Resisted Exercise Initiative (RExI)
This article is currently under review and may not be up to date. Please come back soon to see the finished work!
Introduction[edit | edit source]
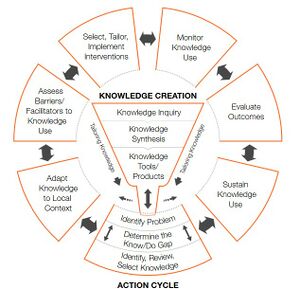
RExI is an abbreviation for the PT Knowledge Broker facilitated project started in April 2019: Resisted Exercise Initiative (RExI) – Use of resisted exercise by physiotherapists for elderly patients in British Colombia (BC) Hospitals.
The current volume and level of acuity of elderly patients in acute care settings challenges physical therapists to address all needs. One related aspect of practice that is receiving increasing attention is the optimal prescription of resistance exercise in these settings.
Goal: To support best practice in use of resisted exercise by physical therapists for elderly patients in BC Hospitals.
Objectives:
- To determine existing practice.
- To identify opportunities to support enhanced practice.
- To undertake knowledge translation (KT) strategies to target barriers to enhance using of resisted exercise.
- To evaluate effect of introduction of the KT strategies.
This project will:
- Describe current practice to confirm whether there is ‘a gap’ between current actual and desired evidence-based practice for PTs in BC.
- Determine the barriers to desired evidence-based practice from the perspective of the front-line public-practice PT.
- Map the barriers identified to categories identified by KT/implementation/behaviour change science.
- Using KT/implementation/behaviour change science and resources to identify targeted KT strategies to address the barriers.
- Develop/undertake, disseminate & support implementation of the targeted strategies.
- Re-evaluate practice post-implementation of the strategies.
Resistance Exercise Tool Kit[edit | edit source]
Definition&Benefits[edit | edit source]
Defined as movement using body weight or external resistance that improves muscular strength ,power , endurance and it may positively impact mobility ,function and independence.[1]
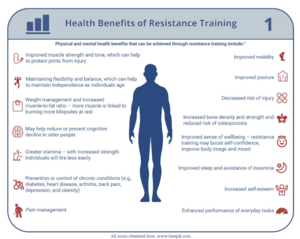
Benefits of resistance exercise ;[2][3]
- Improving muscle strength and tone.
- Maintaining flexibility and balance .
- Weight management and increased muscle to fat ratio.
- May help in prevent or reduce cognitive decline in older people.
- Greater stamina ( people will not tire easily due to improved body strength ).
- Prevention or control of chronic conditions ...eg (back pain, heart disease , arthritis , obesity &depression ).
- Pain management .
- Improved posture and decrease risk of injury.
- Decrease risk of osteoporosis by helping in increasing bone density.
- Improve sense of wellbeing , boost confidence and self-esteem.
A statement from National Strength and Conditioning Association highlighted the benefits of resistance exercise to older people ( Fragala et al .2019).[4]
Aproberly designed resistance training programme can help in :[5]
- Counteracting the age related changes in human skeletal muscle.
- Enhance the muscular strength ,power and neuromuscular functioning of senior citizens.
- Improve older adults resistance to injuries and catastrophic events like : falls.
- Improve mobility , physical functioning , performance of daily activities (ADL) and preserve independence.
- Help in promoting psychosocial well-being of older adults.
Also Fragala et al .2019 recommended the resisted exercise training programme should be matched appropriately to the individuals'abilities and goals.
Considerations & Flags[edit | edit source]
Before prescribing resistance exercise , liaise with patient's physician your treatment plan and discuss the signs and symptoms to monitor :[6][7][8]
| Flags &Contraindications |
|---|
|
- Pain
- Strength
- Function
- Ability to learn
- Comorbidities and medications
- Oxygen Saturation and requirements
- Needs Supervision
- Fatigue Management
- Mobility Assessment
- Hemoglobine (hgb) (monitor patients with levels less than 70g/L)
- Blood Pressure
- HR
- Oxygen Saturation SPO2.
- Platelets
- Physical Activity vital signs (PAVS)*
- Rapid Assessment of Physical Activity *
- Physical Activity Screening for Elderly *
- Risks of coronary Artery Disease
- Uncontrolled hypertension
- People with implanted pacemakers and defibrillators
- Musculoskeletal Limitation
- Joint Pain and Instability (from arthritis or any other causes)
- Diabetes at any age
- Lines
- Aids ( eye wear , hearing aids & gait aids )
Exercise Physiology Foundation[edit | edit source]
1-Muscle strength & life course[edit | edit source]
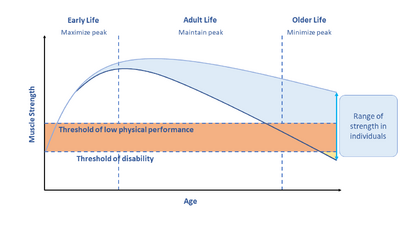
Muscle strength decrease through adult years and life course . There is a strong link between decreased muscle strength and falls,immobility and mortality [4] .
Loss in strength can be moderated by maximizing muscle in early adulthood , maintaining strength in middle age and minimizing loss in older age. This can be achieved through resistance exercise training .[4] [9] *(diagram)
Hospitalized older adults may experience some problems from immobility like: Muscle atrophy , Sarcopenia [9], cachexia.....eg
1- Muscle Atrophy[edit | edit source]
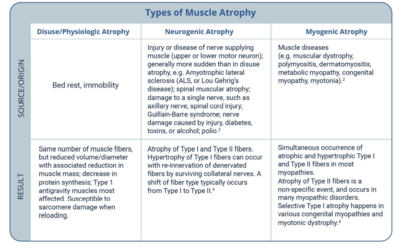
Types of muscle atrophy[10][11]
- Disuse or physiologic Atrophy.
- Neurogenic Atrophy.[12]
- Myogenic Atrophy.
2- Sarcopenia[edit | edit source]
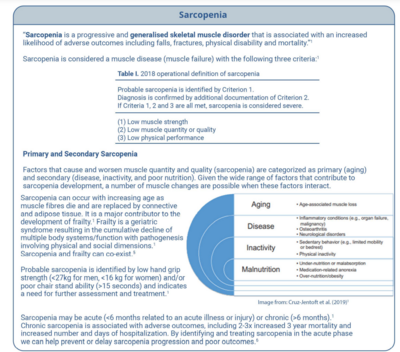
Is defined as a progressive and generalized skeletal muscle disorder associated with an increased likelihood of adverse outcomes like falls, fractures, physical disability and mortality.[9] Sarcopenia is considered a muscle disease ( muscle failure ) with the following 3 criteria :
- Low muscle strength.
- Low muscle quantity and quality.
- Low physical performance.
- Probable sarcopenia is identified by criteria 1.
- Diagnosis is confirmed by additional documentation of criteria 2.
- sarcopenia is considered severe if 1,2 &3 criteria are met.
3- Cachexia[edit | edit source]
Cachexia is a complex metabolic syndrome associated with underlying illness and characterized
by loss of muscle with or without loss of fat mass. The prominent clinical feature of cachexia is weight
loss in adults (corrected for fluid retention) or growth failure in children (excluding endocrine
disorders). Anorexia, inflammation, insulin resistance, and increased muscle protein breakdown are
frequently associated with cachexia. Cachexia is distinct from starvation, age-related loss of muscle
mass, primary depression, malabsorption, and hyperthyroidism and is associated with increased
morbidity.Sarcopenia is one of the factors that may cause cachexia.[13][14]
2-Regeneration Of Injured Skeletal Muscle[edit | edit source]
If the patient has sustained an injury to skeletal muscle, the following information regarding types of muscle injuries and phases of muscle healing may be helpful in planning the progression of resisted exercise.
3- Principles Of Strength and Conditioning[edit | edit source]
References[edit | edit source]
- ↑ Loveless MS, Ihm JM. Resistance exercise: how much is enough?. Current sports medicine reports. 2015 May 1;14(3):221-6.
- ↑ Exercise prescription principles - Exercise.trekeducation.org https://exercise.trekeducation.org/2021
- ↑ American Physical Therapy Association | Choosing Wisely Choosing Wisely | Promoting conversations between providers and patients https://www.choosingwisely.org/societies/american-physical-therapy-association/
- ↑ 4.0 4.1 4.2 Fragala MS, Cadore EL, Dorgo S, Izquierdo M, Kraemer WJ, Peterson MD, Ryan ED. Resistance training for older adults: position statement from the national strength and conditioning association. The Journal of Strength & Conditioning Research. 2019 Aug 1;33(8).
- ↑ Ratamess N. ACSM's foundations of strength training and conditioning. Lippincott Williams & Wilkins; 2021 Mar 15.
- ↑ Kim J, Fanola C, Ouzounian M, Hughes GC, Pyeritz RE, Gleason TG, Evangelista-Masip A, Braverman AC, Montgomery DG, Ehrlich M, Schermerhorn M. ACUTE AORTIC DISSECTION IN PATIENTS WITH MITRAL VALVE DISEASE. Journal of the American College of Cardiology. 2020 Mar 24;75(11_Supplement_1):2255-.
- ↑ Jeevanantham D, Rajendran V, McGillis Z, Tremblay L, Larivière C, Knight A. Mobilization and exercise intervention for patients with multiple myeloma: clinical practice guidelines endorsed by the Canadian Physiotherapy Association. Physical therapy. 2021 Jan;101(1):pzaa180.
- ↑ Stiller K, Phillips A. Safety aspects of mobilising acutely ill inpatients. Physiotherapy theory and practice. 2003 Jan 1;19(4):239-57.
- ↑ 9.0 9.1 9.2 Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E. Sarcopenia: European consensus on definition and diagnosis Report of the European Working Group on Sarcopenia in Older PeopleA. J. Cruz-Gentoft et al. Age and ageing. 2010 Jul 1;39(4):412-23.
- ↑ He N, Ye H. Exercise and muscle atrophy. Physical Exercise for Human Health. 2020:255-67.
- ↑ Ding S, Dai Q, Huang H, Xu Y, Zhong C. An overview of muscle atrophy. Muscle Atrophy. 2018:3-19.
- ↑ Dumitru A, Radu BM, Radu M, Cretoiu SM. Muscle changes during atrophy. Muscle Atrophy. 2018:73-92.
- ↑ Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, Guttridge D, Jatoi A, Kalantar-Zadeh K, Lochs H, Mantovani G, Marks D. Cachexia: a new definition. Clinical nutrition. 2008 Dec 1;27(6):793-9.
- ↑ Ding S, Dai Q, Huang H, Xu Y, Zhong C. An overview of muscle atrophy. Muscle Atrophy. 2018:3-19.