Salter-Harris Fractures: Difference between revisions
mNo edit summary |
(Updates to anatomy) |
||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Clinically Relevant Anatomy == | ||
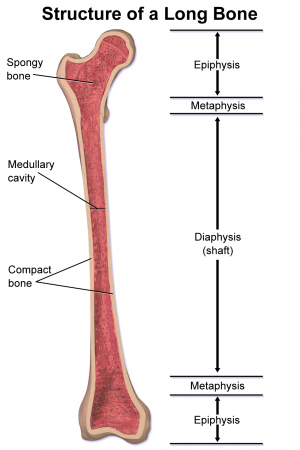
Salter Harris fractures are unique to children because they involve the growth plate | The bones of growing children contain four sections including the diaphysis (shaft), metaphysis, and epiphysis (end). The metaphysis and epiphysis are separated by the physis (growth plate). Salter Harris fractures are unique to children because they involve the growth plate. Cartilage grows from the epiphysis up toward the metaphysis and neovascularization develops from the metaphysis toward the epiphysis. Damage to the vascular supply will disrupt bone development but damage to the cartilage may not cause a problem if it is repositioned appropriately and the vasuclar supply has not been disrupted. | ||
[[File:Structure of a Long Bone.png|thumb|Structure of a long bone including epiphysis, metaphysis, and diaphysis sections.]] | |||
*Type I is a fracture through the growth plate | <br>Salter-Harris fractures are classified into 5 types: | ||
*Type I is a fracture through the growth plate. | |||
*Type II extends through the metaphysis and the growth plate. There is no involvement of the epiphysis. This is the most common of the Salter-Harris fractures. | *Type II extends through the metaphysis and the growth plate. There is no involvement of the epiphysis. This is the most common of the Salter-Harris fractures. | ||
*Type III is a fracture through the growth plate and the epiphysis. This is rare and when it does occur, it is usually at the distal end of the tibia. | *Type III is a fracture through the growth plate and the epiphysis. This is rare and when it does occur, it is usually at the distal end of the tibia. | ||
| Line 14: | Line 17: | ||
*Type V is a crushing type injury that affects the growth plate.<ref name="Moore">Moore W, Smith TH. Salter-Harris Fractures. http://emedicine.medscape.com/article/412956-print</ref> | *Type V is a crushing type injury that affects the growth plate.<ref name="Moore">Moore W, Smith TH. Salter-Harris Fractures. http://emedicine.medscape.com/article/412956-print</ref> | ||
<br> | |||
There are Type VI-Type IX fractures also but these are rare. <br> | There are Type VI-Type IX fractures also but these are rare. <br> | ||
| Line 42: | Line 45: | ||
== Key Evidence == | == Key Evidence == | ||
add text here relating to key evidence with regards to any of the above headings<br> | add text here relating to key evidence with regards to any of the above headings<br> | ||
== Resources == | |||
<br>The following link is a good visual representation of the structures involved in these fractures. [http://emedicine.medscape.com/article/412956-print emedicine.medscape.com/article/412956-print] | |||
== Case Studies == | == Case Studies == | ||
Revision as of 00:14, 25 June 2018
Original Editor - Margaret Layden
Top Contributors - Meaghan Rieke, Admin, Kim Jackson, Margaret Layden, Vidya Acharya and WikiSysop
Clinically Relevant Anatomy[edit | edit source]
The bones of growing children contain four sections including the diaphysis (shaft), metaphysis, and epiphysis (end). The metaphysis and epiphysis are separated by the physis (growth plate). Salter Harris fractures are unique to children because they involve the growth plate. Cartilage grows from the epiphysis up toward the metaphysis and neovascularization develops from the metaphysis toward the epiphysis. Damage to the vascular supply will disrupt bone development but damage to the cartilage may not cause a problem if it is repositioned appropriately and the vasuclar supply has not been disrupted.
Salter-Harris fractures are classified into 5 types:
- Type I is a fracture through the growth plate.
- Type II extends through the metaphysis and the growth plate. There is no involvement of the epiphysis. This is the most common of the Salter-Harris fractures.
- Type III is a fracture through the growth plate and the epiphysis. This is rare and when it does occur, it is usually at the distal end of the tibia.
- Type IV extends through the epiphysis, the growth plate and the metaphysis.
- Type V is a crushing type injury that affects the growth plate.[1]
There are Type VI-Type IX fractures also but these are rare.
Mechanism of Injury / Pathological Process
[edit | edit source]
Salter-Harris fractures are often the result of sports related injuries however they have also been attributed to child abuse, genetics, injury from extreme cold, radiation and medications, neurological disorders, and metabolic diseases which all affect the growth plate according to the National Institute of Arthritis and Musculoskeletal and Skin Diseases.[2]
Approximately 1/3rd of Salter-Harris fractures occur as the result of sports and 1/5th occur from recreational activites.
They may result from a single injury or may be caused by repetitive stresses on the upper and lower extremities.[2]
Point tenderness on palpation at the epiphyseal plate may indicate a fracture. Other signs to look for are persistent pain or pain that affects the child’s ability to tolerate weight bearing through the limb or use of the limb. [2]Soft tissue swelling and/or visible deformity could be another sign of a fracture.[2]
Diagnostic Procedures[edit | edit source]
The diagnostic process begins with obtaining a history of the patients medical status and the mechanism of injury. X-rays will then be obtained but these may be negative. The contralateral limb will be x-rayed as well for comparison.
Magnetic resonance imaging (MRI), computed tomography (CT) and ultrasound may also be used. [2]
Management / Interventions
[edit | edit source]
According to information from NIAMS, Type I and most Type II fractures are treated with cast immobilization although Type II sometimes require surgery. Both normally heal well. Type III disrupts the growth plate and therefore requires surgery. Internal fixation may be required to allow for good alignment. Type IV and Type V are also usually treated with surgery with internal fixation.[3]
Once the fracture has healed the may be referred for physical therapy to restore range of motion and function.
The patient is also seen for assessment of their growth over the next 2 years, usually at 3-6 month intervals.
Approximately 85% of growth plate fractures heal without any long term deficits.
The most common complication of growth plate fractures is early arrest of bone growth which may lead to a short limb or a crooked limb. There is a greater incidence of this at the knee compared to the upper extremity.[2]
Differential Diagnosis
[edit | edit source]
According to Moore et al. ankle fractures, wrist and scaphoid fractures and complications should be considered.[1]
Additionally, as was mentioned previously, one needs to consider medications, radiation, neurological disorders, metabolic disease or exposure to extreme cold especially if no specific injury can be identified.[2]
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
Resources[edit | edit source]
The following link is a good visual representation of the structures involved in these fractures. emedicine.medscape.com/article/412956-print
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1PyjUGRaEF2NUNCZ4fiUgVyJk1SMl2milGuOk0lexHwG6ftE1U: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 Moore W, Smith TH. Salter-Harris Fractures. http://emedicine.medscape.com/article/412956-print
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 National Institute of Arthritis and Musculoskeletal and Skin Diseases. Publication Date October 2001. Revised August 2007.
- ↑ Consumer Health Information Network. arthritis-symptom.com/fracture/salter-harris-fracture.htm