Periventricular Leukomalacia (PVL): Difference between revisions
No edit summary |
No edit summary |
||
| Line 9: | Line 9: | ||
== Introduction == | == Introduction == | ||
'''Periventricular Leukomalacia''' (PVL) has been cited as one of the leading causes of brain injury of a non-haemorragic nature in the cerebral white matter of the premature infant. | '''Periventricular Leukomalacia''' (PVL) is a form of brain injury occuring in both term and preterm infants. It has been cited as one of the leading causes of brain injury of a non-haemorragic nature in the cerebral white matter of the premature infant. It is an injury which can lead to deficits of physical, cognitive or behavioral deficits and is the leading cause of [[Cerebral Palsy Introduction|cerebral palsy]] in preterm infants..<ref name=":0">Volpe JJ. [https://www.nature.com/articles/pr2001219 Neurobiology of periventricular leukomalacia in the premature infant]. Pediatric research. 2001 Nov;50(5):553-62.</ref>The term leukomalacia has roots in the words 'Leukos' meaning white and 'malacia' meaning softening.<ref name=":2">Ahya KP, Suryawanshi P. [https://www.tandfonline.com/doi/full/10.2147/RRN.S125575 Neonatal periventricular leukomalacia: current perspectives]. Research and Reports in Neonatology. 2018 Jan 10:1-8.</ref> | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
| Line 38: | Line 38: | ||
# The first component is the '''focal component'''. This is characterized by localized necrosis of all cellular elements. This then leads to '''cyst formation'''. | # The first component is the '''focal component'''. This is characterized by localized necrosis of all cellular elements. This then leads to '''cyst formation'''. | ||
# The second component is the '''diffuse component'''. This is cell-specific death of oligodendroglia - those cells which will mature into oligodendrocytes (forming the myelin of the cerebral white matter). It is characterized by reactive gliosis in the surrounding white matter of the focal site. | # The second component is the '''diffuse component'''. This is cell-specific death of oligodendroglia - those cells which will mature into oligodendrocytes (forming the myelin of the cerebral white matter). It is characterized by reactive gliosis in the surrounding white matter of the focal site. | ||
By 22 weeks gestation, microglial cells (which can produce toxic inflammatory mediators, free radicals and reactive oxygen intermediates) are dispersed throughout white matter. When a PVL insult occurs, microglia become activated leading to a release of toxic products thought to lead to the death of premylinating [[Glial Cells|oligodendroglia]] in the periventricular area. There is also the death of [https://www.frontiersin.org/articles/10.3389/fnana.2020.00008/full subplate neurons] (susceptible to ischemia). These subplate neurons are important in the formation of mature thalamocortical connections. Damage to these neurons results in loss of cortical and thalamic volumes.<ref name=":1" /><ref name=":2" /> | By 22 weeks gestation, microglial cells (which can produce toxic inflammatory mediators, free radicals and reactive oxygen intermediates) are dispersed throughout white matter. When a PVL insult occurs, microglia become activated leading to a release of toxic products thought to lead to the death of premylinating [[Glial Cells|oligodendroglia]] in the periventricular area. There is also the death of [https://www.frontiersin.org/articles/10.3389/fnana.2020.00008/full subplate neurons] (susceptible to ischemia). These subplate neurons are important in the formation of mature thalamocortical connections. Damage to these neurons results in loss of cortical and thalamic volumes.<ref name=":1" /><ref name=":2" /> | ||
| Line 47: | Line 48: | ||
== Clinical Presentation == | == Clinical Presentation == | ||
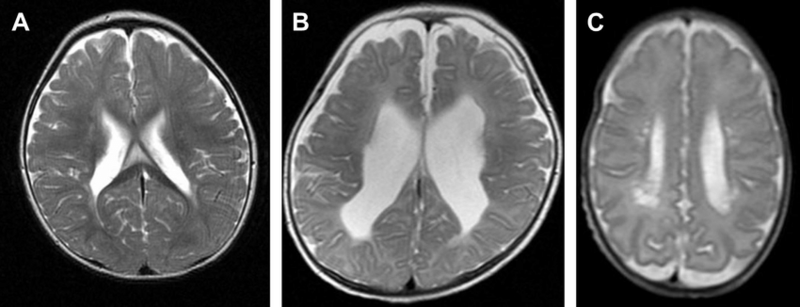
Severity of a PVL insult can be graded 1,2 or 3.<ref>Imamura T, Ariga H, Kaneko M, Watanabe M, Shibukawa Y, Fukuda Y, Nagasawa K, Goto A, Fujiki T. [https://www.sciencedirect.com/science/article/pii/S1875957213000764 Neurodevelopmental outcomes of children with periventricular leukomalacia]. Pediatrics & Neonatology. 2013 Dec 1;54(6):367-72.</ref> | |||
* Grade 1 : Abnormally high intensity (tissue appearing 'brighter') in periventricular white matter on T2-weighted images. T2-weighted MRI images are those used to highlight fatty tissue and water.<ref>Radiology Masterclass. MRI interpretation T1 vs T2 images. Available from https://www.radiologymasterclass.co.uk/tutorials/mri/t1_and_t2_images (Accessed 28th September 2023)</ref> There is also fluid-attenuated inversion recovery images. Inversion recovery sequences provide a high contrast between tissue and lesion. | |||
* Grade 2: Loss of periventricular white matter with abnormally high signal intensities, as well as ventricular enlargement adjacent to the regions of the lateral ventricles. | |||
* Grade 3: Both focal and extensive cystic changes occurring in the white matter. | |||
[[File:PVL grades.png|center|frameless|800x800px|Periventricular Leukomalacia Grading 1,2 and 3 (left to right)]] | |||
The presentation of spastic diplegia is most often linked to an incidence of PVL.<br> | The presentation of spastic diplegia is most often linked to an incidence of PVL.<br> | ||
Revision as of 20:56, 28 September 2023
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (28/09/2023)
Introduction[edit | edit source]
Periventricular Leukomalacia (PVL) is a form of brain injury occuring in both term and preterm infants. It has been cited as one of the leading causes of brain injury of a non-haemorragic nature in the cerebral white matter of the premature infant. It is an injury which can lead to deficits of physical, cognitive or behavioral deficits and is the leading cause of cerebral palsy in preterm infants..[1]The term leukomalacia has roots in the words 'Leukos' meaning white and 'malacia' meaning softening.[2]
Clinically Relevant Anatomy[edit | edit source]
add text here relating to clinically relevant anatomy of the condition
Mechanism of Injury / Pathological Process
[edit | edit source]
Incidences of PVL have been linked to:[2][3]
- Neonatal hypocarbia
- Hypotension
- Prolonged cardiac surgery
- Hypocarbia
- Patent Ductus Arteriosus (PDA)
- Inflammatory or infectious occurrences - both in the maternal or foetal system, which may increase the activity of proinflammatory cytokines.
- Sick infants where events lead to the failure of areolar autoregulation of cerebral perfusion.[3]
Between the gestational ages of 23-32 weeks, the developing brain is particularly sensitive to hypoperfusion due to a still-developing arteriol system in the brain.[2]
At 32 weeks and less (gestation age), the germinal matrix (GM) of the neonate is particularly sensitive to bleeding. [3]
Hemorrhages confined to the GM generally do not have a major effect on the prognostic outcome. When bleeding extends into the ventricles, hydrocephalus may result. If this is severe, distortion of the corticospinal tracts ensues. This has been linked to more severe spastic diplegic presentation in those affected.[3]
There are 2 components of a PVL injury.[1][2]
- The first component is the focal component. This is characterized by localized necrosis of all cellular elements. This then leads to cyst formation.
- The second component is the diffuse component. This is cell-specific death of oligodendroglia - those cells which will mature into oligodendrocytes (forming the myelin of the cerebral white matter). It is characterized by reactive gliosis in the surrounding white matter of the focal site.
By 22 weeks gestation, microglial cells (which can produce toxic inflammatory mediators, free radicals and reactive oxygen intermediates) are dispersed throughout white matter. When a PVL insult occurs, microglia become activated leading to a release of toxic products thought to lead to the death of premylinating oligodendroglia in the periventricular area. There is also the death of subplate neurons (susceptible to ischemia). These subplate neurons are important in the formation of mature thalamocortical connections. Damage to these neurons results in loss of cortical and thalamic volumes.[3][2]
Damage to the various regions of the white matter can produce deficits in motor, sensory, visual and even higher cortical functions.[2]
Epidemiology[edit | edit source]
The incidence of PVL increases with decreasing gestational age. Peak occurrence is seen between 24 and 32 weeks gestational age and in those infants weighing 1500g or less.[2]
Clinical Presentation[edit | edit source]
Severity of a PVL insult can be graded 1,2 or 3.[4]
- Grade 1 : Abnormally high intensity (tissue appearing 'brighter') in periventricular white matter on T2-weighted images. T2-weighted MRI images are those used to highlight fatty tissue and water.[5] There is also fluid-attenuated inversion recovery images. Inversion recovery sequences provide a high contrast between tissue and lesion.
- Grade 2: Loss of periventricular white matter with abnormally high signal intensities, as well as ventricular enlargement adjacent to the regions of the lateral ventricles.
- Grade 3: Both focal and extensive cystic changes occurring in the white matter.
The presentation of spastic diplegia is most often linked to an incidence of PVL.
Diagnostic Procedures[edit | edit source]
Brain imaging[edit | edit source]
Ultrasonography - Can be used in utero and postnatally. Cystic changes and increased echogenicity are indicators of PVL. After 1 week of birth, ultrasonography which yields no abnormalities can exclude PVL as a diagnosis.[3]
MRI - Can be used earlier than ultrasonography. Repeated MRIs and diffuse tension imaging can be used to determine prognostic information by tracking grey matter atrophy and tract degeneration.[3]
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
Prevention is the best form of treatment. An important aspect in this regard is ensuring arterial CO2 (PCO2)does not fall below 35mmHg. [3]
In low-birth-weight infants inhalation of NO has seen to decrease the incidence of PVL. [3]
Cooling, as done for HIE has had little attention in the research and thus has no definable outcomes.[3]
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Resources
[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Volpe JJ. Neurobiology of periventricular leukomalacia in the premature infant. Pediatric research. 2001 Nov;50(5):553-62.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Ahya KP, Suryawanshi P. Neonatal periventricular leukomalacia: current perspectives. Research and Reports in Neonatology. 2018 Jan 10:1-8.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Deng W, Pleasure J, Pleasure D. Progress in periventricular leukomalacia. Archives of neurology. 2008 Oct 13;65(10):1291-5.
- ↑ Imamura T, Ariga H, Kaneko M, Watanabe M, Shibukawa Y, Fukuda Y, Nagasawa K, Goto A, Fujiki T. Neurodevelopmental outcomes of children with periventricular leukomalacia. Pediatrics & Neonatology. 2013 Dec 1;54(6):367-72.
- ↑ Radiology Masterclass. MRI interpretation T1 vs T2 images. Available from https://www.radiologymasterclass.co.uk/tutorials/mri/t1_and_t2_images (Accessed 28th September 2023)
- ↑ Anne Hansen. Periventricular Leukomalacia. Available from: https://www.youtube.com/watch?v=069Eita-PZk [last accessed 27/09/2023]