Primary-Progressive Multiple Sclerosis (PPMS) - A Case Study: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
== Abstract == | == Abstract == | ||
'''''Purpose:''''' The case study was designed for Queen’s University PT858 Neurorehabilitation II course. | '''''Purpose:''''' The case study was designed for Queen’s University PT858 Neurorehabilitation II course. The purpose of this fictional case study is to understand and explore an individual diagnosed with Primary Progressive Multiple Sclerosis (PPMS). Additionally, we investigated and applied a research-based treatment approach while integrating the role of technology in rehabilitation. | ||
'''''Case Presentation:''''' This fictional case study focuses on Michelle White a female 47 year old work from home accountant who recently progressed from active primary progressive multiple sclerosis (PPMS) without progression to active PPMS with progression. Her primary complaints were fatigue, difficulty with normal gait, impaired balance, weakness and decreased attention and memory. | '''''Case Presentation:''''' This fictional case study focuses on Michelle White a female 47 year old work from home accountant who recently progressed from active primary progressive multiple sclerosis (PPMS) without progression to active PPMS with progression. Her primary complaints were fatigue, difficulty with normal gait, impaired balance, weakness and decreased attention and memory. | ||
| Line 29: | Line 29: | ||
* '''Medical diagnosis:''' PPMS active with progression | * '''Medical diagnosis:''' PPMS active with progression | ||
** MRI to confirm and identify areas of lesions in the brain | ** MRI to confirm and identify areas of lesions in the brain<ref name=":2" /> | ||
** Positive lumbar puncture test | ** Positive lumbar puncture test | ||
** Positive evoked potentials test<ref>Tsang BK, Macdonell R. [https://www.racgp.org.au/afp/2011/december/multiple-sclerosis-diagnosis-management-and-progno Multiple sclerosis: diagnosis, management and prognosis]. Australian family physician. 2011 Dec;40(12):948-55.</ref> | ** Positive evoked potentials test<ref name=":2">Tsang BK, Macdonell R. [https://www.racgp.org.au/afp/2011/december/multiple-sclerosis-diagnosis-management-and-progno Multiple sclerosis: diagnosis, management and prognosis]. Australian family physician. 2011 Dec;40(12):948-55.</ref> | ||
* '''Treatment to Date:''' No previous history of physiotherapy treatment. | * '''Treatment to Date:''' No previous history of physiotherapy treatment. | ||
* '''Current Symptoms:''' | * '''Current Symptoms:''' | ||
** Impaired mobility | ** Impaired mobility<ref name=":3" /> | ||
** Weakness and stiffness in the legs, the right leg worse than the left. | ** Weakness and stiffness in the legs, the right leg worse than the left.<ref name=":3" /> | ||
** Decreased attention, and memory | ** Decreased attention, and memory<ref name=":3" /> | ||
** Pins and needles in the feet | ** Pins and needles in the feet<ref name=":3" /> | ||
** Urgency incontinence | ** Urgency incontinence<ref name=":3" /> | ||
** Fatigue | ** Fatigue<ref name=":3" /> | ||
** Difficulty with normal gait | ** Difficulty with normal gait<ref name=":3" /> | ||
** Balance impairments<ref>Miller DH, Leary SM. [https://www.thelancet.com/article/S1474-4422(07)70243-0/fulltext Primary-progressive multiple sclerosis]. The Lancet Neurology. 2007 Oct 1;6(10):903-12.</ref> | ** Balance impairments<ref name=":3">Miller DH, Leary SM. [https://www.thelancet.com/article/S1474-4422(07)70243-0/fulltext Primary-progressive multiple sclerosis]. The Lancet Neurology. 2007 Oct 1;6(10):903-12.</ref> | ||
'''''Past Medical History:''''' | '''''Past Medical History:''''' | ||
| Line 55: | Line 55: | ||
'''''Medications:''''' | '''''Medications:''''' | ||
* Oral Paroxetine - 20mg, once a day for depressive symptoms | * Oral Paroxetine - 20mg, once a day for depressive symptoms<ref name=":2" /><ref name=":4" /> | ||
* Norvasc (Amlodipine) - 5mg, once per day for hypertension | * Norvasc (Amlodipine) - 5mg, once per day for hypertension<ref name=":4" /> | ||
* Ocrevus - 600 mg intravenous infusion every six months<ref>[https://mssociety.ca/managing-ms/treatments/medications Medications] [Internet]. MS Society of Canada. (n.d.). [cited 2022May2]. Available from <nowiki>https://mssociety.ca/managing-ms/treatments/medications</nowiki></ref> | * Ocrevus - 600 mg intravenous infusion every six months<ref name=":4">[https://mssociety.ca/managing-ms/treatments/medications Medications] [Internet]. MS Society of Canada. (n.d.). [cited 2022May2]. Available from <nowiki>https://mssociety.ca/managing-ms/treatments/medications</nowiki></ref> | ||
'''''Social History:''''' Michelle lives in Mississauga in a house with 2 steps to get into the house as well as 12 steps to get to the second floor. She lives there with her husband, 2 children and family dog. She has been a work-from-home accountant for the last 15 years. Michelle enjoys working from home but has noticed in the last few months that she has trouble concentrating on her work and thinks her memory has gotten worse. Her family recently moved to Mississauga from Ottawa in the last year, and friends and distant family are still located in Ottawa. Michelle enjoys walking her dog daily, reading and watching movies. However, she finds when she sits in the same position for a long period her pain and discomfort increases. | '''''Social History:''''' Michelle lives in Mississauga in a house with 2 steps to get into the house as well as 12 steps to get to the second floor. She lives there with her husband, 2 children and family dog. She has been a work-from-home accountant for the last 15 years. Michelle enjoys working from home but has noticed in the last few months that she has trouble concentrating on her work and thinks her memory has gotten worse. Her family recently moved to Mississauga from Ottawa in the last year, and friends and distant family are still located in Ottawa. Michelle enjoys walking her dog daily, reading and watching movies. However, she finds when she sits in the same position for a long period her pain and discomfort increases. | ||
| Line 79: | Line 79: | ||
* LE - Table #1 | * LE - Table #1 | ||
{| class="wikitable" | {| class="wikitable" | ||
|+Table #1: Joint Range of Motion | |||
|Joint | |Joint | ||
|Movement | |Movement | ||
| Line 172: | Line 173: | ||
'''''Spasticity''''' | '''''Spasticity''''' | ||
[https://www.physio-pedia.com/Modified_Ashworth_Scale?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Modified Ashworth Scale] | [https://www.physio-pedia.com/Modified_Ashworth_Scale?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Modified Ashworth Scale]<ref>Harb A, Kishner S. [https://www.ncbi.nlm.nih.gov/books/NBK554572/ Modified ashworth scale]. InStatPearls [Internet] 2021 May 9. StatPearls Publishing.</ref> | ||
* UE - WNL | * UE - WNL | ||
* LE - Table #2 | * LE - Table #2 | ||
{| class="wikitable" | {| class="wikitable" | ||
|+Table #2: Modified Ashworth Scale | |||
|Muscle Group | |Muscle Group | ||
|Left Limb | |Left Limb | ||
| Line 214: | Line 216: | ||
|} | |} | ||
'''''Strength''''' | '''''Strength''''' | ||
[https://www.physio-pedia.com/Five_Times_Sit_to_Stand_Test?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal 5 Times Sit to Stand Test]: 7.3 seconds<ref>[https://www.sralab.org/rehabilitation-measures/five-times-sit-stand-test#non-specific-patient-population Five times SIT to stand test] [Internet]. Shirley Ryan AbilityLab. (2013). [cited 2022May 5]. Available from: <nowiki>https://www.sralab.org/rehabilitation-measures/five-times-sit-stand-test#non-specific-patient-population</nowiki></ref> | |||
[https://www.physio-pedia.com/Category:Manual_Muscle_Testing?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Manual Muscle Testing] (MMT) | [https://www.physio-pedia.com/Category:Manual_Muscle_Testing?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Manual Muscle Testing] (MMT) | ||
| Line 220: | Line 224: | ||
* LE - Table #3 | * LE - Table #3 | ||
{| class="wikitable" | {| class="wikitable" | ||
|+Table #3: Manual muscle testing | |||
|Muscle Group | |Muscle Group | ||
|Score Left Limb | |Score Left Limb | ||
| Line 275: | Line 280: | ||
* Reflexes | * Reflexes | ||
** UMN | ** UMN | ||
*** Clonus - postitive | *** [[Clonus of the Ankle Test|Clonus]] - postitive | ||
*** Babinski - positive | *** [[Babinski Sign|Babinski]] - positive | ||
** LMN | ** LMN | ||
*** Patellar - 3/4 | *** Patellar - 3/4 | ||
*** Achilles - 3/4 | *** Achilles - 3/4 | ||
* Sensation testing - decreased pinprick sensation to dorsal feet bilaterally | * Sensation testing - decreased pinprick sensation to dorsal feet bilaterally<ref name=":5">Miehm JD, Buonaccorsi J, Lim J, Sato S, Rajala C, Averill J, Khalighinejad F, Ionete C, Jones SL, Kent JA, van Emmerik RE. [https://journals.sagepub.com/doi/full/10.1177/2055217320934835 Sensorimotor function in progressive multiple sclerosis.] Multiple Sclerosis Journal–Experimental, Translational and Clinical. 2020 Jul;6(3):2055217320934835.</ref> | ||
* Proprioception - contralateral joint matching task - reduced proprioception found in the ankle joint | * Proprioception - contralateral joint matching task - reduced proprioception found in the ankle joint<ref name=":5" /> | ||
<br /> '''''Gait''''' | <br /> '''''Gait''''' | ||
* Gait Deviations: | * Gait Deviations: | ||
** Foot drop during swing - right worse than left | ** Foot drop during swing - right worse than left<ref name=":0" /> | ||
** Poor heel strike during initial contact | ** Poor heel strike during initial contact<ref name=":0" /> | ||
** Shortened step length | ** Shortened step length<ref name=":0" /> | ||
** Knee buckling and hyperextension in mid-stance - right more than left<ref name=":0">[https://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical_Bulletin_Physical-Therapy-in-MS-Rehabilitation.pdf A RESOURCE FOR HEALTHCARE PROFESSIONALS: Physical Therapy in Multiple Sclerosis] [Internet]. National Multiple Sclerosis Society. 2018 [cited 2022May 2]. Available from: <nowiki>https://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical_Bulletin_Physical-Therapy-in-MS-Rehabilitation.pdf</nowiki></ref> | ** Knee buckling and hyperextension in mid-stance - right more than left<ref name=":0">[https://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical_Bulletin_Physical-Therapy-in-MS-Rehabilitation.pdf A RESOURCE FOR HEALTHCARE PROFESSIONALS: Physical Therapy in Multiple Sclerosis] [Internet]. National Multiple Sclerosis Society. 2018 [cited 2022May 2]. Available from: <nowiki>https://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical_Bulletin_Physical-Therapy-in-MS-Rehabilitation.pdf</nowiki></ref> | ||
* Assessment Measures | * Assessment Measures | ||
** [https://www.physio-pedia.com/index.php?title=Six_Minute_Walk_Test_/_6_Minute_Walk_Test&redirect=no%3Futm_source%3Dphysiopedia&utm_medium=search&utm_campaign=ongoing_internal 6 Minute Walk Test:] 348m | **[https://www.physio-pedia.com/index.php?title=Six_Minute_Walk_Test_/_6_Minute_Walk_Test&redirect=no%3Futm_source%3Dphysiopedia&utm_medium=search&utm_campaign=ongoing_internal 6 Minute Walk Test:] 348m<ref>Wetzel JL, Fry DK, Pfalzer LA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3076913/ Six-minute walk test for persons with mild or moderate disability from multiple sclerosis: performance and explanatory factors.] Physiotherapy Canada. 2011 Apr;63(2):166-80.</ref> | ||
** Multiple Sclerosis Walking Scale – 12 (MSWS-12): 36/60 (60%) | ** Multiple Sclerosis Walking Scale – 12 (MSWS-12): 36/60 (60%)<ref>[https://www.sralab.org/sites/default/files/2017-07/msws-eng.pdf Twelve item ms walking scale (MSWS-12)] [Internet]. Shirley Ryan AbilityLab. (n.d.). [cited 2022May 5]. Available from: <nowiki>https://www.sralab.org/sites/default/files/2017-07/msws-eng.pdf</nowiki></ref> | ||
** See Figure 1 | ** See Figure 1 | ||
[[File:Screen Shot 2022-05-03 at 9.25.47 PM.png|none|thumb|Figure 1: Multiple Sclerosis Walking Scale 12 ]] | [[File:Screen Shot 2022-05-03 at 9.25.47 PM.png|none|thumb|Figure 1: Multiple Sclerosis Walking Scale 12 ]] | ||
| Line 302: | Line 307: | ||
Assessments: | Assessments: | ||
* [https://www.physio-pedia.com/Balance_Evaluation_Systems_Test_(BESTest)?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Mini BESTest]: 11/28 | * [https://www.physio-pedia.com/Balance_Evaluation_Systems_Test_(BESTest)?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Mini BESTest]: 11/28<ref>[https://www.sralab.org/sites/default/files/2017-06/MiniBEST_revised_final_3_8_13.pdf Mini-bestest: Balance Evaluation Systems Test] [Internet]. Oregon health. (n.d.). [cited 2022May 9] Available from: <nowiki>https://www.sralab.org/sites/default/files/2017-06/MiniBEST_revised_final_3_8_13.pdf</nowiki></ref> | ||
** See Figure 2 | ** See Figure 2 | ||
[[File:Screen Shot 2022-05-06 at 9.58.02 AM.png|none|thumb|Figure 2: Mini BESTest]] | [[File:Screen Shot 2022-05-06 at 9.58.02 AM.png|none|thumb|Figure 2: Mini BESTest]] | ||
* [https://www.physio-pedia.com/Activities-Specific_Balance_Confidence_Scale?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Activities Balance Confidence Scale] (ABC): 69% | * [https://www.physio-pedia.com/Activities-Specific_Balance_Confidence_Scale?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Activities Balance Confidence Scale] (ABC): 69%<ref>Nilsagård Y, Carling A, Forsberg A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3420074/ Activities-specific balance confidence in people with multiple sclerosis.] Multiple sclerosis international. 2012 Aug 7;2012.</ref> | ||
** See Figure 3 | ** See Figure 3 | ||
| Line 313: | Line 318: | ||
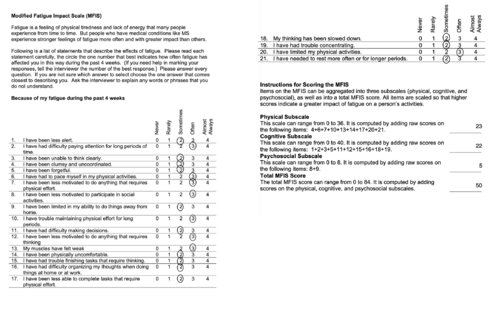
'''''Fatigue''''' | '''''Fatigue''''' | ||
* Modified Fatigue Impact Scale (MFIS): 50/84 | * Modified Fatigue Impact Scale (MFIS): 50/84<ref>[https://www.sralab.org/sites/default/files/2017-06/mfis.pdf Modified fatigue impact scale (MFIS)] [Internet]. Shirley Ryan Abilitylab. (n.d.). [cited 2022May 9]. Available from: <nowiki>https://www.sralab.org/sites/default/files/2017-06/mfis.pdf</nowiki></ref> | ||
** See Figure 4 | ** See Figure 4 | ||
[[File:Screen_Shot_2022-05-06_at_9.52.01_AM.png|alt=|none|thumb|500x500px|Figure 4: Modified fatigue impact scale]] | |||
[[File: | |||
== Clinical Impression == | == Clinical Impression == | ||
Revision as of 02:55, 10 May 2022
Abstract[edit | edit source]
Purpose: The case study was designed for Queen’s University PT858 Neurorehabilitation II course. The purpose of this fictional case study is to understand and explore an individual diagnosed with Primary Progressive Multiple Sclerosis (PPMS). Additionally, we investigated and applied a research-based treatment approach while integrating the role of technology in rehabilitation.
Case Presentation: This fictional case study focuses on Michelle White a female 47 year old work from home accountant who recently progressed from active primary progressive multiple sclerosis (PPMS) without progression to active PPMS with progression. Her primary complaints were fatigue, difficulty with normal gait, impaired balance, weakness and decreased attention and memory.
Intervention: Patient was prescribed activities and exercises that will maintain and improve her function as her MS continues to progress. These interventions are designed to target the short and long term goals of the patient to allow her to regain and maintain function that is meaningful to the patient. Prescribed exercises include aerobic exercise, resistance training, balance training, fatigue management, education as well as referrals to target problems that are outside the scope of physiotherapy. The use of technology in rehabilitation is used throughout the different aspects of intervention.
Outcomes: At the 4 month reassessment, Michelle White was reassessed in the following tests; Multiple Sclerosis Walking Scale, 6 Minute Walk, mini BESTest, Activities Balance Confidence Scale, 5 times sit to stand test and the Modified Fatigue Impact Scale. After completing her physiotherapy sessions, her home exercise routine and additional appointments with members of her inter-professional team, Michelle was able to improve her ability and confidence with ambulation, balance and activities of daily living.
Introduction[edit | edit source]
Multiple sclerosis (MS) is a neurological, autoimmune disease that affects the central nervous system (HOPKINS). Though the exact etiology of MS is unknown, it occurs when the immune system attacks nerve fibers and the myelin sheath of neuronal axons, leading to inflammation and demyelination of the central nervous system (TAFTI ET AL., 2022). As a result, it alters electrical signaling in the brain and leads to a variety of symptoms, such as difficulty with walking, blindness, paralysis, etc. In Canada, over 90,000 people are living with MS, which equates to 1 in every 400 people (MS SOCIETY). Annually, 4,377 Canadians are diagnosed with MS, which equates to almost 12 people per day (MS SOCIETY).
A thorough medical history in conjunction with a neurological examination and imaging are used to diagnose MS, and MS is diagnosed once other potential reasons for symptoms are ruled out (MS SOCIETY). MS can be classified into four types of diagnoses: clinically isolated syndrome, relapsing remitting, secondary progressive and primary progressive (NATIONAL MS SOCIETY).
Primary progressive multiple sclerosis (PPMS) is characterized by a gradual deterioration in functional capacity due to neurological deficits, without the occurrence of early relapses (exacerbation or flare-ups). Furthermore, this type of MS can be categorized as active (confirmed via an occasional relapse and/or imaging) or inactive, as well as progressive (evident decrease in functional capacity) or non-progressive (NATIONAL MS SOCIETY). Globally, 10-15% of individuals diagnosed with MS present with PPMS (TAFTI).
The fictional case study will highlight the experience of Michelle White, a 47-year-old female who was diagnosed with PPMS. Michelle was referred to physiotherapy due to an acute exacerbation of PPMS, and her primary goals with rehabilitation are to improve her walking capacity and ability to perform activities of daily living. The purpose of this case study is to provide evidence-based information from the literature regarding symptoms, objective findings, and interventions for PPMS.
Client Characteristics [edit | edit source]
Michelle White is a 47-year-old female (DOB March 14th, 1970) who was diagnosed with primary progressive MS 2 years ago. Since the onset of her symptoms, Michelle’s status has changed from being in the active without progression PPMS stage (increasing accumulation of disability), to active (new MRI changes) with progression (increasing accumulation of disability). Michelle was diagnosed with clinical depression 1 year ago and has been managing hypertension for the last 5 years. Michelle is a work-from-home accountant, and currently resides in a detached home in Mississauga, Ontario with her husband, 2 children, and family dog. Michelle was referred to rehabilitation by her neurologist to reduce the risk of a relapse, as well as to help improve her mobility (walking with the use of a mobility aid and balance training) and function (activities of daily living).
Examination Findings[edit | edit source]
Subjective Assessment[edit | edit source]
Chief Complaint: Michelle has concerns about taking her dog for daily walks in the summer. She is afraid of losing her balance and worried she won’t have enough energy to complete the walks. Michelle is also having trouble with the stairs in her house. She finds her legs weak and she is tired by the time she reaches the top of the stairs.
History of Present Illness:
- Medical diagnosis: PPMS active with progression
- Treatment to Date: No previous history of physiotherapy treatment.
- Current Symptoms:
Past Medical History:
- Diagnosed with active PPMS without progression 2 years ago
- Diagnosed with active PPMS with progression 2 weeks ago
- Comorbidities:
- Depression - diagnosed 1 year ago
- Prescribed medications
- Weekly visits to psychiatrist to help with depressive symptoms
- Hypertension - diagnosed 5 years ago
- Depression - diagnosed 1 year ago
Medications:
- Oral Paroxetine - 20mg, once a day for depressive symptoms[1][3]
- Norvasc (Amlodipine) - 5mg, once per day for hypertension[3]
- Ocrevus - 600 mg intravenous infusion every six months[3]
Social History: Michelle lives in Mississauga in a house with 2 steps to get into the house as well as 12 steps to get to the second floor. She lives there with her husband, 2 children and family dog. She has been a work-from-home accountant for the last 15 years. Michelle enjoys working from home but has noticed in the last few months that she has trouble concentrating on her work and thinks her memory has gotten worse. Her family recently moved to Mississauga from Ottawa in the last year, and friends and distant family are still located in Ottawa. Michelle enjoys walking her dog daily, reading and watching movies. However, she finds when she sits in the same position for a long period her pain and discomfort increases.
Family History: History of hypertension on maternal side
Functional History: Michelle was previously able to ambulate 45 minutes with dog without use of gait aid. She was also less fearful of community ambulation. Michelle also previously enjoyed gentle weight-bearing resistance training at her local gym, she would often go twice a week for about 30-45 minutes. Michelle was also able to walk up a flight of stairs without fatigue. She had no problems with her daily activities such as grooming, cleaning and cooking. However, she found carrying laundry up the stairs quite difficult but often received help from her husband or kids.
Current Functional Status: Michelle has been cutting back on the length of her workouts at the gym as she now finds resistance training more painful and difficult due to balance impairments. Michelle has also become more fearful of community ambulation due to fear of falling, and currently walks around the block. She only walks the dog twice a week due to her balance and stability deficits and will only go if her husband or one of her children accompanies her. Michelle is often fatigued and feels weak after walking up a flight of stairs and is unable to carry her laundry up the stairs anymore. She still manages her daily activities well, but finds herself tired if she does a large clean of the house.
Patient Goals:
- Michelle would like to get back to walking her dog daily, independently.
- Michelle would also like to limit the progression of her symptoms.
- Michelle would like to improve her strength to be able to walk up stairs better.
Objective Assessment[edit | edit source]
Range of Motion
- UE - WNL
- LE - Table #1
| Joint | Movement | Active ROM - LEFT | Passive ROM - LEFT | Active ROM - RIGHT | Passive ROM -RIGHT |
| Hip | Flexion | 100 | 105 | 90 | 100 |
| Hip | Extension | 10 | 15 | 10 | 15 |
| Hip | Adduction | 20 | 30 | 20 | 30 |
| Hip | Abduction | 40 | 45 | 40 | 45 |
| Hip | External Rotation | 30 | 40 | 30 | 40 |
| Hip | Internal Rotation | 30 | 40 | 30 | 40 |
| Knee | Flexion | 125 | 130 | 115 | 125 |
| Knee | Extension | 0 | -5 | -5 | -5 |
| Ankle | Plantar flexion | 40 | 45 | 35 | 45 |
| Ankle | Dorsiflexion | 10 | 15 | 5 | 10 |
| Ankle | Inversion | 15 | 20 | 10 | 15 |
| Ankle | Eversion | 5 | 10 | 5 | 10 |
Spasticity
- UE - WNL
- LE - Table #2
| Muscle Group | Left Limb | Right Limb |
| Hip Flexors | 0 | 0 |
| Hip Extensors | 0 | 0 |
| Hip Adductors | 0 | 0 |
| Hip Abductors | 0 | 0 |
| Knee Flexors | 1 | 1 |
| Knee Extensors | 1 | 1 |
| Ankle Plantar Flexors | 1+ | 2 |
| Ankle Dorsiflexors | 1 | 1+ |
Strength
5 Times Sit to Stand Test: 7.3 seconds[5]
Manual Muscle Testing (MMT)
- UE - WNL
- LE - Table #3
| Muscle Group | Score Left Limb | Score Right Limb |
| Hip Flexors | 4+ | 4+ |
| Hip Extensors | 4 | 4 |
| Hip Adductors | 4 | 4 |
| Hip Abductors | 4 | 3+ |
| Hip External Rotators | 4 | 3+ |
| Hip Internal Rotators | 4 | 3+ |
| Knee Flexors | 4 | 4- |
| Knee Extensors | 4 | 4- |
| Ankle Plantar Flexors | 4 | 4 |
| Ankle Dorsiflexors | 4- | 3+ |
| Ankle Inverters | 4- | 4- |
Neurological
- Dermatomes - WNL
- Myotomes - WNL
- Reflexes
- Sensation testing - decreased pinprick sensation to dorsal feet bilaterally[6]
- Proprioception - contralateral joint matching task - reduced proprioception found in the ankle joint[6]
Gait
- Gait Deviations:
- Assessment Measures
- 6 Minute Walk Test: 348m[8]
- Multiple Sclerosis Walking Scale – 12 (MSWS-12): 36/60 (60%)[9]
- See Figure 1
Balance
Assessments:
- Mini BESTest: 11/28[10]
- See Figure 2
- Activities Balance Confidence Scale (ABC): 69%[11]
- See Figure 3
Fatigue
- Modified Fatigue Impact Scale (MFIS): 50/84[12]
- See Figure 4
Clinical Impression[edit | edit source]
Patient Profile
Mrs. White is a 47-year-old female with PPMS that has been experiencing declining function since her disease progressed to active with progression. Currently, Mrs. White is presenting to outpatient rehabilitation with significantly impaired mobility and balance as a result of lower extremity weakness and spasticity, reduced sensation of the feet, gait deviations and fatigue. Additionally, Mrs. White is also experiencing urgency incontinence and cognitive deficits that are also impacting her quality of life.
Problems list
- Body structure function
- Reduced balance due to decreased proprioception and weakness in lower extremities.
- Impaired memory due to disease progression.
- Impaired sensation due to irreversible destruction of the myelin sheath and axons of nerves.[13]
- Mild drop foot gait with poor heel strike due to weak dorsiflexors.
- Increased muscle tone/spasticity around ankle and knee joint due to demyelinated nerves in brain and spinal cord.[14]
- Weak hip abductors, hip external and internal rotators, knee extensors and flexors and ankle dorsiflexors due to demyelinated peripheral nerves.
- Activity
- Difficulty climbing stairs due to fatigue and SOB.
- Urgency incontinence due to weakened sphincter muscles.
- Reduced attention span due to fatigue and cognitive deficits.
- Reduced walking endurance due to gait deviations and fatigue.
- Participation
- Unable to walk her dog due to impaired mobility and fatigue.
- Avoids resistance training due to pain and lack of stability.
- Difficulty concentrating at work due to impaired memory and attention deficits.
- Personal factors
- Patient is fearful of falling.
- Reduced productivity at work due to pain during prolonged positioning.
- Easily fatigued.
- Diagnosed with depression 1 year ago.
- Environmental
- The patient's home has 2 steps to enter, and 12 steps to reach the second floor.
Interventions[edit | edit source]
Patient Centered Treatment Goals
Short Term Goals:
- Patient will achieve a minimum of a 4/5 MMT score for all lower extremity muscle group
- Improvement in Activities Balance Confidence Scale score from 69% to 86% within 2 weeks. [15]
- Be able to ambulate up and down 12 stairs with a single-point cane independently within 2 weeks.
Long Term Goals:
- Patient will be able to lower her score on the MFIS by 10-20 points within 6 weeks .
- Patient will be able to maintain or improve her lower extremity MMT scores at current baseline within 6 months.
- Patient will be able to continue use of single-point cane without requiring a more stable gait aid over the next 4 months.
Strength Training:
- Functional exercises are prioritized, mainly targeting large muscle groups.
- Examples of functional exercises:
- Farmers Carry
- Sit to Stand
- 1/2 Squat
- Step ups and Step downs
- Heel walking & Toe walking
- Strengthening muscles of the lower extremity will help with improving gait as well as counteract spasticity present in ankles and knees.
- Muscle groups and examples:
- Dorsiflexors: Toe raises, resisted dorsiflexion
- Plantarflexors: Seated heel raises, standing heel raises
- Knee Flexors: Hamstring curls, RDLs
- Knee Extensors: resisted knee extension, mini squat
- Hip Abductors: side-lying hip abduction
- General parameters for strength training, used for all exercises listed above: [7]
- 8-12 reps at 60-80% of the patients one repetition max performing 2-3 sets, 2-3 times per week. Rest for 2-3 minutes between sets is recommended. [7]
- Patient should be reaching fatigue within the outlined rep range. If the patient is able to reach 12 reps with minimal to mild fatigue, resistance should be added or increased.
Gait Training:
- Prescribe and fit patient to a single-point cane to improve stability while maintaining as much mobility as possible.
- FES can be incorporated to help improve gait pattern in the early stages by facilitating dorsiflexion through activation of the tibialis anterior to improve drop foot gait. [17]
- Ideally continue with gait training until single-point cane is no longer required for stable ambulation. This is dependant solely on the changes that are seen within the patients condition; both improvements in function as well as progressions of PPMS decreasing function.
Aerobic Training:
- Aerobic exercise will improve the patients aerobic capacity and improve her ability to walk for longer periods of time without fatigue. [18]
- Should be performed 3-4 times per week working up to around 20-30 minutes. [7]
- Methods of aerobic training include:
- Treadmill training, swimming, walking, arm bike
- From all options listed above, patients goals align most with walking therefore walking will be prioritized.
- Treadmill training, swimming, walking, arm bike
- Be mindful of the patients level of fatigue throughout training.
Balance Training:
- In clinic exercises, performed with supervision and guarding, roughly 2 minutes of each activity. As the patient gets more comfortable, balance exercises can be performed outside of the clinical setting. Examples include: [19]
- Standing eyes open, progressing to eyes closed and widening base of support as needed
- Ankle sways
- Marching in place
- Reaching, nudging and leaning in seated progressing to standing as well as to eyes closed as tolerated
- Adding cognitive task to any or all of the above to increase intensity and difficulty for the patient
- Other alternatives to balance exercises include: Tai Chi, Yoga, Pilates [7]
- Patient is encouraged to find a program or class in one of the categories listed above that is of most interest to her in order to train balance in a different environment. [7]
Education:
- Reducing fatigue can be addressed with the 4P's: Pacing, Planning, Prioritizing, and Positioning.[7]
- Any exercise can be broken up throughout the day to further manage fatigue.
- Educate the patient to take breaks as required.
- Patient is educated on the use of a single-point cane with a 2 point step-to gait pattern, progressing to a step-through pattern as the patient gets comfortable and her balance and stability improves.
- Patient is informed that exercise is important and movement is always encouraged [7]
- As the disease may progress, exercise is modified to ensure that the patient is doing as much as they can based on their new functional status
- Patient should seek Physiotherapy even when her symptoms are stable to follow up with functional status and make any changes to treatment plan as necessary.
Referrals:
- Patient will be referred to a Pelvic Floor Physiotherapist to help treat her urgency incontinence.
- Patient will be referred to an Occupational Therapist to work on improving memory and attention.
- Patient will be referred to a Psychologist to control her depression if she is not currently seeing one.
Outcome[edit | edit source]
After Michelle’s initial assessment on May 3, 2022 she was reassessed on September 4th, 2022, about 4 months later. She was reassessed using the Multiple Sclerosis Walking Scale, 6 Minute Walk, mini BESTest, Activities Balance Confidence Scale, Modified Fatigue Impact Scale and 5 times sit to stand. The table #3 below shows the change in each test. Michelle’s improvement in the Multiple Sclerosis Walking and her 6 minute walk test demonstrates her improvement in her ability to walk, including improving her pace, distance and effort needed to walk. Michelle's improved mini BESTest, Activities Balance Confidence scale and 5 minutes sit to stand demonstrates the positive impact of the interventions on her dynamic balance, functional mobility and confidence in balance. While completing these tests, Michelle experienced less overall fatigue.
| Outcome Measure | Initial Assessment: May 3rd, 2022 | Reassessment: September 4th, 2022 |
| Multiple Sclerosis Walking Scale | 36/60 or 60% | 28/60 or 47% |
| 6 Minute Walk | 348m | 387m |
| Mini BESTest | 11/28 | 16/28 |
| Activities Balance Confidence Scale | 69% | 76% |
| 5 times sit to stand test | 7.3 seconds | 6.9 seconds |
| Modified Fatigue Impact Scale | 50/84 | 39/84 |
After the 16-week intervention, we are pleased with the progress Michelle has made and believe she is ready for discharge from physiotherapy. Michelle will continue with her home exercise program and understands she is able to contact the clinic if she has any questions or concerns. No further referrals are needed at this time.
Michelle responded positively to the assessment with a pelvic floor physiotherapist to provide support for her urinary incontinence. She will continue to see the pelvic floor physiotherapist. She will continue to have follow-up appointments with other members of her inter-professional team including her neurologist and general practitioner to follow the progression of her PPMS as well as her psychiatrist to help support her depression.
Discussion[edit | edit source]
Self-Study Questions[edit | edit source]
1.Which of the following is not true related to the Mini-BESTest?
a) It assesses the patient’s compensatory stepping ability
b) It assesses postural control
c) It does not include dynamic gait tests
d) It is frequently used on patients with Multiple Sclerosis
2.Which is true about Multiple sclerosis?
a) MS is more prevalent in males than females
b) Fatigue is not a common symptom of MS
c) MS is more common in Europe
d) Symptoms progress faster in males than females
3.What is the best intervention approach for a physiotherapy session for someone with Multiple sclerosis?
a) High intensity and high repetition during physiotherapy sessions
b) Functional activities that focus on balance and gait
c) Having the physiotherapy session focus only on upper extremities
d) All of the above would be helpful in improving MS symptoms
Answers: (1) C (2) D (3) B
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Tsang BK, Macdonell R. Multiple sclerosis: diagnosis, management and prognosis. Australian family physician. 2011 Dec;40(12):948-55.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Miller DH, Leary SM. Primary-progressive multiple sclerosis. The Lancet Neurology. 2007 Oct 1;6(10):903-12.
- ↑ 3.0 3.1 3.2 Medications [Internet]. MS Society of Canada. (n.d.). [cited 2022May2]. Available from https://mssociety.ca/managing-ms/treatments/medications
- ↑ Harb A, Kishner S. Modified ashworth scale. InStatPearls [Internet] 2021 May 9. StatPearls Publishing.
- ↑ Five times SIT to stand test [Internet]. Shirley Ryan AbilityLab. (2013). [cited 2022May 5]. Available from: https://www.sralab.org/rehabilitation-measures/five-times-sit-stand-test#non-specific-patient-population
- ↑ 6.0 6.1 Miehm JD, Buonaccorsi J, Lim J, Sato S, Rajala C, Averill J, Khalighinejad F, Ionete C, Jones SL, Kent JA, van Emmerik RE. Sensorimotor function in progressive multiple sclerosis. Multiple Sclerosis Journal–Experimental, Translational and Clinical. 2020 Jul;6(3):2055217320934835.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 A RESOURCE FOR HEALTHCARE PROFESSIONALS: Physical Therapy in Multiple Sclerosis [Internet]. National Multiple Sclerosis Society. 2018 [cited 2022May 2]. Available from: https://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical_Bulletin_Physical-Therapy-in-MS-Rehabilitation.pdf
- ↑ Wetzel JL, Fry DK, Pfalzer LA. Six-minute walk test for persons with mild or moderate disability from multiple sclerosis: performance and explanatory factors. Physiotherapy Canada. 2011 Apr;63(2):166-80.
- ↑ Twelve item ms walking scale (MSWS-12) [Internet]. Shirley Ryan AbilityLab. (n.d.). [cited 2022May 5]. Available from: https://www.sralab.org/sites/default/files/2017-07/msws-eng.pdf
- ↑ Mini-bestest: Balance Evaluation Systems Test [Internet]. Oregon health. (n.d.). [cited 2022May 9] Available from: https://www.sralab.org/sites/default/files/2017-06/MiniBEST_revised_final_3_8_13.pdf
- ↑ Nilsagård Y, Carling A, Forsberg A. Activities-specific balance confidence in people with multiple sclerosis. Multiple sclerosis international. 2012 Aug 7;2012.
- ↑ Modified fatigue impact scale (MFIS) [Internet]. Shirley Ryan Abilitylab. (n.d.). [cited 2022May 9]. Available from: https://www.sralab.org/sites/default/files/2017-06/mfis.pdf
- ↑ Multiple sclerosis [Internet]. NORD (National Organization for Rare Disorders). 2020 [cited 2022May9]. Available from: https://rarediseases.org/rare-diseases/multiple-sclerosis/
- ↑ Spasticity (stiffness) [Internet]. MSAA. 2022 [cited 2022May9]. Available from: https://mymsaa.org/ms-information/symptoms/spasticity/
- ↑ Raad J, Moore J, Hamby J, Rivadelo RL, Straube D. A brief review of the Activities-Specific Balance Confidence Scale in older adults. Archives of Physical Medicine and Rehabilitation. 2013 Jul 1;94(7):1426-7.
- ↑ 16.0 16.1 Lo AC, Triche EW. Improving gait in multiple sclerosis using robot-assisted, body weight supported treadmill training. Neurorehabilitation and neural repair. 2008 Nov;22(6):661-71.
- ↑ Campbell E, Coulter EH, Mattison PG, Miller L, McFadyen A, Paul L. Physiotherapy rehabilitation for people with progressive multiple sclerosis: a systematic review. Archives of physical medicine and rehabilitation. 2016 Jan 1;97(1):141-51.
- ↑ Beer S, Khan F, Kesselring J. Rehabilitation interventions in multiple sclerosis: an overview. Journal of neurology. 2012 Sep;259(9):1994-2008.
- ↑ Jackson K, Mulcare JA, Donahoe-Fillmore B, Fritz HI, Rodgers MM. Home balance training intervention for people with multiple sclerosis. International Journal of MS Care. 2007;9(3):111-7.