Sacroiliac Joint Force and Form Closure: Difference between revisions
No edit summary |
No edit summary |
||
| Line 150: | Line 150: | ||
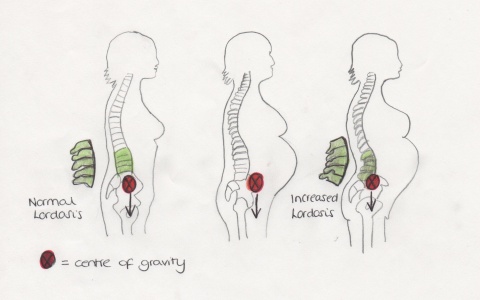
Throughout pregancy the weight of the developing foetus and the uterus increases significantly. It is suggested on average most mothers will gain approximately 11kg in weight, (Ireland and Ott, 2000). This additional load is predominantly carried on the front of the mother's body. To compensate for the increased anterior load, most mothers will adopt an exaggerated lumbar lordosis in standing, (Ritchie 2003, Liebetrau 2012). As the lumbar spine moves into greater extension; the sacrum moves into greater nutation, (Norris 2008). The result of this is increased compression at the SIJ in upright postures. | Throughout pregancy the weight of the developing foetus and the uterus increases significantly. It is suggested on average most mothers will gain approximately 11kg in weight, (Ireland and Ott, 2000). This additional load is predominantly carried on the front of the mother's body. To compensate for the increased anterior load, most mothers will adopt an exaggerated lumbar lordosis in standing, (Ritchie 2003, Liebetrau 2012). As the lumbar spine moves into greater extension; the sacrum moves into greater nutation, (Norris 2008). The result of this is increased compression at the SIJ in upright postures. | ||
| |||
[[Image:Increased_lordosis.jpg|thumb|center|500x300px|Increased lordosis in pregnancy due to increased anterior load.]] | |||
<u>Influence of pregnancy on the ligaments of the SIJ</u> | |||
The increased joint compression assists form closure, however if excess joint compression occurs for a prolonged period of time the mother may develop some sclerosis at the SIJ such as; Osteitis condensana illi, (Mantle, Haslam & Barton, 2004). The sclerotic changes can cause pain and tenderness over the SIJ, which then has a negative impact on form closure, (Mitra, 2009). In most cases the sclerotic changes improve within a number of months post partum, (Mantle, Haslam & Barton, 2004). The current literature suggests the sclerotic changes to the SIJ during pregnancy are most likely to be attributed to the increased mechanical stress on the joint, (Mitra 2009). However there have been suggestions by other authors that reduced blood supply to the illium and various other mechanisms could infact be the primary cause of these changes, (Nicholas, 1975; Haggart & Hare, 1945).<br> | |||
<u></u><u></u><u></u><u></u><u></u><u></u><u></u><u></u><u></u><u></u><u></u><u></u><u>Influence of pregnancy on the ligaments of the SIJ</u> | |||
Progesterone and relaxin are two key hormones released during pregnancy. Both of these hormones are responsible for increasing the elasticity of collagen fibres at various stages in preganacy, (Ireland and Ott 2000). The role of relaxin and progesterone is to increase the extensibility of the ligaments and smooth muscle to allow the pelvis to expand more readily for the delivery of the baby. However as these hormones are released at 10 to 12 weeks into the pregnancy force closure can be greatly affected. This is becasue the ligaments across the joint become lax and therefore do not provide sufficient tension to maintain the joint in it's optimum position, especially during movement, (Ritchie, 2003). | Progesterone and relaxin are two key hormones released during pregnancy. Both of these hormones are responsible for increasing the elasticity of collagen fibres at various stages in preganacy, (Ireland and Ott 2000). The role of relaxin and progesterone is to increase the extensibility of the ligaments and smooth muscle to allow the pelvis to expand more readily for the delivery of the baby. However as these hormones are released at 10 to 12 weeks into the pregnancy force closure can be greatly affected. This is becasue the ligaments across the joint become lax and therefore do not provide sufficient tension to maintain the joint in it's optimum position, especially during movement, (Ritchie, 2003). | ||
Revision as of 21:02, 16 January 2013
Original Editors - Kerry Alexander, Faye Dickinson, Christine McDonagh, Juliet Underwood
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
The Sacro-Iliac Joint[edit | edit source]
The Sacro-Iliac Joint (SIJ) is a synovial joint between the sacrum bone and the ilium bone. Its main roles are to provide stability and offset the load of the trunk to the lower limbs[4]. The SIJ has a high level of stability from the self locking mechanisms of the pelvis, which comes from the anatomy and shape of the bones in the SIJ (Form Closure) and also the muscles supporting the pelvis (Force Closure) [5] [6] Vleeming & Stoeckart)
Movements at the SIJ
The two main movements that occur at the SIJ are nutation and counternutation, and the movements describe the position of the sacrum relative to the iliac bones.
Nutation descibes when the sacrum is rotated forwards relative to the iliac bones.
Counternutation describeswhen the sacrum is rotated backwards relative to the iliac bones.
The amount of movement at the joint is very small and normally amounts to 4 degrees (Vleeming & Soteckart).
According to Willard et al [7]nutation can be regarded as anticipation for joint loading. During nutation the posterior parts of the iliac bones are compressed in the “keystone-like” shape, and the joint is said to be in the locked in the close packed position [8]. This normally occurs during increased load bearing situations e.g. standing and sitting, to increase stability (Vleeming & Soteckart).
Form closure[edit | edit source]
Form Closure describes the stability of the joint from the design of the pelvic anatomy. The sacrum and the ilium have one flat surface [3] and the other surface has ridges which interlock, promoting stability [8]. The symmetrical grooves and ridges allow the highest coefficient of friction of any diarthrodial joint and protect the joint against shearing. The position of the bones in the SIJ creates a “keystone-like” shape which adds to the stability in the pelvic ring. This “keystone” shape is created, as the sacrum has a wider side superiorly which allows the sacrum to be “wedged” in between the ilium. [9]
Force Closure[edit | edit source]
Although form closure provides stability to the SIJ, for mobility to occur further joint compression and stabilisation is required to withstand a vertical load [8] [7]. Force closure is the term used to describe the other forces acting across the joint to create stability (Takasaki et al 2009). This force is generated by structures with a fibre direction perpendicular to the sacroiliac joint and is adjustable according to the loading situation [8]. Muscles, ligaments and the thoracolumbar facia all contribute to force closure [8] [7] [3]; [5]; [4]; Harrison, Harrison and Troyanovich, 1997; van Wingerden et al, 2004) Force closure is particularly important during activities such as walking when unilateral loading of the legs creates shear forces [8] [3].
Force closure creates greater friction and therefore increased form closure and what is called “self-bracing” or “self-locking” of the joint. [7] Takasaki et al, 2009; Vleeming et al, 1990a; Vleeming et al, 1990b; Snijders et al 1993 [5]) According to Willard et al [7] force closure reduces the joint’s ‘neutral zone’ thereby facilitating stabilisation.
As the ilium and sacrum only meet for approximately a third of the surfaces, the rest of the stability between the two bones is provided by the ligaments [4].
Ligaments involved in force closure
Table 1 shows the main ligaments in the SIJ involved in force closure.
| Ligaments | Location | Role |
| Sacrotuberous | Attaches to the ilium, sacrum, coccyx and ischium[10] |
Restricts nutation [3]; [11] |
| Sacrospinous | Attaches between the sacrum and anterior longitudinal ligaments in the lumbar spine [11] |
Lowers the ischium in relation to the sacrum [12] |
| Interosseous | Surrounds an iliac protrusion that inserts into a dorsal sacral cavity [11] | ‘The ligament is unlikely to contribute significantly to mechanical restraint of motion.’ It is speculated perhaps it has a proprioceptive role. [13] |
| Long, dorsal sacroiliac | Attaches between the posterior–superior iliac spine and the third and fourth sacral segments [11]. It is the strongest of all the ligaments [7] | Restricts counternutation [11] |
| Iliolumbar | It is a large, fan shape and from the L4/L5 transverse processes the ligament extends laterally to the iliac crest [7] |
Restricts nutation [14] and side bending [7] |
Muscles involved in self-locking mechanism
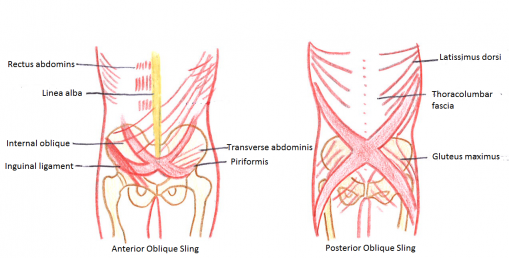
Table 2. shows three muscle slings that contribute to force closure of the SIJ, the longitudinal, posterior oblique and anterior oblique slings.
| Name of Sling: | Components of sling: | Action on SIJ: |
|
Longitudinal
|
• Multifidus attaching to the sacrum • Deep layer of thoracolumbar facia • Long head of biceps femoris attaching to the sacrotuberous ligament |
• Contraction of the sacral part of the multifidus causes the SIJ to nutate thereby increasing tension in the interosseous and short dorsal ligaments and creating increased force closure of the SIJ. The iliac connections of this muscle along with the erector spinae muscle also pull the posterior sides of the iliac bones toward each other, limiting further nutation. • The muscles of this sling, particulary the multifidus, cause the thoracolumbar fascia to inflate increasing force closure. • Contraction of the erector spinae muscle and the long head of the biceps femoris can help to increase force close due to their anatomical connections with the sacrotuberous ligament. The functions of this ligament have already been described (see Table 1). |
|
Posterior Oblique |
• Latissimus dorsi and contralateral •Biceps femoris |
• These muscles work as synergists to directly stabilise the SIJ. • Force closure can be increased indirectly due to the anatomical connections of the gluteus maximus and the thoracolumbar facia with the sacrotuberous ligament. |
|
Anterior Oblique |
• External oblique • Internal oblique • Transverse abdominus |
• These muscles connect via the rectus sheath and help to increase force closure. |
Pool-Goudzwaard et al 1998; Vleeming et al 2012; Liebenson, 2004; Cohen, 2005; van Wingerden et al, 2004; Pel et al 2008)
If the myofascial slings fail to secure the SIJ this can lead to pelvic pain and dysfuctions. This is discussed further under The effects of Pregnancy on Sacro-iliac joint form and force closure.
Other muscles affecting the SIJ
Deep muscles including the transverse abdominis, the middle part of the internal oblique, multifidus, the diaphragm, the piriformis and the pelvic floor muscles all exhibit anticipatory stabilising contractions prior to large movements. These deep muscles are closer to the centres of rotation of the spine and the SIJ and are therefore able to exert a greater compressive force on the SIJ. ( Vleeming et al 2012; Adams and Dolan, 2007; Richardson et al 2002)
In addition, the pelvic floor muscles oppose lateral movements of the coxal bones thereby stabilising the position of the sacrum between the coxal bones (Pel et al 2008)
Evidence has shown that SIJ stability increases with even slight muscle contraction. (Vleeming et al 2012; van Wingerden et al 2004; Richardson et al 2002)
Even resting muscle activity, as well as active muscle contraction, causes compression of the SIJ joint surfaces.
The Thoracolumbar Fascia
The thoracolumbar fascia is important helping to transfer load from the thoracic cage to the pelvis and lower limbs through the SIJ. The ligaments of the SIJ and many of the surrounding muscles interact with the thoracolumbar fascia and it has been described as a “large transmission belt” (Cohen 2005).
The thoracolumbar fascia is a strong aponeurosis composed of three layers that extends the thoracic region to the sacrum and separates the paraspinal muscles from the muscles of the posterior abdominal wall. (Cohen 2005; Willard et al 2012) The lumbar posterior layer (lumbodorsal fascia) of the thoracolumbar facia attaches to:
• The fascia of the erector spinae
• Internal oblique
• Serratus posterior inferior
• Sacrotuberous ligament
• Dorsal SI ligament
• Posterior iliac spine
• Sacral crest
• Lateral raphe (Harrison et al 1997)
The superficial layer of the thoracolumbar facia supplies a surface for attachment for several upper limb and trunk muscles including:
• Latissimus dorsi
• Gluteus maximus
• Trapzius
It is believed that increased tension in the thoracolumbar fascia can lead to increase compression on the SIJ and therefore increased stability. (Pool-Goudzwaard et al 1998) The tension of the thoracolumbar fascia can be increased in two ways:
1. Contraction of the muscles that are attached to the thoracolumbar fascia.
2. Contraction of the erector spinae muscle and multifidus that ‘inflate’ the thoracolumbar fascia. (Pool-Goudzwaard et al 1998)
Effects of pregnancy on Sacro-iliac Joint Form and Force Closure[edit | edit source]
It is well documented that biomechanical changes occur during pregnancy which can reduce the effectiveness of form and force closure. Several different factors can be responsible for compromising stability at the SIJ. These include:
- altered posture and load bearing
- changes in ligamentous & joint capsule tension
- altered muscle length and reduced muscle strength
- poor muscular co-ordination
Influence of pregnancy on the joint surfaces
Throughout pregancy the weight of the developing foetus and the uterus increases significantly. It is suggested on average most mothers will gain approximately 11kg in weight, (Ireland and Ott, 2000). This additional load is predominantly carried on the front of the mother's body. To compensate for the increased anterior load, most mothers will adopt an exaggerated lumbar lordosis in standing, (Ritchie 2003, Liebetrau 2012). As the lumbar spine moves into greater extension; the sacrum moves into greater nutation, (Norris 2008). The result of this is increased compression at the SIJ in upright postures.
The increased joint compression assists form closure, however if excess joint compression occurs for a prolonged period of time the mother may develop some sclerosis at the SIJ such as; Osteitis condensana illi, (Mantle, Haslam & Barton, 2004). The sclerotic changes can cause pain and tenderness over the SIJ, which then has a negative impact on form closure, (Mitra, 2009). In most cases the sclerotic changes improve within a number of months post partum, (Mantle, Haslam & Barton, 2004). The current literature suggests the sclerotic changes to the SIJ during pregnancy are most likely to be attributed to the increased mechanical stress on the joint, (Mitra 2009). However there have been suggestions by other authors that reduced blood supply to the illium and various other mechanisms could infact be the primary cause of these changes, (Nicholas, 1975; Haggart & Hare, 1945).
Influence of pregnancy on the ligaments of the SIJ
Progesterone and relaxin are two key hormones released during pregnancy. Both of these hormones are responsible for increasing the elasticity of collagen fibres at various stages in preganacy, (Ireland and Ott 2000). The role of relaxin and progesterone is to increase the extensibility of the ligaments and smooth muscle to allow the pelvis to expand more readily for the delivery of the baby. However as these hormones are released at 10 to 12 weeks into the pregnancy force closure can be greatly affected. This is becasue the ligaments across the joint become lax and therefore do not provide sufficient tension to maintain the joint in it's optimum position, especially during movement, (Ritchie, 2003).
There are numerous studies which suggest these hormones, particularly relaxin, can lead to hypermobility at the SIJ during pregnancy due to poor force closure. However a recent systematic review suggests the literature to support this theory is contrasting, and currently there is insufficient evidence to clearly state a direct relationship between increased relaxin concentrations and hypermobility at the SIJ, (Aldabe, 2012).
In addition to the hormonal changes, the increased nutation in standing also impacts on the ligament tension. The posterior ligaments which resist nutation are put under excess stress, (Ritchie, 2003). This can lead to tears within the ligament fibres which will reduce their efficiency to maintain good stability across the joint.
Influence of pregnancy on the abdominal muscles
During pregnancy the abdominal muscles are stretched to allow space for the enlarging uterus, causing rapid lengthening of these muscles (Gilleard and Brown, 1996). This can lead to loss of muscle tone and strength in the abdominal region, with a lengthened position compromising the amount of tension a muscle can produce (Gilleard and Brown, 1996). Weakening of transverse abdominus and the internal obliques may reduce the amount of tension produced in the thoracolumbar fascia, resulting in reduced force closure across the SIJ. However, it has been identified that skeletal muscle fibres add sarcomere to their length when stretched over periods such as 3 weeks, as is the case during pregnancy, and therefore avoid reductions to maximum force production (William and Goldspink, 1978 citied Gilleard and Brown, 1996). This would suggest that it is not changes to the length of the abdominal muscles that primarily reduced their strength during pregnancy. However this study was performed on animals and therefore it is unclear if the results can be generalised to human skeletal muscle fibres. Weakness of transverse abdominus may also occur following Caesarean sections (DiFiore, 2010). Although the abdominal muscles are not cut through during a Caesarean, during a transverse incison the aponeurose is seperated, resulting in bruising and bloating that can disrupt the recruitment of transverse abdominus (DiFiore, 2010).
In some cases the rectus abdominal muscle can be stretched so far laterally that it becomes separated from the linea alba; a condition known as diastasis recti abdominis (Ricci and Kyle, 2009; Gilleard and Brown, 1996). This condition is common in pregnant women, with the majority of incidences occurring during the third trimester and remaining throughout the immediate post-birth period (Boissonnault and Blaschak, 1988). The condition appears to be more common in women with poor abdominal tone prior to pregnancy (Ricci and Kyle, 2009), however, it is believed that all pregnant females are predisposed to diastasis recti abdominis due to the hormonal and biomechanical changes they undergo during pregnancy (Noble, 1982). The increase in maternal hormones during pregnancy results in softening of the linea alba. The increased stretch of the abdominal wall enhances the tension placed on this already weakened tissue, which predisposes the linea alba, and the muscles it supports, to increased risk of injury; leaving the tissue susceptible to separating (Boissonault and Blaschak, 1988). A large diastasis recti abdominis, or distortion of any of the abdominal muscles, can impair the function of the abdominal wall including its role in posture and pelvic stability (Boissonnault and Blaschak, 1988). Gilleard and Brown (1996) found that the ability of the abdominal muscles to support the pelvis against resistance was compromised in pregnant women during the third trimester, and in the majority of cases remained so until at least 8 weeks post birth, when compared to pre-pregnancy abilities (Gilleard and Brown, 1996). The authors noted a change in the angles of insertion of rectus abdominus during the third trimester and concluded that the change this caused to the muscle line of action resulted in the reductions in function capacity (Gilleard and Brown, 1996).
Influence of pregnancy on Muscular Slings
The pelvic nutation that pregnant women adopt may also have an influence on force closure. Continuous nutation will lead to prolonged shortening of the muscles responsible for nutation and lengthening of the muscles responsible for counter-nutation according to the theory of antagonistic pairing (Carnell et al, 2004). If a muscle is shorted or lengthened its force production will be compromised (Knudson, 2007). Some of the muscles responsible for nutation include erector spinae and adductor magnus and some of the counter-nutating muscles include pectineus, adductor longus and brevis and latissimus dorsi (Franklin, 2012). These muscle all contribute to the muscular slings that stabilise the SIJ (Sjodahl, 2010), therefore it is plausible that a reduction in these muscle groups force production may reduce the stability at the SIJ. Piriformus and the hamstrings also contribute within the muscular slings that provide force closure and are known to become shortened during pregnancy (Howard et al, 2000).
The lumbar multifidus also contributes to nutation of the SIJ (Carriere and Feldt, 2006) and may therefore become weakened by prolonged nutation of the pelvis. As multifidus contributes to the tensioning on the thoracolumbar, weakening of this muscle may also act to reduce the force closure of the joint. Lordosis of the lumbar spine can also result in weakening of the abdominal muscles by changing the angle of their pull, and shortening of the thoracolumbar fascia (Howard et al, 2000).
Influence of pregnancy on the Pelvic Floor muscles
Pregnancy and vaginal delivery can lead to dysfunction of the pelvic floor muscles which are classed as local muscles supporting the SIJ (Sjodahl, 2010). It is believed that changes in pelvic floor function as a result of pregnancy can result from damage to the nerves, skeletal muscle and connective tissues (Schussler et al, 1994).
The literature suggests that during pregnancy stretching or pressure on the pudendal nerve can occur as a result of the growing uterus. The pudendal nerve is responsible for innovation of the uterine muscle and therefore over stretching and increased pressure on the nerve can lead to pelvic floor dysfunction as a result of disruptions to the neural signaling. This neuropathy may start during pregnancy and worsen during delivery where further injury to the nerve can occur causing further weakening in the pelvic floor muscles (Viktrup and Lose, 2002).
Changes in the function of the pelvic floor muscles during pregnancy can also result from the influence of hormonal changes on smooth muscles. The increased levels of progesterone present in the body during pregnancy causes relaxation of the pelvic floor muscles and reduced muscle excitability to prevent uterine contraction (Pairman et al, 2010). This can lead to increase stretch and hence weakening of the pelvic floor muscles. Relaxin also causes connective tissue remodelling, with considerable remodelling taking place in the uterine body, cervix and perineal tissue in late pregnancy and parturition, reducing the tensile strength of the tissues (MacLennan et al, 2000).
It is suggested that the type of delivery a female undergoes can also effect pelvic floor function and hence the muscle group’s contribution to the stability of the SIJ. During vaginal deliveries the pelvic floor muscles are stretched maximally to allow for the baby’s head and shoulders to pass out of the vagina, with the pubovisceral muscle being stretched over three times its resting length during the second stage of labour (Lee et al, 2011). This can cause tearing of supportive ligaments and weakening of the pelvic floor muscles which can range from minor weakness to inability to support pelvic organs, resulting pelvic organ prolapse (Kassai et al, 2012). Muscular damage from vaginal tears and episiotomy during labour can also result in scaring, particularly of the puborectalis muscle. This has been reported to impair muscle contractions or even inhibit contractions completely (Schussler et al, 1994). Studies suggest vaginal deliveries that require the aid of instruments such as forceps cause the most significant dysfunction to the pelvic floor muscles (MacLennon et al, 2000). It is suggested that differences in pelvic floor function following birth exist between females who have had vaginal deliveries and those who have had Caesarean sections. A study by Pool-Goudzwaard et al, (2005) found weakening of the pelvic floor contractions following vaginal deliveries when compared to Caesarean section which were characterised by a decrease in muscle endurance. There is conflict in the literature however with MacLennon et al (2000) identifying that although there is a reduced prevalence of pelvic floor dysfunction following a Caesarean Section compared to a vaginal delivery, there was not a significant difference between the two modes of delivery. This was supported by (Lal et al, 2003), suggesting that labour is the cause of pelvic floor disorder regardless of the mode of delivery.
It is likely that instability of the SIJ, and resulting pelvic pain, is multifactorial in cause with contribution from more than one of the structures highlighted (Perkins et al, 1998). Functional instability of the pelvis is thought to be a cause of pelvic girdle pain which is experienced in 14-33% of pregnant women (Sjodahl, 2010).It is possible, however, that some pregnant females are able to compensate for reduced force closure at the SIJ by managing to maintain good pelvic floor function (Pool-Goudzwaard et al, 2005). Literature has suggested that physiotherapy intervention can be an effective treatment for improving SIJ stability following impairments due to pregnancy or labour, (Stuge et al, 2004).
For further information on the assessment and treatment available see sacroiliac joint dysfunction, pregnancy related pelvic pain, lower back pain in pregnancy.
References[edit | edit source]
see adding references tutorial.
- ↑ Liebenson C. The relationship of the sacroiliac joint, stabilization musculature, and lumbo-pelvic instability. Journal of Bodywork and Movement Therapies (2004) 8; 45-45
- ↑ Mitchell T.D, Urli K.E, Breitenbach J & Yelverton C. The predictive value of the sacral base pressure test in detecting specific types of sacroiliac dysfunction. Journal of Chiropractic Medicine 2007 6, 45-55
- ↑ 3.0 3.1 3.2 3.3 3.4 Liebenson C. The relationship of the sacroiliac joint, stabilization musculature, and lumbo-pelvic instability. Journal of Bodywork and Movement Therapies 2004 8; 45-45
- ↑ 4.0 4.1 4.2 Cohen S.P. Sacroiliac Joint Pain: A Comprehensive Review of Anatomy, Diagnosis, and Treatment. Anesthesia &amp;amp;amp; Analgesia 2005: 101:1440-53
- ↑ 5.0 5.1 5.2 Arumugam A, Milosavljevic S, Woodley S &amp;amp;amp;amp;amp;amp;amp; Sole G. Effects of external pelvic compression on form closure, force closure, and neuromotor control of the lumbopelvic spine. A systematic review. Manual Therapy 2012; 17: 275-284 Cite error: Invalid
<ref>tag; name "Arumugam" defined multiple times with different content Cite error: Invalid<ref>tag; name "Arumugam" defined multiple times with different content - ↑ Mitchell T.D, Urli K.E, Breitenbach J &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Yelverton C. ‘The predictive value of the sacral base pressure test in detecting specific types of sacroiliac dysfunction’. Journal of Chiropractic Medicine (2007) 6, 45-55
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 Cite error: Invalid
<ref>tag; no text was provided for refs namedwillard - ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Pool-Goudzwaard A.L, Vleeming A, Stoeckart R, Snijders C. J &amp;Mens J.M.A. Insufficient lumbopelvic stability: a clinical, anatomical and biomechanical approach to ‘a-specific’ low back pain. Manual Therapy. 1998; 3(1): 12-20
- ↑ Willard F.H, Vleeming A, Schuenke M.D, Danneels L &amp; Schleip R. The thoracolumbar fascia: anatomy, function and clinical considerations. Journal of Anatomy 2012; 221(6): 507-36
- ↑ Woodley S.J. &amp;amp;amp; Mercer S.R. Anatomy in practice: the sacrotuberous ligament. NZ Journal of Physiotherapy 2005 33:(3); 91-94
- ↑ 11.0 11.1 11.2 11.3 11.4 Vleeming A, De Vries H.J, Mens J.M.A &amp;amp;amp;amp; Van Wingerden J.P. Possible role of the long dorsal sacroiliac ligament in women with peripartum pelvic pain. Acta Obstet Gynecol Scand 2002 81; 430-436
- ↑ Hammer N, Steinke H, Slowik V, Josten C, Stadler J, Bӧhme J &amp;amp;amp; Spanel-Borowski K. The sacrotuberous and the sacrospinous ligament – A virtual reconstruction. Ann Anat 2009: 191; 417-425.
- ↑ Bechtel R. Physical characteristics of the axial interosseous ligament of the human sacroiliac joint. The Spine Journal 2001: 1; 255-259
- ↑ Pool-Goudzwaard A, HoekvanDijke G, Mulder P, Spoor C, Snijders C & Stoeckart R. The iliolumbar ligament: its influence on stability of the sacroiliac joint. Clinical Biomechanics 2003; 18: 99-105