Primary-Progressive Multiple Sclerosis (PPMS) - A Case Study: Difference between revisions
No edit summary |
No edit summary |
||
| Line 390: | Line 390: | ||
* | * | ||
* FES can be incorporated to help improve gait pattern in the early stages by facilitating dorsiflexion through activation of the tibialis anterior to improve | * FES can be incorporated to help improve gait pattern in the early stages by facilitating dorsiflexion through activation of the tibialis anterior to improve drop foot gait. | ||
** | ** | ||
* Ideally continue with gait training until single-point cane is no longer required for stable ambulation. This is dependant solely on the changes that are seen within the patients condition; both improvements in function as well as progressions of PPMS decreasing function. | * Ideally continue with gait training until single-point cane is no longer required for stable ambulation. This is dependant solely on the changes that are seen within the patients condition; both improvements in function as well as progressions of PPMS decreasing function. | ||
Revision as of 15:53, 7 May 2022
Abstract[edit | edit source]
Purpose:
Case Presentation:
Intervention:
Outcomes:
Introduction[edit | edit source]
Add your content to this page here!
Client Characteristics [edit | edit source]
Add your content to this page here!
Examination Findings[edit | edit source]
Subjective Assessment[edit | edit source]
Chief Complaint: Michelle has concerns about taking her dog for daily walks in the summer. She is afraid of losing her balance and worried she won’t have enough energy to complete the walks. Michelle is also having trouble with the stairs in her house. She finds her legs weak and she is tired by the time she reaches the top of the stairs.
History of Present Illness:
- Medical diagnosis: PPMS active with progression
- MRI to confirm and identify areas of lesions in the brain
- Positive lumbar puncture test
- Positive evoked potentials test
- Treatment to Date: No previous history of physiotherapy treatment.
- Current Symptoms:
- Impaired mobility
- Weakness and stiffness in the legs, the right leg worse than the left.
- Decreased attention, and memory
- Pins and needles in the feet
- Urgency incontinence
- Fatigue
- Difficulty with normal gait
- Balance impairments
Past Medical History:
- Diagnosed with active PPMS without progression 2 years ago
- Diagnosed with active PPMS with progression 2 weeks ago
- Comorbidities:
- Depression - diagnosed 1 year ago
- Prescribed medications
- Weekly visits to psychiatrist to help with depressive symptoms
- Hypertension - diagnosed 5 years ago
- Depression - diagnosed 1 year ago
Medications:
- Oral Paroxetine - 20mg, once a day for depressive symptoms
- Norvasc (Amlodipine) - 5mg, once per day for hypertension
- Ocrevus - 600 mg intravenous infusion every six months
Social History: Michelle lives in Mississauga in a house with 2 steps to get into the house as well as 12 steps to get to the second floor. She lives there with her husband, 2 children and family dog. She has been a work-from-home accountant for the last 15 years. Michelle enjoys working from home but has noticed in the last few months that she has trouble concentrating on her work and thinks her memory has gotten worse. Her family recently moved to Mississauga from Ottawa in the last year, and friends and distant family are still located in Ottawa. Michelle enjoys walking her dog daily, reading and watching movies. However, she finds when she sits in the same position for a long period her pain and discomfort increases.
Family History: History of hypertension on maternal side
Functional History: Michelle was previously able to ambulate 45 minutes with dog without use of gait aid. She was also less fearful of community ambulation. Michelle also previously enjoyed gentle weight-bearing resistance training at her local gym, she would often go twice a week for about 30-45 minutes. Michelle was also able to walk up a flight of stairs without fatigue. She had no problems with her daily activities such as grooming, cleaning and cooking. However, she found carrying laundry up the stairs quite difficult but often received help from her husband or kids.
Current Functional Status: Michelle has been cutting back on the length of her workouts at the gym as she now finds resistance training more painful and difficult due to balance impairments. Michelle has also become more fearful of community ambulation due to fear of falling, and currently walks around the block. She only walks the dog twice a week due to her balance and stability deficits and will only go if her husband or one of her children accompanies her. Michelle is often fatigued and feels weak after walking up a flight of stairs and is unable to carry her laundry up the stairs anymore. She still manages her daily activities well, but finds herself tired if she does a large clean of the house.
Patient Goals:
- Michelle would like to get back to walking her dog daily, independently.
- Michelle would also like to limit the progression of her symptoms.
- Michelle would like to improve her strength to be able to walk up stairs better.
Objective Assessment[edit | edit source]
Range of Motion
- UE - WNL
- LE - Table #1
| Joint | Movement | Active ROM - LEFT | Passive ROM - LEFT | Active ROM - RIGHT | Passive ROM -RIGHT |
| Hip | Flexion | 100 | 105 | 90 | 100 |
| Hip | Extension | 10 | 15 | 10 | 15 |
| Hip | Adduction | 20 | 30 | 20 | 30 |
| Hip | Abduction | 40 | 45 | 40 | 45 |
| Hip | External Rotation | 30 | 40 | 30 | 40 |
| Hip | Internal Rotation | 30 | 40 | 30 | 40 |
| Knee | Flexion | 125 | 130 | 115 | 125 |
| Knee | Extension | 0 | -5 | -5 | -5 |
| Ankle | Plantar flexion | 40 | 45 | 35 | 45 |
| Ankle | Dorsiflexion | 10 | 15 | 5 | 10 |
| Ankle | Inversion | 15 | 20 | 10 | 15 |
| Ankle | Eversion | 5 | 10 | 5 | 10 |
Spasticity
Modified Ashworth Scale
- UE - WNL
- LE - Table #2
| Muscle Group | Left Limb | Right Limb |
| Hip Flexors | 0 | 0 |
| Hip Extensors | 0 | 0 |
| Hip Adductors | 0 | 0 |
| Hip Abductors | 0 | 0 |
| Knee Flexors | 1 | 1 |
| Knee Extensors | 1 | 1 |
| Ankle Plantar Flexors | 1+ | 2 |
| Ankle Dorsiflexors | 1 | 1+ |
Strength
Manual Muscle Testing (MMT)
- UE - WNL
- LE - Table #3
| Muscle Group | Score Left Limb | Score Right Limb |
| Hip Flexors | 4+ | 4+ |
| Hip Extensors | 4 | 4 |
| Hip Adductors | 4 | 4 |
| Hip Abductors | 4 | 3+ |
| Hip External Rotators | 4 | 3+ |
| Hip Internal Rotators | 4 | 3+ |
| Knee Flexors | 4 | 4- |
| Knee Extensors | 4 | 4- |
| Ankle Plantar Flexors | 4 | 4 |
| Ankle Dorsiflexors | 4- | 3+ |
| Ankle Inverters | 4- | 4- |
Neurological
- Dermatomes - WNL
- Myotomes - WNL
- Reflexes
- UMN
- Clonus - postitive
- Babinski - positive
- LMN
- Patellar - 3/4
- Achilles - 3/4
- UMN
- Sensation testing - decreased pinprick sensation to dorsal feet bilaterally
- Proprioception - contralateral joint matching task - reduced proprioception found in the ankle joint
Gait
- Gait Deviations:
- Foot drop during swing - right worse than left
- Poor heel strike during initial contact
- Shortened step length
- Knee buckling and hyperextension in mid-stance - right more than left
- Assessment Measures
- 6 Minute Walk Test: 348m
- Multiple Sclerosis Walking Scale – 12 (MSWS-12): 36/60 (60%)
- See Figure 1
Balance
Assessments:
- Mini BESTest: 11/28
- See Figure 2
- Activities Balance Confidence Scale (ABC): 69%
- See Figure 3
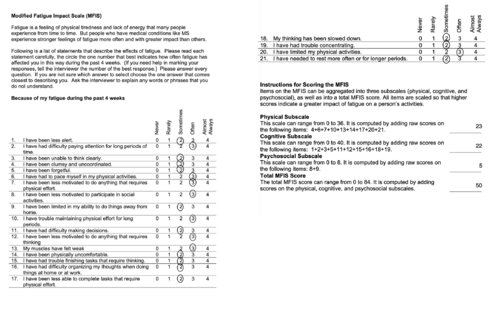
Fatigue
- Modified Fatigue Impact Scale (MFIS): 50/84
- See Figure 4
Clinical Impression[edit | edit source]
Patient Profile
Mrs. White is a 47-year-old female with PPMS that has been experiencing declining function since her disease progressed to active with progression. Currently, Mrs. White is presenting to outpatient rehabilitation with significantly impaired mobility and balance as a result of lower extremity weakness and spasticity, reduced sensation of the feet, gait deviations and fatigue. Additionally, Mrs. White is also experiencing urgency incontinence and cognitive deficits that are also impacting her quality of life.
Problems list
- Body structure function
- Reduced balance due to decreased proprioception and weakness in lower extremities.
- Impaired memory due to disease progression.
- Impaired sensation due to irreversible destruction of the myelin sheath and axons of nerves.1
- Mild drop foot gait with poor heel strike due to weak dorsiflexors.
- Increased muscle tone/spasticity around ankle and knee joint due to demyelinated nerves in brain and spinal cord.2
- Weak hip abductors, hip external and internal rotators, knee extensors and flexors and ankle dorsiflexors due to demyelinated peripheral nerves.
- Activity
- Difficulty climbing stairs due to fatigue and SOB.
- Urgency incontinence due to weakened sphincter muscles.
- Reduced attention span due to fatigue and cognitive deficits.
- Reduced walking endurance due to gait deviations and fatigue.
- Participation
- Unable to walk her dog due to impaired mobility and fatigue.
- Avoids resistance training due to pain and lack of stability.
- Difficulty concentrating at work due to impaired memory and attention deficits.
- Personal factors
- Patient is fearful of falling.
- Reduced productivity at work due to pain during prolonged positioning.
- Easily fatigued.
- Diagnosed with depression 1 year ago.
- Environmental
- The patient's home has 2 steps to enter, and 12 steps to reach the second floor.
Interventions[edit | edit source]
Patient Centered Treatment Goals
Short Term Goals:
- Patient will achieve a minimum of a 4/5 MMT score for all lower extremity muscle group
- Improvement in Activities Balance Confidence Scale score from 69% to 86% within 2 weeks.
- Be able to ambulate up and down 12 stairs with a single-point cane independently within 2 weeks.
Long Term Goals:
- Patient will be able to take dog for a 20 minute walk 3 times a week with single-point cane and little to no fatigue within 6 weeks.
- Patient will be able to maintain or improve her lower extremity MMT scores at current baseline within 6 months.
Strength Training:
- Functional exercises are prioritized, mainly targeting large muscle groups.
- Examples of functional exercises:
- Farmers Carry
- Sit to Stand
- Mini Squat
- Step ups and Step downs
- Heel walking & Toe walking
- Strengthening muscles of the lower extremity with help with improving gait as well as counteract spasticity present in ankles and knees.
- Muscle groups and examples:
- Dorsiflexors: Toe raises, resisted dorsiflexion
- Plantarflexors: Seated heel raises, standing heel raises
- Knee Flexors: Hamstring curls, RDLs
- Knee Extensors: resisted knee extension, mini squat
- General parameters for strength training:
- 8-12 reps at 60-80% of the patients one repetition max performing 2-3 sets, 2-3 times per week
- Patient should be reaching fatigue within the outlines rep range. If the patient is able to reach 12 reps with mild fatigue, resistance should be added or increased.
Gait Training:
- Prescribe and fit patient to a single-point cane to improve stability while maintaining as much mobility as possible.
- Gait training may include:
- Body weight treadmill training
- Robot-assisted training
- FES can be incorporated to help improve gait pattern in the early stages by facilitating dorsiflexion through activation of the tibialis anterior to improve drop foot gait.
- Ideally continue with gait training until single-point cane is no longer required for stable ambulation. This is dependant solely on the changes that are seen within the patients condition; both improvements in function as well as progressions of PPMS decreasing function.
Aerobic Training:
- Aerobic exercise will improve the patients aerobic capacity and improve her ability to walk for longer periods of time without fatigue
- Methods of aerobic training include:
- Treadmill training, swimming, walking, arm bike
- Be mindful of the patients level of fatigue throughout training.
Balance Training:
Stretching:
Education:
- Reducing fatigue can be addressed with the 4P's: Pacing, Planning, Prioritizing, and Positioning.
- Conserving energy by managing the characteristics listed above can reduce the amount of fatigue that the patient experiences.
- Educate the patient to take breaks as required.
Referrals:
- Patient will be referred to a Pelvic Floor Physiotherapist to help treat her urgency incontinence.
- Patient will also be referred to an Occupational Therapist to work on improving memory and attention.
Outcome[edit | edit source]
Discussion[edit | edit source]
Self-Study Questions[edit | edit source]
References[edit | edit source]
see adding references tutorial.