
- Decreased sensation
- Decreased endurance
- Decreased balance/coordination
- Spasticity
- Fear/avoidance behaviour
- Catastrophizing thinking
Intervention
Outcome
Mrs. X follow- up assessment was conducted 2 months following her initial assessment. Beginning with the MSQOL-54 score, Mrs. X score improved from 43 to 54 for physical health and from 40 to 46 for mental health. The Berg Balance Scale re-assessment showed an improvement from 32 to 42. The Timed 25-foot walk was re-assessed with the mobility aid this time, which decreased her score from 10 seconds to 7 seconds. Her 9-Hole Peg test decreased from 19 seconds to 17 seconds. Lastly, her 12-Item MS walking scale decreased from 50 to 38.
Mrs. X has had fewer falls due to her gait aid and she experiences more stability with the 4WW. She also experienced positive impacts of the HEP (specifically, the walking program) in reducing her fatigue symptoms. In addition, she also had positive impact on her cardiorespiratory fitness and general health.
Mrs. X’s discharge plan should include home-based physiotherapy. The program will include a HEP, including walking, stretching, and resistance training. Her discharge plan also includes a follow-up assessment in 2 months to re-evaluate her symptoms and to track her changes in function and mobility. Re-evaluation will also include follow-up regarding catastrophizing and fear-avoidance beliefs.
Our intervention demonstrated that a short-term outpatient rehabilitation program can improve levels of fatigue, strength, and fitness and can confirm the effectiveness of individualized rehabilitation program for a MS patient.
Discussion
Self study questions
Which of the following is not a type of MS
- Primary Progressive Multiple Sclerosis
- Clinically Isolated Syndrome
- Relapsing-Remitting Multiple Sclerosis
- Secondary Remitted Sclerosis
- All of the above are types of Multiple Sclerosis
The Multiple Sclerosis Quality of Life-54 consists of what major components?
- Physical Health and Mental Health
- Emotional Health, Physical Health, Cognitive Health, and Social Health
- Functional Health and Mobility
- Cardiovascular Ability and Muscular Strength
References
Cosh A, Carslaw H. Multiple sclerosis: symptoms and diagnosis. InnovAiT. 2014 Nov;7(11):651-7. Retrieved from: https://journals.sagepub.com/doi/full/10.1177/1755738014551618
Galey T, Miller C, Nazareth M, Bakshi R, Brownscheidle CM, Weinstock-Guttman B, Moise C, Jacobs L. Sensory Abnormalities in MS: Patient Descriptions of “Macrosomatic Illusions”. International Journal of MS Care. 2004 Dec;6(4):144-7. Retrieved from: https://ijmsc.org/doi/abs/10.7224/1537-2073-6.4.144
Negahban H, Rezaie S, Goharpey S. Massage therapy and exercise therapy in patients with multiple sclerosis: a randomized controlled pilot study. Clinical rehabilitation. 2013 Dec;27(12):1126-36. Retrieved from:https://journals.sagepub.com/doi/full/10.1177/0269215513491586
Karpatkin, HI, Napolione, D and Siminovich-Blok, B. Acupuncture and Multiple Sclerosis: A Review of the Evidence.Evidence-Based Complementary and Alternative Medicine. 2014; 2014: 1-9. Retrieved from: http://dx.doi.org/10.1155/2014/972935.
Kurtzke J.. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33:1444–52. Retrieved from: https://n.neurology.org/content/33/11/1444.short
Potter K, Cohen ET, Allen DD, Bennett SE, Brandfass KG, Widener GL, Yorke AM. Outcome measures for individuals with multiple sclerosis: recommendations from the American Physical Therapy Association Neurology Section Task Force. Physical therapy. 2014 May 1;94(5):593-608. Retrieved form: https://academic.oup.com/ptj/article/94/5/593/2735536
Rose, JW, Houtchens, M, Lynch, SG. (2000). Multiple Sclerosis: Lectures. Retrieved from: https://library.med.utah.edu/kw/ms/clinical_present.html
Wolf BA. Effects of temperature reduction on multiple sclerosis. Physical Therapy. 1970 Jun 1;50(6):808-12. Retrieved from: https://www.researchgate.net/publication/18254241_Effects_of_Temperature_Reduction_on_Multiple_Sclerosis