Post Concussion Syndrome Case Study: Following a Fall
Abstract[edit | edit source]
Introduction[edit | edit source]
Concussion is a mild brain injury that is commonly seen in events such as sports and motor vehicle accidents. After the initial injury, symptoms such as headache and dizziness tend to persist for weeks, months, or even years; this phenomenon is referred to as post-concussion syndrome (PCS).[1]
The consequences of concussion can include physical, cognitive and/or emotional abnormalities. The duration of concussion symptoms can range depending on the nature of the injury and the individual affected. Sport-related concussion symptoms typically resolve in 7-10 days in adults, and up to 3-4 weeks in children and adolescence. However, in some cases, these symptoms persist for a longer period of time, this is referred to as post-concussion syndrome.[2] Following a concussion, patients are typically advised to rest and avoid any strenuous physical or cognitive activity until the patient’s symptoms have resided. This has also been the traditional approach for post concussion syndrome combined with education, support/reassurance and antidepressants, and neuro-cognitive rehabilitation.[3] However, more recent research has recommended that there are several active therapies that may benefit recovery if intensity is kept below the symptom threshold.[2] Some of these more active approaches may include cognitive therapies, physical therapy, aerobic exercise, vestibular therapies and ocular therapies. Although rest may be important in the initial phases of recovery from concussion, there is evidence that low-level exercise and multimodal physical therapy is beneficial for patients who are recovering slowly following a sports related concussion.[4]
The purpose of this case study is to expose the readers on a typical patient with post-concussion syndrome, how it affects the patient’s life, and how it can be managed with physiotherapy, to subsequently improve the patient’s quality of life.
Client Characteristics[edit | edit source]
36-year-old female with post-concussion syndrome; seeking help from physiotherapy due to persistent symptoms (e.g., headache, dizziness) that are affecting the quality of her life. There are no other relevant comorbid conditions.
Examination Findings[edit | edit source]
Subjective
History of Present Illness - Initial injury occurred on January 2nd, 2020; patient fell and hit the back of her head while ice-skating and lost consciousness. She was sent to the hospital and diagnosed with a concussion. The patient was discharged from the hospital the following day and returned home. Patient returned to work on January 6th, four days post injury, but was unable to continue after a few hours due to the presence of severe headache. She then remained off work for a few weeks with persistent symptoms, at which point the she made an appointment with her family physician, and she was then referred to see a physiotherapist for rehabilitation and management.
Past Medical History - Healthy prior to injury; no previous trauma, surgeries, or other serious health conditions/comorbidities noted
Major Symptoms
Headache - constant, dull, diffuse headache 2/10 at rest
- Aggravating factors
- Physical activity: pain increases to 7 or 8/10 with ~20 min of moderate activity, particularly when the activity involves head movements, which then reaches 7 or 8/10 more quickly
- Cognitive activity: pain level increases to 4 or 5/10 with ~30 min of activities such as reading, planning, and learning.
- Exposure to light sources: pain reaches 7 or 8/10 in ~20 min when outside on a sunny day without sunglasses (able to tolerate over one hour with sunglasses); ~30 min of screen time can also raise the pain level to 7 or 8/10
- Easing factors:
- Rest: pain usually returns to baseline (2/10) with ~10 minutes of rest and removal of aggravating factors;
- The higher the pain level, the longer it usually takes to return to baseline
- The longer the exposure to aggravating factors, the longer it takes to return to baseline
- Rest: pain usually returns to baseline (2/10) with ~10 minutes of rest and removal of aggravating factors;
Medications - No medications; occasionally takes Tylenol 2-3 days per week if headaches become unbearable (i.e., 8/10 pain)
Health Habits - Non-smoker; consumption of wine (2-3 glasses/week) prior to the injury - has ceased drinking any alcohol post-injury
Social History - Registered Nurse (RN) for 11 years; practiced yoga for 10 years and has been teaching yoga for the past 5 years; currently living in a two-storey townhouse with fiancé.
Current Level of Function - Able to ambulate normally at home and perform simple chores independently, sleep quality has decreased markedly since the injury: has trouble falling asleep and wakes up 2-3 times on average at night; able to drive during day time, but has difficulty at night time due to light sensitivity (i.e., bright lights from car); decreased concentration and memory has been noted; more likely to become emotional over relatively trivial issues (i.e., spilling milk); tolerance for moderately challenging activities (such as work) has decreased drastically due to headaches, decreased cognitive capacity, moodiness, etc. Although the major complaint is of headache, the patient also reports slight dizziness when looking around frequently (i.e., such as looking for a product during grocery shopping).
Objective
Blood Pressure - 108 mmHg / 66 mmHg (within normal limits)
Heart Rate - 66 bpm (within normal limits)
General Observation - no significant postural abnormalities
Gait - normal
Speech - normal speech comprehension and fluency
Upper Limb Scan Exam - normal
Upper Limb Neurological Exam - normal dermatomes, myotomes & reflexes
Cranial Nerve Testing - normal
Cervical Active ROM - all ranges within normal limits
Superficial and Deep Neck Flexors - normal activation and strength
Palpation - increased tightness bilaterally in upper fibre trapezius and levator scapulae
- Remarks: neck muscles dysfunctions are often associated with people with PCS, and tightness in neck muscles may lead to increased headaches[5]
Outcome Measures
Modified Clinical Test for Sensory Interaction on Balance (CTSIB-M)
| Condition | Results (out of 30 sec) |
|---|---|
| Firm Surface, Eyes Open | Trial 1: 30sec |
| Firm Surface, Eyes Closed | Trial 1: 30sec |
| Foam Surface, Eyes Open | Trial 1: 30sec |
| Foam Surface, Eyes Closed | Trial 1: 18sec
Trial 2: 21sec Trial 3: 19sec |
Total Score: 111 sec/ 120 sec (sum of best results from each condition)
- Remarks: CTSIB-M is used to test the three sensory inputs (somatosensory, visual, and vestibular inputs) that are important for balance[6]
Static Balance
| Condition | Results (out of 30 sec) |
|---|---|
| Tandem stance (eyes open) | Left foot behind: 30 sec
Right foot behind: 30 sec |
| Tandem Stance (eyes closed) | Left foot behind:
Right foot behind:
|
| Single Leg Stance (eyes open) | Left foot: 30 sec
Right foot: 30 sec |
| Single Leg Stance (eyes closed) | Left foot:
Right foot:
|
- Remarks: these items were included since the patient reported having no difficulty staying in tandem stance or single leg stance, eyes closed, for at least 30 seconds prior to the injury. Research suggests that the mean for single leg stance, eyes closed for the patient’s demographic (18-39 y.o. female) is about 13 seconds,[7] whereas for tandem stance, eyes closed, it is about 26 seconds.[8] The 30 second mark is set both as a convenient value for assessment and as a (short-term) goal for the patient to return to prior-to-injury function.
Score: 29/30 - Mild difficulties for "Gait with Eyes Closed" condition (Score: 2/3)
- Remarks: the FGA is a 10-item assessment tool used to evaluate a patient's dynamic gait and vestibular impairments;[9] study suggests that the cut-off score for increased fall risk is 22/30.[10] Although the patient’s score is above the cut-off, it does give us some hints as to the exercises to prescribe (i.e., dynamic balance when eyes closed)
The Headache Impact Test
Score: 61 - Severe impact on quality of life
- Remarks: The Headache Impact Test is a 6-question questionnaire that assesses the severity of the impact a headache has on one’s life. The score ranges from 36 to 78: the impact is considered little to none for scores below 50, scores of 50-55 are interpreted as some impact is produced by the headache, 56-59 is substantial impact, and scores above 60 are severe impact.[11] Using this categorization, the patient’s headache is having a severe impact on her life, which is consistent with her primary complaint, and it is certainly a major focus of the treatment.
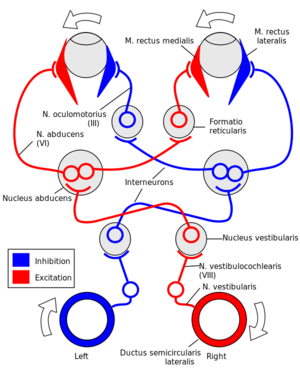
Vestibular-Oculomotor Screening (VOMS) Test
| Vestibular/Ocular Motor Test | Headaches
(0-10) |
Dizziness
(0-10) |
Nausea
(0-10) |
Fogginess
(0-10) |
Comments |
|---|---|---|---|---|---|
| Baseline Symptoms | 2 | 0 | 0 | 0 | Constant dull headache at rest |
| Smooth Pursuits | 2 | 0 | 0 | 0 | |
| Saccades - Horizontal | 4 | 1 | 0 | 0 | Symptoms returned to baseline in less than 30s |
| Saccades - Verticle | 3 | 0 | 0 | 0 | Symptoms returned to baseline in less than 30s |
| Convergence (Near Point) | 2 | 0 | 0 | 0 | Able to bring the tip of pen to nose, no double vision noted |
| VOR - Horizontal | 6 | 4 | 3 | 0 | Symptoms returned to baseline after ~1 min |
| VOR - Vertical | 5 | 2 | 2 | 0 | Symptoms returned to baseline after ~30s |
| Visual Motion Sensitivity Test | 5 | 4 | 2 | 0 | Symptoms returned to baseline after ~30s |
- Remarks: the VOMS is a tool used to test vestibular/oculomotor impairments and motion sensitivity for patients with PCS;[12] results from VOMS can guide our treatment exercises.[13]
Clinical Impression[edit | edit source]
Diagnosis
36 year-old female presenting with post concussion syndrome 4 weeks after diagnosis of concussion from fall while ice skating on Jan 2, 2020. Patient has impaired balance and vestibular system, and motion sensitivity. She has persistent headache, which is exacerbated by motion and cognitive tasks; the bilateral tightness in upper trapezius and levator scapulae might also contribute to her headache. These symptoms are interfering with return to work, driving at night, getting a restful sleep, grocery shopping, learning, etc. The patient is an excellent candidate for physiotherapy.
Problem List
- Disturbance in quality of sleep
- Inability to drive at night due to light sensitivity
- Persistent headache
- Decreased concentration and moodiness
- Motion sensitivity
- Impaired balance, particularly when vestibular system is challenged
Intervention[edit | edit source]
Patient-focused Goals
- Reduce headache severity at rest from a 2/10 to 0/10 by the end of the 3rd week of treatment
- Be able to maintain static single leg stance balance bilaterally with eyes closed for 30 seconds by the end of the 4th week of treatment
- Be able to turn head while walking without causing nausea or dizziness by the end of the 6th week of treatment
Education
- Provide the patient with reassurance about her condition
- Provide coping strategies
- Discuss expected recovery time[2]
- Educate the patient on appropriate performance, and structuring of return to activities and work[14]
Manual Therapy
Soft Tissue Release Technique
- Upper fibers trapezius (bilateral)
- Levator Scapulae (bilateral)
Parameters: Passive approach with gliding pressure along muscle fibres in multiple planes, 10 reps total each side
Progression: Can progress to performing active-assisted and then active STR
Trigger Point Release Technique
- Upper fibers Trapezius (bilateral)
- Levator Scapulae (bilateral)
Parameters: Apply pressure on trigger points for 30 seconds, 2 reps, each side
*****need to include research on why STR is good at relieving post-concussion headache symptoms, same with trigger point release******
Exercise
Balance
Stretching
Gaze Stability Exercise (VOR)
Outcome[edit | edit source]
Change in Status Post Intervention
After the patient completed physiotherapy treatment (duration: 8 weeks, 2 sessions per week), she noticed a marked change in the presence of her symptoms. The headaches completely disappeared from baseline, presenting as a constant dull and achey pain, to no pain at all. While completing her ADLs, ***
Outcome Measures
Modified Clinical Test for Sensory Interaction on Balance (CTSIB-M)
| Condition | Results (out of a possible 30sec) |
|---|---|
| Firm Surface, Eyes Open | Trial 1: 30sec |
| Firm Surface, Eyes Closed | Trial 1: 30sec |
| Foam Surface, Eyes Open | Trial 1: 30sec |
| Foam Surface, Eyes Closed | Trial 1: 30sec |
Total Score: 120sec/120sec
Static Balance
| Condition | Results (out of a possible 30 sec) |
|---|---|
| Tandem Stance (eyes open) | Left foot behind: 30sec
Right foot behind: 30 sec |
| Tandem Stance (eyes closed) | Left foot behind: 30sec
Right foot behind: 30sec |
| Single Leg Stance (eyes open) | Left foot: 30sec
Right foot: 30sec |
| Single Leg Stance (eyes closed) | Left foot: 30sec
Right foot: 30sec |
Functional Gait Assessment
The Headache Impact Test
Vestibular-Oculomotor Screening (VOMS) Test
| Vestibular/Ocular Motor Test | Headaches
(0-10) |
Dizziness
(0-10) |
Nausea
(0-10) |
Fogginess
(0-10) |
Comments |
|---|---|---|---|---|---|
| Baseline Symptoms | 0 | 0 | 0 | 0 | |
| Smooth Pursuits | 2 | 0 | 0 | 0 | |
| Saccades - Horizontal | 2 | 1 | 0 | 0 | Symptoms returned to baseline after ~10s |
| Saccades - Verticle | 1 | 0 | 0 | 0 | Symptoms returned to baseline after ~10s |
| Convergence (Near Point) | 0 | 0 | 0 | 0 | No double vision noted |
| VOR - Horizontal | 2 | 2 | 0 | 0 | Symptoms returned to baseline after ~30s |
| VOR - Vertical | 1 | 0 | 0 | 0 | Symptoms returned to baseline after ~10s |
| Visual Motion Sensitivity Test | 2 | 2 | 0 | 0 | Symptoms returned to baseline after ~30s |
Discharge Plan
Patient has met all goals laid out at the beginning of treatment.
Discussion[edit | edit source]
Self Study Questions[edit | edit source]
The consequences of concussions can include which of the following?
a) Physical
b) Cognitive
c) Emotional
d) All of the above
Post concussion symptoms typically resolve in _________ days among adults.
a) 4-6
b) 7-10
c) 15-20
d) 10-12
The vestibular oculomotor screening test (VOMS) test the following?
a) Convergence
b) Smooth pursuits
c) Visual motion sensitivity
d) a and b
e) a and c
f) a, b, and c
References[edit | edit source]
- ↑ Post-concussion syndrome [Internet]. Mayo Clinic. Mayo Foundation for Medical Education and Research; 2017 [cited 2020May11]. Available from: https://www.mayoclinic.org/diseases-conditions/post-concussion-syndrome/symptoms-causes/syc-20353352
- ↑ 2.0 2.1 2.2 Leddy JJ, Baker JG, Willer B. Active Rehabilitation of Concussion and Post-concussion Syndrome. Physical Medicine and Rehabilitation Clinics of North America. 2016;27(2):437–54.
- ↑ Mcallister TW, Arciniegas D. Evaluation and treatment of postconcussive symptoms. NeuroRehabilitation. 2002;17(4):265–83.
- ↑ Schneider KJ, Iverson GL, Emery CA, Mccrory P, Herring SA, Meeuwisse WH. The effects of rest and treatment following sport-related concussion: a systematic review of the literature. British Journal of Sports Medicine. 2013Nov;47(5):304–7.
- ↑ Evans RW. Post-traumatic headaches. Neurologic Clinics. 2004;22(1):237–49.
- ↑ Modified Clinical Test of Sensory Interaction on Balance [Internet]. Shirley Ryan AbilityLab. [cited 2020May12]. Available from: https://www.sralab.org/rehabilitation-measures/modified-clinical-test-sensory-interaction-balance
- ↑ Springer BA, Marin R, Cyhan T, Roberts H, Gill NW. Normative Values for the Unipedal Stance Test with Eyes Open and Closed. Journal of Geriatric Physical Therapy. 2007;30(1):8–15.
- ↑ El-Kashlan HK, Shepard NT, Asher AM, Smith-Wheelock M, Telian SA. Evaluation of Clinical Measures of Equilibrium. The Laryngoscope. 1998;108(3):311–9.
- ↑ Wrisley DM, Marchetti GF, Kuharsky DK, Whitney SL. Reliability, Internal Consistency, and Validity of Data Obtained With the Functional Gait Assessment. Physical Therapy. 2004Jan;84(10):906–18.
- ↑ Wrisley DM, Kumar NA. Functional Gait Assessment: Concurrent, Discriminative, and Predictive Validity in Community-Dwelling Older Adults. Physical Therapy. 2010Jan;90(5):761–73.
- ↑ Yang M, Rendas-Baum R, Varon SF, Kosinski M. Validation of the Headache Impact Test (HIT-6™) across episodic and chronic migraine. Cephalalgia. 2010Jun;31(3):357–67.
- ↑ Mucha A, Collins MW, Elbin R, Furman JM, Troutman-Enseki C, Dewolf RM, et al. A Brief Vestibular/Ocular Motor Screening (VOMS) Assessment to Evaluate Concussions. The American Journal of Sports Medicine. 2014Aug;42(10):2479–86.
- ↑ What Is Vestibular Ocular Motor Screening? [Internet]. ReThink Concussions. 2017 [cited 2020May11]. Available from: https://rethinkconcussions.upmc.com/what-is-voms/
- ↑ Fowler Kennedy Sport Medicine. Post-Concussion Syndrome Management Guidelines. Available from: https://www.fowlerkennedy.com/wp-content/uploads/2017/02/Post-Concussion-Treatment-Guidelines.pdf (Accessed 12 May 2019)






