Pelvic Floor Dysfunction
Original Editors - Sarah Barnes, Chris Van Wyk, Amy McCarthy, Gina McLoughlin, John Lavin, Claire Ramsden and Carolinne Cieslak.
Top Contributors - Sarah Barnes, Carolinne Cieslak, Gina McLoughlin, Kim Jackson, Claire Ramsden, Chris Van Wyk, Amy McCarthy, John Lavin, Vidya Acharya, Nicole Hills and Rachael Lowe
Pelvic Floor Dysfunction[edit | edit source]
Below is an overview of this physiopedia page. If you would like to skip to a certain part within the page then use the 'Contents' drop down tab at the top of the page to navigate your way to that information.
Introduction[edit | edit source]
Speaking about your nether-regions is never an easy thing to do! Problems with your pelvic floor (including incontinence, leaking, and pelvic organ prolapse) is no easy subject to bring up, especially when you are worried that there may be something wrong! Pelvic floor dysfunction is heavily underreported[1] as so many people don't feel comfortable speaking up about it.
This physiopedia page has been written to provide the public with some information on pelvic floor health, providing information on what the pelvic floor is, how to exercise it and what can happen if you don't. This patient guide also has information on how to access treatment from local NHS services, for example physiotherapy. This page has been designed to build upon previous resources available and to bring together important and valuable information on pelvic floor health, so it is all within one page for your easy reading.
Yer aff yer heid!! A am' nae talkin' about whats under ma breeks!!![edit | edit source]
Do you feel you are the only person with problems with your undercarriage?. . . .
You are not alone. Many people find talking about pelvic health to be a difficult conversation to bring up.
In fact, 41-50% of women over 40 are affected by pelvic organ prolapse (information below)[2]. Only 17% of those with urinary incontinence seek medical help[3]. Pelvic floor dysfunction affects more women than men[4], however, men are affected!!! From these figures, 46% of people suffer with their symptoms for 1 to 5 years[3], 42% of people suffering with their symptoms for 5 years or more[3].
Issues with your nether-regions are well known to have negative effects on your quality of life for both men and women [4]. Many individuals have reported negative effects on their home and work activities, personal relationships, social lives and mental well-being [1]. Pelvic floor dysfunction is also associated with depression, social isolation, anxiety and generally reduced quality of life [4].
Fear not! We have designed this patient guide to provide you with the information you need to take charge of your undercarriage and help improve your life!!
We have also designed a quick quiz (at the bottom of the page) for you to test your knowledge after reading through this guide. Have fun!!
Our mission:[edit | edit source]
To increase the public's knowledge and recognition of pelvic floor health, and empower individuals to seek professional help if they believe something to be wrong.
Our aim:[edit | edit source]
For all members of the public to understand the consequences of reduced pelvic floor health and the overall impact it has on daily activities and quality of life. Through education, we hope to empower the public to be proactive and seek advice from healthcare professionals. A partnership between the public and healthcare professionals will help individuals gain the correct tools to improve their symptoms by increasing levels of self-management.
In support of our mission, we have designed a healthcare professional section (at the bottom of the page) specifically designed for physiotherapists and members of the public who would like to read further on the subject of pelvic floor health. This section includes more detailed information on all aspects of pelvic floor dysfunction, handy treatment advice and helpful ways to discuss pelvic floor health and teach the pelvic floor exercises to patients.
Learning Outcomes[edit | edit source]
After exploring this wiki page, the reader should be able to:
Any problems with your water works?[edit | edit source]
Still feel the topic of pelvic floor health is a little awkward and uncomfortable? Not to worry here is Elaine Miller (a pelvic health physiotherapist and stand up comedian) to lighten the mood. This is Elaine's Edinburgh Fringe Festival performance Gusset Grippers. In this show she makes personal topics a more humorous topic.
Click here If you would like to know more about Elaine or her gigs.
Overview[edit | edit source]
What is the Pelvic Floor?[edit | edit source]
The pelvic floor is made up of a layer of muscles covering the bottom of the pelvis that support the bladder and bowel in men [5] and bladder, bowel and womb in women. These structures that sit on top of the pelvic floor are known as our pelvic organs. The muscles run like a hammock from the front of the pelvis to the tailbone (coccyx) at the back, and side-to-side from one sitting bone to the other [6] as can be seen in the picture below.
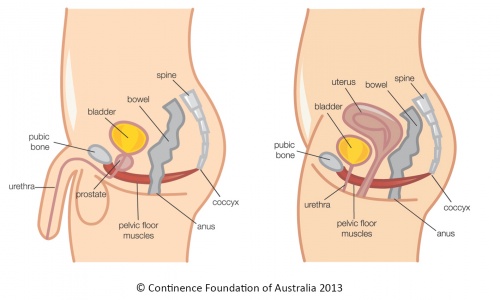
The pelvic floor muscles also have holes through which the urethra (tube through which urine (wee) exits our body from the bladder) and anus (exit at the end of our digestive system through which faeces (poo) leaves) pass through in males and urethra, anus and vagina pass through in females[6]. The muscles are snug against these structures in order to hold the passages closed. Both the anus and urethra have extra circular muscles (called sphincters) that help to keep the passages closed and prevent any unwanted leaking or stains [8].
Our pelvic floor muscles are similar to a trampoline, as they have the ability to move up and down. This occurs during breathing and is much easier to imagine if we think of our body as a cylinder. When we breath in, our diaphragm (breathing muscle) pulls down to open our lungs[9], this is like the top of the cylinder pulling down. This pushes down on our internal organs and in order to avoid squashing these organs, our pelvic floor and abdominal muscles relax and stretch down and out. This is like the bottom and sides of the cylinder stretching down and out to create more space for the organs. When we exhale, the top of the cylinder (the diaphragm) springs back to its normal position. As it does so the abdominals and pelvic floor muscles return to their normal positions. A common problem experienced by people, is holding their breath during lifting activities or bowel movements. This can lead to pelvic floor weakness or dysfunctions by adding excess stress on these muscles [10].
Click here to see a visual diagram of the diaphragm and pelvic floor muscles working together.
Functions of the Pelvic Floor Muscles:[edit | edit source]
The pelvic floor serves many important functions from being a hammock to hold our organs to stopping us from leaking and to improves your sexual experience and function. The picture and paragraph below run through some of the main functions of your pelvic floor in more detail.
- Support internal pelvic organs in the correct positions (Bladder, bowels and womb).[5][11]
- Allows self-control of bladder and bowel habits using the sphincter muscles. This allows us to control the release of urine (wee), faeces (poo) and gas. This allows us to delay emptying until a convenient time when a toilet is available. This works by the pelvic floor muscles tightening and lifting the pelvic organs up while the sphincter tightens around the openings of the urethra and anus.[5][11]
- When relaxed, they allow the passage of urine and faeces out of the body.[5][10]
- Sexual function[5]
- As mentioned before, the pelvic floor muscles play a role in breathing by relaxing and increasing the space the lungs have to expand.[10]
- During pregnancy, the pelvic floor offers support to the baby and also assists in childbirth [5]
Strong pelvic floor muscles are important when we cough, laugh, sneeze and during lifting activities as there is extra force added to the abdomen and pelvic floor[10]. If these muscles are weak, stretched or not working as they should, pelvic floor dysfunction may occur and lead to the signs and symptoms mentioned below. Some of these symptoms may be pressure felt in the pelvic region and/or bladder or bowel leaking occurring during laughing, coughing, sneezing or lifting.[13]
Signs and Symptoms of Pelvic Floor Dysfunction[edit | edit source]
There are a few well known signs and symptoms that people experience when they have a problem with their pelvic floor muscles. Many individuals have described some of these problems and feelings as normal, as they have been happening for so long. However, this shouldn't be the case!!
The following list of signs and symptoms are common for people with weak pelvic floor muscles.
Urinary dysfunction, erectile dysfunction, premature ejaculation, painful ejaculation and chronic pelvic pain are some conditions that can be linked with weak pelvic floor muscles.
Men:[edit | edit source]
- Constipation or bowel strains[14]
- Ongoing pain in your pelvic region, genitals or rectum.[15][16]
- A prolapse – may feel as though there is a bulge/ pressure in the rectum or a feeling of needing to use your bowels without actually needing to go.
- Accidentally leaking urine when you exercise, laugh, cough or sneeze.[17][18][16]
- Feelings of urgency in needing to the bathroom, or not making it there in time.[17][18][19]
- Frequent need to urinate.[19]
- Difficultly emptying your bladder (discontinuous urination – stop and start multiple times) and bowels.[19]
- The feeling of needing to have several bowel movements during a short period of time.
- Accidentally passing wind.[17]
- Pain in your lower back that cannot be explained by other causes.[17]
- Pain in the testicles, penis (referred pain from the pelvic floor) or pelvis during intercourse.[15]
- Erectile dysfunction.[15][18][16]
- Painful ejaculation.[15][18][16]
- Premature ejaculation. [15][18]
Erectile function requires contraction of the pelvic floor muscles to block blood from leaving the penis. When the muscles are weak the outflow of blood from the penis is not stopped resulting in erectile dysfunction. Through learning voluntary control of the pelvic floor muscles this can help prevent premature ejaculation by learning how to relax and contract the muscles.[20]
Urinary incontinence has a direct relationship with pelvic floor muscles. These muscles tighten as a closure mechanism for the tube from the bladder to the exit (urethra) and weakness of these muscle can cause leaking and dribbling.[21]
If you are unsure whether you have a pelvic floor dysfunction or would like further information on each sign and symptom, the following website is extremely useful!! Women's and men's health physiotherapy.
For further information on the male pelvic floor go to: Pelvic floor advice for men - download the advice leaflet. OR. Male pelvic floor.
Women:[edit | edit source]
- Pain or numbness during intercourse.[17][14][16]
- Ongoing pain in your pelvic region, genitals or rectum.
- A prolapse – may be felt as a bulge in the vagina (feeling or seeing a bulge or lump in or coming out of your vagina) or a feeling of heaviness, discomfort, pulling, dragging or dropping sensation.[17]
- Accidentally leaking urine when you exercise, laugh, cough or sneeze (stress incontinence).[16][19]
- Feelings of urgency in needing to the bathroom, or not making it there in time.[19]
- Frequent need to urinate.[17][19]
- Difficultly emptying your bladder (discontinuous urination – stop and start multiple times) and bowels.[17][19]
- The feeling of needing to have several bowel movements during a short period of time.
- Constipation or bowel strains.[14]
- Accidentally passing wind.[17]
- Pain in your lower back that cannot be explained by other causes.[17]
Prolapse is a common condition that can occur due to weak pelvic floor muscles in women. This occurs due to the womb, bladder, bowel or top of the vagina moving out of their normal positions and pushing into the vagina.This can cause pain and discomfort but can be improved with pelvic floor exercises and lifestyle changes which are mentioned in the treatment section of this wiki[22].
Urinary incontinence has a direct relationship with pelvic floor muscles. These muscles tighten as a closure mechanism for the tube from the bladder to the exit (urethra) and weakness of these muscle can cause leaking and dribbling.[21]
If you are unsure whether you have a pelvic floor dysfunction or would like further information on each sign and symptom, the following website is extremely useful!! Women's and men's health physiotherapy.
Helpful websites for further information on the signs and symptoms of pelvic floor dysfunction: Health line or Pelvic floor first.
For further support for urinary or faecal incontinence you can visit the following NHS site: Living with incontinence.
Common Misconceptions[edit | edit source]
[1]- A patient personal experience of pelvic floor dysfunction, This is an interesting, personal and relatable video that explains pelvic floor dysfunction in real life terms.
It’s my fault isn’t it?[23][edit | edit source]
Being a female in the 21st century is certainly not an easy task. The role of a woman is diverse, demanding and challenging. Women chop and change from being a mother, a lover, a homemaker to a successful business woman managing the hiring and firing in some of the worlds most successful and glamorous companies. Women are athletes, breaking records for the highest jump in the Olympic games and setting new personal bests, that challenges not only them but every other female on this planet to beat. Women are the backbone of the fashion industry, selling our souls for the latest Louis Vuitton autumn/spring collection which of course consists of utterly divine leather pants! The overall picture is, WOMEN ARE BUSY! ...
Women who experience symptoms associated with pelvic organ dysfunction such as incontinence, leaking, increase urgency and prolapse blame themselves[24]. Some women feel "deserving" of these symptoms, due to lack of consistency or failure to prioritise their pelvic floor muscle training post childbirth or throughout the ageing process due to commitments in other roles[24]. Now, lets talk about the shame that comes with this! Shame, that awful uncomfortable, just brush it under the carpet word that women associate with symptoms as mentioned above. Shame prevents reporting of such symptoms to healthcare professionals, not only due to the uncomfortable nature of the topic but interestingly, women fear they will be judged or reprimanded for failure to train pelvic floor muscles as expected over the years [23]. Eye opening, right? Some women feel that leaking, incontinence and even prolapse are "part of the parcel" of being a woman, and these are side effects that come with the job [24]. Some women accept this faith and resign to a life of incontinence wear and multiple red cheeked situations. A pelvic floor contraction.... Queue the tumbleweed! One of the more difficult things in life to explain, we can all agree with that! Some women have highlighted the difficulty communicating with healthcare professionals about how to actually do a pelvic floor contraction, resulting in poor or incorrect technique and never truly exercising their pelvic floor muscles. . . REFERENCE
The silent private exercise:[25][edit | edit source]
Many things in life can be described as mysterious, for example, the Loch ness monster, the misplacement of socks post laundry day, that diminishing tub of ice-cream in the freezer when you swear you only had one bite. But, the biggest mystery of all, the nature of a pelvic floor contraction.
Finding the appropriate yet explicit language to explain a pelvic floor contraction is not an easy task. Exercising muscles that cannot be seen, are located in a private area of the body and associated with private function are not easily discussed. Hence, the mystery that surrounds pelvic floor muscle training. A study was conducted to evaluate healthcare professionals skills at explaining pelvic floor muscle contraction to patients. One patient involved in this study, described the explanation given as "sketchy and confusing [25]. Difficulty grasping this technique has been a cause of embarrassment for woman and many feel silly as they struggle to get their head around engaging the pelvic floor muscles correctly! In an attempt to contract the pelvic floor muscle, some common errors are made. Contraction of other muscles such as the rectus abdominus (tummy muscle) glutes (bottom muscles) and adductors (inner thigh muscles) instead of the true internal pelvic floor muscles. Also, compensatory movements such as pelvic tilts, breath holding and straining can give the illusion of a pelvic floor contraction. In fact, this study found that 57% of woman incorrectly use other movements when attempting to contract the pelvic floor [24]. . Frustrating, right?
Will pelvic floor muscle training work?[25] [24][edit | edit source]
Hell yeah it works!!
Want a bigger bicep? Simple, operation bicep curl and problem solved! Dreams of that Kardashian derriere? 50 squats a day and I am as good as Kim K right? Want a stronger pelvic floor? Hell yes! See ya later incontinence !... yeah.. hmm.. okay, perhaps that is not as attractive the other examples granted. Some woman really struggle to commit to pelvic floor exercises due to the absence of noticeable benefit. No immediate or visible effect from training leads woman to feel as though there is no return for their efforts and some woman feel that pelvic floor muscle training is a waste of time[25]. And okay, granted, the nature of pelvic floor exercises is not going to set everyone's world on fire. Give me Aqua-aerobics and some Bonnie Tyler any day! Some woman find pelvic floor exercises tedious, a daily battle and downright boring. The nature of the pelvic floor contraction involves a lot of thinking about ones "private " area. And exercising that "private "area needs concentration, peace and quiet. Many woman feel uncomfortable and simply unable to exercise the pelvic floor around others[25]. Allocating time specifically to this and finding a quite place without distraction is not always easy. As a result, some woman have great difficulty factoring pelvic floor exercises into their daily routine.
Prolapse, incontinence and leaking, that's a female problem right?[26][edit | edit source]
Men are from Mars and woman are from Venus. In some respects yes! But, when it comes to the pelvic floor muscle, we all originate from the same planet! Meaning, regardless of gender pelvic floor muscle training is essential for both men and woman. Prolapse, incontinence and leakage are widely believed to be a female issue. As woman give birth and go through the process of labor, and are subject to hormonal changes throughout the ageing process, it is understandable why some men believe they can dodge the pelvic floor bullet! Unfortunately guys, that bullet is coming straight for you! Males are not exempt from pelvic floor muscle training, as the same risks apply. Studies conducted found that nearly 66% of men are unaware that males are required to do pelvic floor muscle training[26]. But please, don't panic guys, we are here to help! There is a general under reporting of symptoms within the male population when it comes to the telltale signs that all is not well in the land of the pelvic floor, stigma, embarrassment and the discomfort associated with discussing this issue prevents a lot of males from reporting these symptoms. In general, the body of evidence in this area lies within the female population, there is a lack of research investigating the male experience of pelvic floor muscle training.
Are you at risk?[edit | edit source]
There are multiple risk factors that can contribute to pelvic floor dysfunction. They can be modifiable (for ex. smoking) and non-modifiable (ex. age and genetics). A combination of changes in anatomy/physiology, genetics, and lifestyle, play a role in the presentation of pelvic floor conditions.
The common risk factors for both males and females have been illustrated in the diagram below in yellow circles. Risks unique to each gender include blue circles for males and pink for females.
Men:[edit | edit source]
1. Prostate surgery: Specific pelvic floor disorders include urinary (pee) incontinence and erectile dysfunction, which are quite common post-operatively in up to 89% of men[27]. Frequently, after the procedure, these conditions present as having poor bladder control, weakness in pelvic floor muscles (especially urinary sphincters) and changed pelvic nerve supply [28].
Women:[edit | edit source]
2. Age: Menopausal age (48-55) increases risk for developing pelvic organ prolapse by 21.1% [30][31]
3. Pregnancy and childbirth: Vaginal birth, prolonged labour, instrumental delivery (use of spoon-like tools to help baby out of birth canal), episiotomy (surgical procedure to increase opening in vagina), parity (weight and number of children) have also been known to increase the pelvic floor dysfunction risk by 4-16% [30][32][33].
4. Genetics: Women who have a family history of pelvic organ prolapse are more likely to have the condition[34]. In females who are experiencing urinary incontinence the connective tissue (supports pelvic floor) may be genetically weak[35] [36].
5. Hysterectomy (surgical removal of womb): This procedure often damages and weakens the pelvic muscles. Therefore, it is known to increase the chances of developing a pelvic organ prolapse[31] [37]. The risk of urinary incontinence after hystercetomy in middle-aged women is also increased to 60% [38].
Both Genders:[edit | edit source]
6. Pelvic floor injury: A fall causing injury to the pelvic floor muscles can result in pelvic floor weakness/dysfunction. Side effects of pelvic radiotherapy(direct radiation treatment for cancer) involve weakening of pelvic floor muscles in both men and women. In men, radiation for prostate cancer influences erectile dysfunction, and urinary incontinence[39]. For women, pelvic radiation may also lead to urinary incontinence [40].
7. Increased abdominal pressure: This can be thought of as added pressure to the stomach area, or the cylinder concept as explained in the overview. Frequent coughing (due to chronic lung disease, smoking, hay fever) and persistent sneezing cause overuse of pelvic floor muscles. This weakens pelvic floor structures and can lead to release of urine without control [41]. It is often presented as pelvic organ prolapse in women and urinary incontinence in men[32][42].
8. Constipation: Constipation is caused by changes in pelvic floor muscles and increase in abdominal pressure during bowel movement. These persistent conditions can damage nerves and appear as pelvic floor dysfunction symptoms, such as fecal (poo) incontinence[43].
9. Intense physical effort: Elite athletes who engage in high impact sports (e.g. trampolining, running, gymnastics) compared to low impact sports (e.g. golf), tend to experience increases in abdominal pressure, which over time, can lead to urinary incontinence[36][35]. Occupations that require frequent heavy lifting, add pressure to the bladder and influence urinary incontinence in both genders[45]. Women who perform prolonged heavy lifting are 9.6 times more at risk of developing pelvic organ prolapse[36].
10. Obesity: Being overweight may be associated with urinary incontinence in both genders and pelvic organ prolapse in women, compared to those with healthy weight[30][35][39]. Simple changes such as healthy diet or increased physical activity may be prescribed to reduce the risk for these conditions.
11. History of back pain: Low back pain can be related to pelvic floor muscle dysfunction. This is because the lower back and pelvic floor closely work together. Pain felt in the lower back may travel to the pelvic floor. It can prevent from using these muscles efficiently. Over time the pelvic floor muscles supporting bladder control, become weak and lead to urinary incontinence[46].
For more information, you can refer to the links provided below:
Common problems with pelvic floor muscles [48]
Treatment [edit | edit source]
Pelvic floor dysfunction is a very treatable condition. Many ways exist to treat pelvic floor problems conservatively (non-surgical) and should generally be considered as the first-line option prior to more aggressive procedures such as surgery[49][50][51]. Treatment will vary according to the nature of the condition or reason behind the dysfunction. A health care practitioner, such as your GP or a physiotherapist, will help you decide which one is best for you:
Conservative (non-surgical):[edit | edit source]
Physiotherapy & Exercise:[edit | edit source]
- Pelvic floor muscles can be trained just like any other muscle in the body for example your arm and leg muscles. Pelvic floor muscle training is a very important part of improving pelvic floor dysfunction and is valuable to both men and women[52].
- Pelvic floor exercise aims to increase the strength, endurance and co-ordination of the muscles, which improves their overall function[51]. A strong pelvic floor will help to prevent incontinence, provide support to pelvic organs and even improve your sex life![53]
- There are many different methods to assist you in training your pelvic floor muscles. A physiotherapist or GP that specialises in pelvic health is best suited to teach you how to implement these essential strategies. Some specialists combine pelvic floor exercises with other treatment techniques, for example: vaginal cones, electrical stimulation devices [53]. However, these are not always effective in all cases and access can be limited due to limited resources. BUT. . . . Pelvic floor exercises are free!!
- One of the most effective treatments to improving your pelvic floor are pelvic floor exercises. They are cheap, easy and are a great way to help self-manage.
- To exercise your pelvic floor, it's handy to think of 'lifting and squeezing' as if you're trying to stop your wee or stop from passing gas!
Please see the below for more detailed descriptions and videos on how to complete your pelvic floor exercises.
Listen up ladies, here's how to exercise your pelvic floor...[edit | edit source]
- The pelvic floor muscle can be exercised in sitting standing or lying. Some people may prefer doing it in sitting because they feel the muscle is easier to engage from this position. Try each position and see what works for you.
- From sitting, ensure both feet are placed on the floor and you are relaxed and aware of their breathing. Try to relax all muscles, including shoulders, tummy and buttock muscles. Take a few moments to become aware of breathing pattern.
Okay ladies so imagine this...
- Imagine you are sitting on the toilet, having a wee, when suddenly Ryan Gosling bursts into the bathroom cubicle. Naturally, you get a fright, and are forced to stop the flow of wee suddenly. This is a pelvic floor contraction involving the front muscles.
- Holding and clenching wind, is an example of a pelvic floor contraction involving the back muscles.
*But remember don't actually stop the flow of wee, just try to replicate the sensation. It is important to empty your bladder without interrupting the flow. Save your pelvic floor exercises for afterwards!
If you prefer to watch a video to show you how to exercise your pelvic floor, then please watch the video below (1 of 5).
Below are four more progressive pelvic floor exercise videos for you to try home and take at your own pace!:
| [54] | [55] | [56] | [57] |
Okay men, it's your turn next...[edit | edit source]
- The pelvic floor muscle can be exercised in sitting standing or lying. Some people may prefer doing it in sitting because they feel the muscle is easier to engage from this position. Try each position and see what works for you.
- From sitting, ensure both feet are placed on the floor and you are relaxed and aware of their breathing. Try to relax all muscles, including shoulders, tummy and buttock muscles. Take a few moments to become aware of breathing pattern.
- For men to engage their pelvic floor muscles, 'lifting and squeezing' as if trying to stop from passing gas or stop while urinating holds true. Men may also think of the sensation they get when walking into a cold lake or pool: when the water gets up to the level of their 'family jewels'. This sensation is the pelvic floor activating!
Watch the video below for another explanation to exercise the male pelvic floor:
For extra reading click on the following links:
Female information leaflet from the British Association of Urological Surgeons
Male information leaflet from the British Association of Urological Surgeons
Lifestyle Changes:[edit | edit source]
Healthcare professionals may suggest ways to help improve certain aspects of your condition. Here are some hints and tips we have put together that may help improve your pelvic floor health. Every little helps!
- Increasing your physical activity and improving your diet to achieve a healthier weight are great strategies to improve your pelvic floor health and overall quality of life as there will be less stress on your pelvic floor. [49]
- Quitting smoking can reduce coughing symptoms which reduces stress and strain on the pelvic floor
- Another helpful tip is to try and reduce alcoholic drinks and caffeine in your diet, as they can irritate the bladder. A good subsitiute is water (1.5L is the recommended daily intake). [58]
- The NHS has also developed a very handy app to help provide information, additional resources and even reminders about doing pelvic floor exercises! Please visit their site for more information: The Squeezy app
Certain strategies may be used in every day situations as well. For example, tightening up your pelvic floor muscles prior to lifting heavy loads, or when possible, sharing the load with another person to lighten it and reduce the strain. This will help to prevent any unwanted leakage or damage.[52] This is called the knack technique, see below.
The knack technique – Get involved people![edit | edit source]
The knack technique is an absolute gem and can help and support everyone’s pelvic floor health! Pressure builds up in the tummy when lifting, exercising, coughing, sneezing, laughing, lifting weights, turning to look out your rear window when driving, basically in pretty much everything we do! This creates a downward force or pressure on the pelvic floor muscles which can lead to our beloved internal “trampoline” becoming stretched or lax. The knack technique involves contracting the pelvic floor muscle before lifting, bending, sneezing, coughing, or any movement you can think of that will increase pressure in the tummy.This preventative measure can help maintain pelvic health.
The knack technique offers so many benefits and can help you become more aware of your pelvic health. Think about your daily activities, hobbies, family and think of situations in which the knack technique can be useful. Remember to contract the pelvic floor before lifting for example contract that pelvic floor before lifting your 2 year old teething toddler or your heavy shopping bags.
Pharmacological (medication):[edit | edit source]
- Various drugs can be prescribed depending on the reason for your pelvic floor problems.Your GP will decide with you if these are necessary. Drug therapy is particularly common for urinary incontinence and depending on the type of incontinence you’re experiencing, different medications are available[51].
- The aging process can lead to hormonal changes which can negatively impact the pelvic floor muscles and lead to increased laxity/stretching. Therefore, hormone replacement therapies for post-menopausal women can be used to manage or improve the symptoms.
- If you have an over-active bladder or urge incontinence, there are medications to help relax the bladder and reduce the frequency of urination.[59]
- Drug therapy is even more effective when used in combination with other strategies like pelvic floor exercises and lifestyle changes.[59]
For more information, please see this NHS website.
Surgical:[edit | edit source]
- In some cases, when other strategies have been unsuccessful in achieving your treatment goals, surgery may be a treatment option for you. Depending on your specific condition, various procedures exist to address the problem.
- Incontinence and prolapse have multiple types of procedures to alter the pelvic structures or insert supports such as synthetic mesh slings, both in the goal of improving functions.[2][60]
- For those who have a pelvic floor disorder, 1 in 9 will undergo surgery, however there are risks associated with surgery as they don't always succeed. Regarding synthetic mesh sling surgery, roughly 30% will require a second operation, and roughly 35% will need to be removed.[2]
- Slightly less invasive options are also available, such as injections of Botox for urge incontinence or bulking agents to help reduce stress incontinence.[61]
For more information on bladder procedures, please visit this site.
For more information on urinary incontinence procedures, please visit this NHS website.
*REMEMBER TO FIX SURGICAL
Access to services[edit | edit source]
Each NHS Board across Scotland has different processes and guidelines to get referred to a pelvic health physiotherapist. Below is an outline of the referral process in different areas in Scotland.
NHS Forth Valley:[edit | edit source]
For Women’s health you are able to self refer through the following link - Self referral form
If you are having continence problems during and after pregnancy or pelvic floor dysfunction- NHS Forth Valley ask you to complete the screening tool ICIQ Form (link below).This will help you decide if you need to be referred for a 1:1 assessment with a specialist physiotherapist. If you score more than 10 when you add the totals for questions 3, 4 and 5, Forth Valley would suggest that you print, read and complete the Pelvic Bladder Self Referral Form (link below) and send it to the physiotherapy department at either Forth Valley Royal Hospital or Stirling Community Hospital.
Pelvic Bladder self referral form
Alternately, your GP or midwife can also refer you to the services.[62] For males, please contact your GP.
NHS Lothian:[edit | edit source]
Treatment for symptoms of incontinence are offered in several departments within the Edinburgh Community Physiotherapy Service. Currently the departments offering this service are:[edit | edit source]
- Craigroyston Health Clinic
- Leith Community Treatment Centre
- Slateford Medical Practice
- South Queensferry Health Centre
- Tollcross Health Centre
Conditions which are dealt with include:[edit | edit source]
- Stress urinary incontinence (leakage on coughing, sneezing, laughing etc)
- Urgency, frequency and nocturia (needing to empty your bladder urgently and often and getting up at least twice overnight to go to the loo)
- Symptoms of mild prolapse (sensation of something coming down)
- Weak pelvic floor after childbirth including any of the above symptoms
- Men with urinary incontinence can be treated at Leith Community Treatment Centre
The service can be accessed by referral from any of the following:[edit | edit source]
- Self referral – by calling NHS 24 on the number 111 or for Bladder Problems use the Self referral form
- A referral from your GP or any Health Care Professional (nurse, midwife etc). [63]
NHS Borders:[edit | edit source]
The role of the bladder, bowel and pelvic floor service is to promote continence by offering advice, treatment and management options. This is delivered by a skilled team comprising of:
- Principal Physiotherapist
- Specialist Physiotherapist
- Service Nurse
The service can be contacted in the following ways:[edit | edit source]
- A referral from your GP
- A referral from any healthcare professional.
- Self referral- you can refer yourself by telephoning 01896 824555 and leaving your details on the confidential answer phone. [64]
NHS Highlands:[edit | edit source]
Service can be accessed by:[edit | edit source]
NHS Highlands physiotherapists have re-launched their self-referral service for incontinence and other pelvic health problems. New self-referral forms are available from GP practices throughout the Highlands.
Self-referral forms can be returned to the addresses on the form, or handed in to your nearest physiotherapy department. Alternatively, you can leave a message for Alison Clarke on 07748761847.[65]
Pelvic health Physio self referral form
NHS Tayside:[edit | edit source]
Continence Advisory and Treatment Service (CATS)[edit | edit source]
This service can help anyone suffering from incontinence.This will be provided by a healthcare professional who will advise, support and provide treatment for incontinence.
The team of specialist nurses work with the physiotherapists at the Tayside Pelvic Floor Dysfunction service to give you the best care.
Our Location[edit | edit source]
Whitehills Health and Community Care Centre, Forfar 01307 468383
Wallacetown Health Centre, Dundee 01382 443528
Drumhar Health Centre, Perth 01738 564258
Housebound Patients - contact your GP to request a District Nurse to attend your home to perform a continence assessment.
How to access the service:[edit | edit source]
A GP for referral.
Phone for advice and to discuss best option. [66]
Not in these areas:[edit | edit source]
If you live outside these areas don’t worry, you will still be able to access the help you require. Unfortunately, due to limited information available at the time of making this page we suggest making an appointment with your GP to discuss how to get you the help you need.
Conclusion:[edit | edit source]
We hope that you enjoyed this physiopedia resource about Pelvic Floor Health and Dysfunction. More importantly, we hope that you learned a lot about your pelvic floor and have a better understanding of the important role it has. If you are experiencing issues related to your pelvic floor, we hope this new knowledge and will encourage you to speak up and seek help from a healthcare specialist.We believe we have provided you with some helpful tips on self-management so you can begin to take control of your own pelvic floor and life!
Please don't forget to visit the resources we have provided throughout this page in addition to the ones below.
--leaflets from British association?
--NHS choices website, relink to squeezy app, videos of exercises, prostate Scotland
A little quiz to hopefully show yourself what you have learnt along the way, so give it a go!
1.Name 3 functions of the pelvic floor?
2.Why is having a strong pelvic floor important?
3.Can you name 3 signs and symptoms for each male and female?
4.Can you name 2 risk factors for pelvic floor dysfunction for males, females and both?
5.What 2 ways a physiotherapist may do to treat pelvic floor dysfunction?
6.Who to can you contact to get referred to pelvic floor physiotherapy?
7.What NHS approved app that was developed to help with your pelvic floor exercises?
8.Can you describe the steps to performing a pelvic floor contraction?
9.Name 2 lifestyle changes you try to aid pelvic floor function?
(Please scroll down past the next section for answers...)
Information for healthcare professionals (Physiotherapy specific)[edit | edit source]
Detailed anatomy and overview of the pelvic floor[edit | edit source]
- The pelvic floor is a funnel shaped structure covering the base of the pelvis from the pubic symphysis anteriorly to the coccyx posteriorly and stretches from one ischial tuberosity to the other. It consists of two main muscles, the levator ani and the coccygeus.[67]
- The levator ani muscle is a broad thin muscle that is made up of a group of 3 muscles, pubococcygeus, puborectalis and iliococcygeus. The muscles join in the middle of the pelvis except for at the prostrate in males and vagina and urethra in females.
- Pubococcygeus originates from both sides of the body of the pubis lateral to the puborectalis muscle and anterior to the obturator canal at the tendinous arch. It travels posterior and medial to insert onto the perineum, coccyx and anococcygeal ligament.
- Puborectalis is a U-shaped muscle that originates on both sides on the pubic body just lateral to the pubic symphysis. The muscle runs posterior and encircles the rectum so both side join together. Some fibers join the external anal sphincter. Contraction of this muscle causes the anorectal junction to bend 90 degrees. This maintains faecal continence during contraction and enables defecation on relaxation. Some fibers may extend towards the urethra in both male and females and to the vagina in females, aiding with urinary continence.
- Iliococcygeus originates from the ishial spines and posterior portion of the obturator internus. It travels posterior and medially and inserts onto the anococcygeal ligament and coccyx. [68]
- Coccygeus is also known as the ischiococcygeus muscle. It is a small muscle that makes up the posterior portion of the pelvic floor. It originates from the sacrospinous ligament and ischial spine and inserts on to the lateral borders of inferior sacrum and superior coccyx.[69]
- Urogenital Diaphragm: Deep transverse perineal, Sphincter urethrae
- Sphincters and erectile muscles of the urogenital and intestinal tract: External anal sphincter, Bulbospongiosus, Ischiocavernosus, Superficial transverse perineal
For more information on the anatomy of the pelvic floor please visit: http://teachmeanatomy.info/pelvis/muscles/pelvic-floor/
Here is a video demonstrating the anatomy of the pelvic floor muscles:
Types of Prolapse:[edit | edit source]
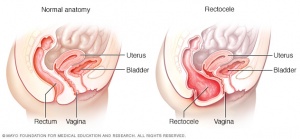
A prolapse is when a structures has slipped down from its normal position and bulges into the vagina. There are multiple types of prolapse depending on which structures have moved.
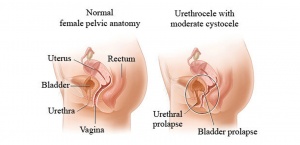
Cystocele prolapse is also known as dropped bladder and is the bulging of the bladder into the vagina (see image below). It occurs due to the weakening of the pubocervical fascia between the bladder and vaginal wall allowing the bladder to displace downwards and backwards against the anterior wall of the vagina. A pouch may also form in the bladder resulting in retention of residual urine. Symptoms include urinary frequency, incomplete emptying of the bladder, recurrent UTI’s and stress incontinence.[70]

Urethrocoele prolapse is the displacement of the female urethra into the vagina, see image below. Due to the urethra being closely attached to the anterior wall of the vagina it can sag backwards and downwards when it receives insufficient support from the vagina or surrounding fascia. This is the least common form of prolapse and is most common in post-menopausal women and pre-pubertal girls.[72]
Cystourethrocoele is a combination of a cystocoele and urethrocoele and it is the most common type of prolapse (see image below). This is when the the bladder and urethra bulge into the vagina. Symptoms may be associated with urinary stress incontinence, and urinary retention or recurrent urinary tract infections or both.[73]
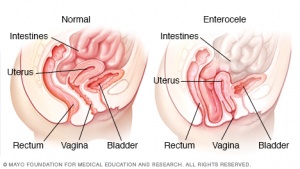
Enterocoele is when the small bowel pushes down from the abdomen onto the posterior wall of the vagina through the rectovaginal septum and causes a herniateion (Space between rectum and vagina). An enteroceoele usually accompanies a uterine prolapse.[75]
Uterine prolapse occurs when there is a lack of support allowing the uterus and cervix to descend from its normal position towards the vaginal opening and sometimes protrude out of the vagina. This can occur along with a vaginal prolapse where the vaginal vault descends due to weakening in the vaginal walls causing the vagina to invert. This prolapse is associated with a cystocoele and enterocoele prolapses. There is 3 degrees of uterine prolapse:
- First degree- the cervix remains within the vagina
- Second degree – descent if the cervix to the introitus
- Third degree- the entire uterus descends outside the introitus of the body, causing total inversion of the vagina. [70]

Rectocele prolapse occurs when the bowel and rectum bulge forwards against the lower part of the posterior wall of the vagina. Inadequate or ineffective suturing of episiotomies and perineal tear post childbirth. Constipation. Perineal splinting for bowel movement.[78]
Here is a video showing a summary of the pelvic floor anatomy and types of prolapses that can occur:
Risk factors[edit | edit source]
The chances of developing pelvic floor dysfunction among men and women have increased over the past few years. According to Berghmans et al. (2015)[81], this tendency will most likely continue. The incidence rates of individuals experiencing problems with their pelvic floor are predicted to increase by 35% between 2010-2030 [82].
These statistics emphasize the importance of expanding knowledge related to the risk factors for pelvic floor dysfunction. When assessing a patient, physiotherapists should focus on detailed subjective examination including past medical history and presenting condition/complaint, as this may reveal potential predispositions. Goal-centred conversations with the patients can provide guidance in planning a treatment, and where applicable, liaising with appropriate healthcare professionals to ensure a holistic approach to care.
Men[edit | edit source]
- Prostate surgery: In general, scientific literature examining pelvic floor dysfunction among males is limited. However, prostate surgery has been identified as a potential risk factor according to available evidence-based sources [83][84]. Specific pelvic floor disorders include urinary incontinence and erectile dysfunction, which are quite common post-operatively (up to 89% men suffer from these conditions)[27]. Individuals who undergo this procedure, may experience disturbance in pelvic floor muscles (especially urinary sphincters) and altered nerve supply to the area. In prostatectomy, the prostate (partially regulating continence) is removed, increasing probability for incontinence. The urinary sphincter nerves may occasionally be damaged during surgery due to their proximity to the prostate. As a result, the patients might later experience poor bladder control[28]. Cavernous nerves responsible for erectile function, may also be disrupted[85].
Women[edit | edit source]
- Age:Females experiencing menopause, are at increased risk for developing pelvic organ prolapse by 21.1%[30]. Wu et al. (2014)[31] assessed the relationship between age and number of pelvic floor disorders. They revealed that with each decade, the risk dramatically increased. This is most likely due to the hormonal fluctuations which change the functioning of female urogenital structures. It includes weakening of the pelvic floor, as the muscle mass tends to decrease during aging [86].
- Direct injury to levator ani (ex. vaginal delivery, fall on groin) and loss of tone in pelvic muscles: This involves the levator ani changing position and widening of genital hiatus, causing the pelvic structures to rely on the connective tissue for support. Over time, this alteration results in weakening or tearing of the tissue/collagen and may contribute to the occurrence of pelvic organ prolapse [32].
- Pregnancy and the nature of childbirth: Overstretching/damaging of the pudendal nerve during vaginal birth, prolonged labour, instrumental (foreceps) delivery,episiotomy (surgical procedure to increase opening in vagina), weight and number of children (parity) have also been known to increase the Ppelvic floor dysfunction isk by 4-16%[30][32][33]. These findings have been supported tthrough biomechanical models of the pelvic floor. The researchers revealed that during the crowning of fetal head in vaginal birth, there is a greater risk for the avulsion of levator ani leading to a potential prolapse. Additionally, episiotomy has been suggested to increase anal lacerations and therefore, incontinence risk [33]. A set of studies within the systematic review noted parity to be a risk factor for primary Ppelvic organ prolapse s well[30].
- Genetics: Women who have a positive family history of pelvic organ prolapse, are more likely to inherit the condition[34]. Campneau et al. (2011)[87], showed that the risk for pelvic organ prolapse increased 1.4 times in the genetically predisposed group, after controlling for vaginal deliveries, hysterectomy and incontinence. Additionally, evidence shows that in females who are experiencing urinary incontinence, the connective tissue of the pelvic floor muscles may be genetically weak[35][36].
- Low socioeconomic status: This factor, especially among racial minorities, may contribute to poorer access to adequate information regarding pelvic floor dysfunction[31] [32].The lack of resources create a challenge in recognizing the symptoms and importance of seeking professional support in a timely manner. Hartigan and Smith (2018)[88], presented that women of poorer socioeconomic status scored lower on the incontinence quiz than their higher socioeconomic status counterparts. Consequently, there is a strong emphasis on public education to reduce the risk of pelvic floor dysfunction.
- Hysterectomy (surgical removal of uterus): This procedure often damages and weakens the pelvic muscles. Therefore, it is known to increase chances of being more predisposed topelvic organ prolapse [31] [37]. In the study group, the incidence of postoperative complications after hysterectomy, including urinary and fecal incontinence was significantly higher than in the control group[37]. Being middle-aged, as an additional factor to post-hysterectomy, increases the risk to 60% for developing urinary incontinence[38] .
Both genders[edit | edit source]
- Previous trauma to pelvic region (e.g. fall or pelvic radiotherapy): This is particularly common in less physically active men who underwent pelvic radiotherapy for prostate cancer. The side effects of the treatment, including decreased tone of pelvic floor muscles, are more prominent in this group of patients. As a result of the pelvic muscles weakening, men are more susceptible to experience erectile impairment and urinary incontinence symptoms[39]. In women, pelvic radiation, as suggested by Walters (2017)[40] has created an additional risk factor for urinary incontinence and for developing pelvic floor dysfunction symptoms. In order to assure quality of life and avoid many discomforts, men and women should require further screening to receive the optimal treatment.
- Increased abdominal pressure: Chronic coughing (symptom of chronic lung disease, smoking, hay fever) and frequent sneezing, have been shown to contribute to pelvic organ prolapse in women[32]. It has been related to overuse of pelvic floor muscles and ligaments supporting the pelvic organs that occurs as the pressure increases within the abdomen. This weakens the anatomical structures and leads to pelvic organ prolapse [42]. For men, it usually presents as urinary incontinence. The frequent increase in intra-abdominal pressure can lead to opening of the sphincter, despite absence of bladder contraction[40].
- Constipation/heavy lifting: Constipation is caused by the altered mechanics (incoordination) of the pelvic floor muscles and increase in intra-abdominal pressure during attempted evacuation. These persistent conditions can lead to nerve damage and appearance of pelvic floor dysfunction symptoms, such as fecal incontinence[89]. Occupations that require frequent heavy lifting, add pressure to the bladder and influence urinary incontinence in both genders[45]. Evidence also shows that women who perform prolonged heavy lifting, are 9.6 times more at risk of developing pelvic organ prolapse[36].
- Prolonged vigorous physical exertion: Elite athletes, engaging in high impact sports (e.g. trampolining, running, gymnastics) compared to low impact sports (e.g. golf), have reported to experience an increase in abdominal pressure through overstretching/overloading of the pelvic floor muscles. Over time the strain and changes in strength of pelvic floor muscles, have shown to be a potential risk for urinary incontinence[35][36][90]. The implications were also suggested in a study that compared women training competitively on a weekly basis with a non-athletic group. The authors found that athletes were 2.5 times more likely to develop urinary incontinence than the non-athletic group[36].
- Increased BMI (above 25)/Obesity: Being overweight as measured by BMI, was strongly associated with urinary incontinence symptoms in both genders as was true for pelvic organ prolapse in women, compared to those with normal BMI values (18.5-24.9)[30][35][39]. With every 5 unit increase in BMI, the urinary incontinence risk rises to 20-70%. This is because of the increased intra-abdominal pressure that adds vesical compression and urethral movement. The continued weakening of pelvic floor muscles, nerve supply, and supporting structures, contribute to ineffective function[91].
- History of back pain: Low back pain has been noted to be closely related to pelvic floor muscle dysfunction. This is because the pelvic muscles have a role of providing stability for the lower back and bladder control continence. As a result, the discomfort experienced may cause individuals to avoid movement including the use of pelvic floor muscles. These muscles then become weak, unable to support the pelvic floor organs and alter urinary function. The researchers have found that due to pain levels in the low back, participants’ abilities to maximally contract the pelvic floor muscles was limited. Additionally, low back pain was attributed to loss of motor control in pelvic floor muscles, presenting as genito-urinary dysfunctions (i.e.urinary incontinence)[46].
- Implications:
- Urinary incontinence affects 69% of those with pelvic floor disorders. - PT
- Faecal incontinence affects 3.6 per 100,000 women aged 60-89. -PT
Financial burden:[edit | edit source]
- Physiotherapists, and other healthcare professionals, have an important role in reducing the financial constraints placed on the NHS. It is now understood that physiotherapists can improve patient outcomes predominantly through promoting self-management[92]. This can be done through education on pelvic floor muscle training and lifestyle modifications which have already been described. Future focus on these areas should have a positive financial impact to the NHS.
- Currently, pelvic floor dysfunction has a huge financial burden to both the patient and the health service. Recent data on the exact costs for Scotland was not identified and the costs to the NHS as a whole do not appear to be well established. This may be due to the difficulty in quantifying the overall costs including direct costs (incontinence pads, diagnostic costs, treatment costs) and indirect costs (lost wages, lost productivity due to absenteeism)[93]. However, some data does exist which gives us an indication of the problem.
- Hagen et al (2014) highlight that about 29,000 prolapse repairs were done in England between 2010 and 2011 which cost around £60 million[94].
- Estimations for the UK have been made by examining other countries data. For example, Cooper et al (2015) note that urinary incontinence in Sweden and the US accounts for 2% of their healthcare budget[3]. They highlight that 2% of the UK budget would equate to £2.1 billion.
- Milsom et al (2014) reviewed the combined economic burden of urinary incontinence to several countries[93]. Their findings indicate that for Canada and five European countries including the UK the combined cost was €7 billion a year with the UK accounting for €595 million of this total.
- Other evidence reviewed suggested that the combined burden for five European countries including the UK was €2.9 billion[93]. Interestingly, the review also noted that the cost of urinary incontinence is expected to rise by 25% in the next ten years due to the aging population[93].
- Overall the financial burden that pelvic floor dysfunction places on the NHS is very evident. Physiotherapists may have a potential role in reducing this burden through both their treatments and through promoting self management. The effectiveness of these types of interventions will be reviewed in a later section.
- Incontinence and pelvic floor exercises, surgery for (Critique and synthesis papers) (Who most benefits from PFE)
- Child birth
- Neuro-post stroke- PT more focused on mobility
- Age- Elderly
- Males- Erectile dysfunction, post surgery
- Summary of where more research needs to be done and PFE need to be incorporated in to
- More teaching of PFH in university.
- Emerging role of physio within stroke, elderly and long term care patients to increase PFE and decrease incontinence
- ?most research has been in child birth females and lacking in elderly, stroke and males
- Prevalence and impact for NHSThere is a lack of research of evidence surrounding pelvic floor health from a physiotherapy perspective; most research exists from nursing etc.
Evidence for physiotherapy[edit | edit source]
Physiotherapy is often a first line of treatment for those who are diagnosed with a form of pelvic floor dysfunction. Although the literature in this area is limited, there is some evidence highlighting the importance of physiotherapy. The research has mainly focused on the role that physiotherapists can play through education on lifestyle modifications and through exercise prescription. Evidence which was identified for both of these areas is summarised below.
Lifestyle:
- Weight loss is associated with improvements in urinary incontinence, particularly when combined with exercise[92].
- Strenuous activity or heavy lifting may be a predisposing factor for prolapse. There is limited evidence to support this and recommendations appear to be based on an understanding of the anatomy and physiology of prolapse[95].
- Some evidence suggests that decreasing fluid intake by 25% may decrease frequency, urgency and nocturia but may not improve incontinence[92].
- Caffeine reduction has been suggested to alleviate incontinence. However, the evidence for this is limited. A review by Gurovich et al (2016) found that caffeine restriction did not improve urinary incontinence symptoms[96]. Other evidence from Gleeson et al (2013) suggests that urinary incontinence is more prevalent in those with high caffeine intake[97]. Reducing caffeine intake may reduce overall fluid intake which may be the mechanism leading to improved symptoms. For this reason, reducing caffeine may be useful.
- The NICE guidelines recommend a trial of caffeine reduction in women with overactive bladder, to trial higher or lower fluid intake in women with UI or overactive bladder and recommend losing weight if BMI is over 30[98].
Exercise:
- Pelvic floor muscle training has been shown to be beneficial for both urinary incontinence and prolapse symptoms. Findings from a review by Dumoulin et al (2015) suggest that pelvic floor muscle training provides better outcomes compared to a control group in women with urinary incontinence[99]. Li et al (2016) found that those with pelvic organ prolapse undertaking pelvic floor muscle training had significantly greater improvements in subjective prolapse symptoms and objective prolapse severity compared to a control group[100].
- Pelvic floor training also seems to improve sexual function. The findings from a review by Ferreira et al (2015) suggest that pelvic floor muscle training can improve sexual function or at least one sexual variable in women with pelvic floor dysfunction[101].
- Interesting findings from two RCTs also corroborate the evidence for pelvic floor muscle training[102][94]. Alves et al (2015) found that twelve group sessions of pelvic floor muscle training increased pelvic floor muscle contractility (p = 0.01) while decreasing urinary symptoms (p < 0.01) and anterior pelvic organ prolapse (p = 0.03)[102]. Hagen et al (2014) found similar results with one to one sessions[94]. They did note that longer term investigations are required to strengthen the evidence.
- When prescribing a pelvic floor muscle training programme, adherence is important. According to a consensus statement by Dumoulin et al (2015), a structured PFMT programme, an enthusiastic physiotherapist, audio prompts, use of established theories of behavior change, and user-consultations seem to increase adherence[103].
- The identified evidence fails to make any recommendations on the optimal dosage of pelvic floor muscle training.
- The NICE guidelines recommend a trial supervised PFMT programme for at least 3 months as first line treatment for those with stress or urinary incontinence[98]. At least 8 contractions three times a day[98].
Synthesis
- Overall, the body of evidence for lifestyle modifications appears to be quite weak and the overall efficacy remains inconclusive. It seems that adjusting fluid intake may be a useful strategy and reducing caffeine intake may help to achieve this. Some evidence also supports weight loss but the justification for its use seems to be largely based on mechanistic evidence. It is worth noting that no adverse events were associated with any of the above methods and so they may be worth incorporating as a trial to gauge the patients response. Currently, the NICE guidelines seem to be the best practice to follow here.
- The evidence for pelvic floor muscle training shows largely positive results. This seems to be an effective strategy for prolapse and urinary incontinence symptoms and for sexual function. Both group and individual sessions have been efficacious and may depend on the patients personal preference. For optimal adherence, the physiotherapist should be enthusiastic, could consider using prompts to help with technique, understand and utilise behaviour change techniques and consult regularly with their patients. Currently, the dosage of therapy is not well established. However, the NICE recommendations of 8 contractions three times a day seems to be effective and was commonly used in the research.
Limitations and future research
- The evidence on pelvic floor dysfunction is lacking with the vast majority of the research focusing on urinary incontinence in particular.
- There is little evidence showing the effectiveness of lifestyle interventions. A lot of recommendations appear to be based on mechanistic and anecdotal evidence.
- Although pelvic floor muscle training appears to be effective, the optimal type and dosage of this training has not been established.
- Almost all of the literature, and guidelines, on pelvic floor dysfunction focuses on the female population. Far more research is required in the male population.
Quiz answers
1.Name 3 functions of the pelvic floor? Any of the following
- Support internal pelvic organs in the correct positions (Bladder, bowel and vagina).
- Allow conscious control of bladder and bowel habits using the sphincter muscles. This allows us to control the release of urine (wee), faeces (poo) and gas and to delay emptying until a convenient time. This works as the pelvic floor muscles contract and the pelvic organs are lifted up. The sphincter then tightens around the openings of the urethra and anus.
- Allow the passage of urine and faeces out of the body due to the pelvic floor muscles relaxing and allowing the passages to open.
- Sexual function
- In males the pelvic floor muscles are important in erectile function by increasing rigidity and ejaculation by improving control and coordination between circulation, pelvic floor muscles.
- In females voluntary contraction of the pelvic floor muscles can contribute to sexual sensation.
- As mentioned above the pelvic floor muscles play a role in breathing by relaxing and increasing the space the lungs have to expand.
- Additionally in pregnant women the pelvic floor offers support to the foetus during pregnancy and also assists in the childbirth process.
2.When and why is having a strong pelvic floor important?
- During coughing, laughing, sneezing or during lifting activities there is extra force added to the abdomen and therefore additional pressure down onto the pelvic floor
3.Can you name 3 signs and symptoms for each male and female?any of the following
Male
- Constipation or bowel strains
- Ongoing pain in your pelvic region, genitals or rectum.
- A prolapse – may feel as though there is a bulge/ pressure in the rectum or a feeling of needing to use your bowels without actually needing to go. - Accidentally leaking urine when you exercise, laugh, cough or sneeze.
- Feelings of urgency in needing to the bathroom, or not making it there in time.
- Frequent need to urinate.
- Difficultly emptying your bladder (discontinuous urination – stop and start multiple times) and bowels.
- The feeling of needing to have several bowel movements during a short period of time.
- Accidentally passing wind.
- Pain in your lower back that cannot be explained by other causes.
- Pain in the testicles, penis (referred pain from the pelvic floor) or pelvis during intercourse.
- Erectile dysfunction.
- Painful ejaculation.
- Premature ejaculation.
Female
- Pain or numbness during intercourse.
- Ongoing pain in your pelvic region, genitals or rectum.
- A prolapse – may be felt as a bulge in the vagina (feeling or seeing a bulge or lump in or coming out of your vagina) or a feeling of heaviness, discomfort, pulling, dragging or dropping sensation.
- Accidentally leaking urine when you exercise, laugh, cough or sneeze (stress incontinence).
- Feelings of urgency in needing to the bathroom, or not making it there in time.
- Frequent need to urinate.
- Difficultly emptying your bladder (discontinuous urination – stop and start multiple times) and bowels.
- The feeling of needing to have several bowel movements during a short period of time.
- Constipation or bowel strains.
- Accidentally passing wind.
- Pain in your lower back that cannot be explained by other causes.
- 4.Can you name 2 risk factors for pelvic floor dysfunction for males, females and both? Any of the following
Male:
- Prostate surgery
Women:
- Age: Menopausal age (48-55)
- Pregnancy and the nature of childbirth
- Genetics and family history
- Hysterectomy (surgical removal of uterus)
Both Genders:
- Previous injury to pelvic region (e.g. fall or pelvic radiotherapy)
- Increased abdominal pressure
- Constipation/heavy lifting
- Intense physical effort
- Obesity
- History of back pain
5.What 2 ways a physiotherapist my do to treat pelvic floor dysfunction?
- Teach you about how to do your pelvic floor exercise
- Advice of lifestyle modifications you can try
6.Who to can you contact to get referred to pelvic floor physiotherapy?
- Area dependant:
- Self referral
- GP referral
- Midwife referral
7.What NHS approved app that was developed to help with your pelvic floor exercises?
- Squeezy
8.Can you describe the steps to performing a pelvic floor contraction
*******Will add this in when its in the treatment section
9.Name 2 lifestyle changes you try to aid pelvic floor function?
- Reduce caffeine and other irritants of the bladder
- The “knack”
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 ABRAMS, P., SMITH, A.P. and COTTERILL, N., 2015. The impact of urinary incontinence on health‐related quality of life (HRQoL) in a real‐world population of women aged 45–60 years: results from a survey in France, Germany, the UK and the USA. BJU International. vol. 115, no. 1, pp. 143-152.
- ↑ 2.0 2.1 2.2 MAXWELL, M., SEMPLE, K., WANE, S., ELDERS, A., DUNCAN, E., ABHYANKAR, P., WILKINSON, J., TINCELLO, D., CALVELEY, E. and MACFARLANE, M., 2017. PROPEL: implementation of an evidence based pelvic floor muscle training intervention for women with pelvic organ prolapse: a realist evaluation and outcomes study protocol. BMC Health Services Research. vol. 17, no. 1, pp. 843.
- ↑ 3.0 3.1 3.2 3.3 COOPER, J., ANNAPPA, M., QUIGLEY, A., DRACOCARDOS, D., BONDILI, A. and MALLEN, C., 2015. Prevalence of female urinary incontinence and its impact on quality of life in a cluster population in the United Kingdom (UK): a community survey. Primary Health Care Research & Development. vol. 16, no. 4, pp. 377-382.
- ↑ 4.0 4.1 4.2 BEDRETDINOVA, D., FRITEL, X., ZINS, M. and RINGA, V., 2016. The effect of urinary incontinence on health-related quality of life: is it similar in men and women? Urology. vol. 91, pp. 83-89.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 CONTINENCE FOUNDATION OF AUSTRALIA., 2018. Pelvic Floor Muscles in Men [online] [viewed 28 March 2018] Available from:https://www.continence.org.au/pages/pelvic-floor-men.html
- ↑ 6.0 6.1 PELVIC FLOOR FIRST., 2016. The Pelvic Floor [online] [viewed 23 March 2018]. Available from:http://www.pelvicfloorfirst.org.au/pages/the-pelvic-floor.html
- ↑ CONTINENCE FOUNDATION OF AUSTRALIA., 2018. Pelvic Floor Muscles [online] [viewed 6 April 2018]. Available from:https://www.continence.org.au/pages/how-do-pelvic-floor-muscles-help.html
- ↑ PELVIC OBSTETRIC AND GYNAECOLOGICAL PHYSIOTHERAPY., 2016. Pelvic Floor Muscles Exercise for Men [online] [viewed 22 March 2018]. Available from:http://pogp.csp.org.uk/publications/pelvic-floor-muscle-exercises-men
- ↑ PELVIC CORE FIRST., 2016. The Pelvic Floor and Core [online] [viewed 29 March 2018]. Available from:http://www.pelvicfloorfirst.org.au/pages/the-pelvic-floor-and-core.html
- ↑ 10.0 10.1 10.2 10.3 PELVIC HEALTH AND REHAB CENTRE., 2017. Understanding Pelvic Floor Movement [online] [Viewed 28 March 2018]. Available from:https://www.pelvicpainrehab.com/low-tone-pelvic-floor-dysfunction/4587/pelvic-floor-movement/
- ↑ 11.0 11.1 11.2 11.3 FOUNDATION PHYSIOTHERAPY., 2018. 5 Basic Functions of your Pelvic Floor [online] [viewed 29 March 2018]. Available from:http://www.foundationphysio.com/5-basic-functions-of-your-pelvic-floor/
- ↑ PROSTATE.NET., 2016. Erectile Dysfunction and the Pelvic Floor Connection [online] [viewed 19 March 2018]. Available from: https://prostate.net/articles/erectile-dysfunction-pelvic-floor-connection
- ↑ BETTER HEALTH CHANNEL., 2017. Pelvic Floor [online] [viewed 28 March 2018]. Available from:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pelvic-floor
- ↑ 14.0 14.1 14.2 HEALTHLINE., 2017. Pelvic Floor Dysfunction [online] [viewed 26 March 2018]. Available from: https://www.healthline.com/health/pelvic-floor-dysfunction#symptoms
- ↑ 15.0 15.1 15.2 15.3 15.4 MALE PELVIC FLOOR., 2012. Male Pelvic Floor - Advanced Massage and Bodywork [online] [viewed 26 March 2018]. Available from: http://malepelvicfloor.com/sd.html
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 WOMEN'S AND MEN'S HEALTH PHYSIOTHERAPY., 2017. Leading the way in pelvic health [online] [viewed 28 March 2018]. Available from: http://www.wmhp.com.au/
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 17.8 17.9 PELVIC FLOOR FIRST., 2017. Pelvic Floor First [online] [viewed 26 March 2018]. Available from: http://www.pelvicfloorfirst.org.au/pages/how-can-i-tellif-i-have-a-pelvic-floor-problem.html
- ↑ 18.0 18.1 18.2 18.3 18.4 PELVIC OBSTECTRIC AND GYNAECOLOGICAL PHYSIOTHERAPY., 2016. Pelvic floor muscle exercises (for men) [online] [viewed 26 March 2018]. Available from: http://pogp.csp.org.uk/publications/pelvic-floor-muscle-exercises-men
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 NHS CHOICES., 2017. Living with incontinence [online] [viewed 28 March 2018]. Available from: https://www.nhs.uk/Livewell/incontinence/Pages/Livingwithincontinence.aspx
- ↑ MALE PELVIC FLOOR., 2012. Sexual Dysfunction and the Male Pelvic Floor [online] [viewed 29 March 2018]. Available from:http://malepelvicfloor.com/sd.html
- ↑ 21.0 21.1 MALE PELVIC FLOOR., 2012. Urinary Dysfunction and the Male Pelvic Floor [online] [viewed 29 March 2018]. Available from:http://malepelvicfloor.com/urinary.html
- ↑ NHS CHOICES., 2018. Pelvic Organ Prolapse Overview [online] [viewed 29 March 2018]. Available from: https://www.nhs.uk/conditions/pelvic-organ-prolapse/
- ↑ 23.0 23.1 HAY-SMITH, E., RYAN, K. and DEAN, S., 2007. The silent, private exercise: experiences of pelvic floor muscle training in a sample of women with stress urinary incontinence. Physiotherapy. vol. 93, no. 1, pp. 53-61.
- ↑ 24.0 24.1 24.2 24.3 24.4 .MASON, L., GLENN, S., WALTON, I. and HUGHES, C., 2001. The instruction in pelvic floor exercises provided to women during pregnancy or following delivery. Midwifery. 2001, vol. 17, no. 1, pp. 55-64.
- ↑ 25.0 25.1 25.2 25.3 25.4 NEELS, H., DE WACHTER, S., WYNDAELE, J., VAN AGGELPOEL, T. and VERMANDEL, A., 2018. Common errors made in attempt to contract the pelvic floor muscles in women early after delivery: A prospective observational study. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 01, vol. 220, pp. 113-117.
- ↑ 26.0 26.1 HIRSCHHORN, A.D., KOLT, G.S. and BROOKS, A.J., 2013. Barriers and enablers to the provision and receipt of preoperative pelvic floor muscle training for men having radical prostatectomy: a qualitative study. BMC Health Services Research. vol. 13, no. 1, pp. 305.
- ↑ 27.0 27.1 DOREY,G., 2013. Pelvic floor exercises after radical prostatectomy. British Journal of Nursing.October,vol.14, no.5, pp.457-464.
- ↑ 28.0 28.1 HOYLAND, K., VASDEV, N., ABROF, A. and BOUSTEAD, G., 2014. Post-radical prostatectomy incontinence: etiology and prevention. Reviews in urology. October, vol.16, no.4, p.181-188.
- ↑ DURAN, S., 2014. Pregnant Woman [online]. [viewed 04 April 2018]. Available from: https://dribbble.com/shots/1447791-Pregnant-Woman
- ↑ 30.0 30.1 30.2 30.3 30.4 30.5 30.6 VERGELDT, T.F., WEEMHOFF, M., INTHOUT, J. and KLUVIERS, K.B., 2015. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. International urogynecology journal. November, vol.26, no.11, pp.1559-1573.
- ↑ 31.0 31.1 31.2 31.3 31.4 WU, J.M., VAUGHN, C.P., GOODE, P.S., REDDEN, D.T., BURGIO, K.L., RICHTER, H.E. and MARKLAND, A.D., 2014. Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstetrics and gynecology, January, vol. 123, no.1, p.141-148.
- ↑ 32.0 32.1 32.2 32.3 32.4 32.5 KUNCHARAPU, I., MAJERONI, B.A. and JOHNSON, D.W., 2010. Pelvic organ prolapse. Am Fam Physician. May, vol.81, no.9, pp.1111-1117.
- ↑ 33.0 33.1 33.2 HANDA, V.L., BLOMQUIST, J.L., McDERMOTT, K.C., FRIEDMAN, S. and MUNOZ, A., 2012. Pelvic floor disorders after childbirth: effect of episiotomy, perineal laceration, and operative birth. Obstetrics and gynecology. February,vol.119, no.2, p.233-239.
- ↑ 34.0 34.1 LINCE, S.L., van KEMPEN, L.C., VIERHOUT, M.E. and KLUVIERS, K.B., 2012. A systematic review of clinical studies on hereditary factors in pelvic organ prolapse. International urogynecology journal. October, vol.23, no.10, pp.1327-1336.
- ↑ 35.0 35.1 35.2 35.3 35.4 35.5 BO, K., 2012. Urinary incontinence, pelvic floor dysfunction, exercise and sport. Sports Medicine. June,vol.34, no.7, pp.451-464.
- ↑ 36.0 36.1 36.2 36.3 36.4 36.5 36.6 NYGAARD, I.E. and SHAW, J.M., 2016. Physical activity and the pelvic floor. American Journal of Obstetrics & Gynecology. February, vol. 214, no.2, pp.164-171.
- ↑ 37.0 37.1 37.2 LUKANOVIC, A. and DRAZIC, K., 2010. Risk factors for vaginal prolapse after hysterectomy. International Journal of Gynecology & Obstetrics. July, vol.110, no.1, pp.27-30.
- ↑ 38.0 38.1 HUMALAJARVI, N., AUKEE P., KAIRALUOMA, M.V., STACH-LEMPINEN, B., SINTONEN, H., VALPAS, A. and HEINONEN, P.K., 2014. Quality of life and pelvic floor dysfunction symptoms after hysterectomy with or without pelvic organ prolapse. European Journal of Obstetrics and Gynecology and Reproductive Biology. November, vol.182, no.1, pp.16-21.
- ↑ 39.0 39.1 39.2 39.3 THOMAS, R.J., HOLM, M., WILLIAMS, M., BOWMAN, E., BELLAMY, P., ANDREYEV, J. and MAHER, J., 2013. Lifestyle factors correlate with the risk of late pelvic symptoms after prostatic radiotherapy. Clinical Oncology. April, vol. 25, no.4, pp.246-251.
- ↑ 40.0 40.1 WALTERS, M.D., 2017. Pelvic floor disorders in women: an overview. Revista de Medicina de la Universidad de Navarra. October, vol. 48, no. 4, pp.9-18.
- ↑ KHANDELWAL, C. and KISTLER, C., 2013. Diagnosis of urinary incontinence. Am Fam Physician. April, vol. 87, no.8, pp.543-550.
- ↑ 42.0 42.1 CHOI, K.H. and HONG, J.Y., 2014. Management of pelvic organ prolapse. Korean journal of urology. November, vol.55, no.11, pp.693-702.
- ↑ JAMSHED, N., LEE, Z.E. and OLDEN, K.W., 2011. Diagnostic approach to chronic constipation in adults. American family physician. August, vol. 84, no.3, p.299-306.
- ↑ COBB, R.,2018. Animation LOL GIF by Robbie Cobb [online]. [viewed 04 April 2018]. Available from: https://giphy.com/gifs/laugh-dennys-diner-3oEduQQQAR2a4y6Cek
- ↑ 45.0 45.1 NASER, S.S.A. and SHAATH, M.Z., 2016. Expert system urination problems diagnosis. World Wide Journal of Multidisciplinary Research and Development, vol.2, no.5, pp.9-19.
- ↑ 46.0 46.1 ARAB, A.M., BEHBAHANI, R.B., LORESTANI, L. and AZARI, A., 2010. Assessment of pelvic floor muscle function in women with and without low back pain using transabdominal ultrasound. Manual therapy. June, vol.15, no.3, pp.235-239.
- ↑ PELVIC FLOOR FIRST., 2017. Who's at risk? [online] [viewed 28 March 2018]. Available from: www.pelvicfloorfirst.org.au/pages/are-you-at-risk.html
- ↑ CONTINENCE FOUNDATION OF AUSTRALIA., 2018. Common problems with pelvic floor muscles [online] [viewed 28 March 2018]. Available from: https://www.continence.org.au/pages/what-can-happen-to-the-pelvic-floor-muscles.html
- ↑ 49.0 49.1 CLEVELAND CLINIC., 2018. Pelvic floor dysfunction. [online]. [viewed March 10, 2018]. Available from: https://my.clevelandclinic.org/health/diseases/14459-pelvic-floor-dysfunction/management-and-treatment
- ↑ ROBERT, M., and ROSS, S., 2006. Conservative management of urinary incontinence. Journal of Obstetrics and Gynaecology Canada. Vol. 28 (12), pp. 1113-1118.
- ↑ 51.0 51.1 51.2 AYELEKE, R., HAY-SMITH, E. & OMAR, M., 2015. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database of Systematic Reviews.
- ↑ 52.0 52.1 KNOWLES, K., 2018. Pelvic floor Dysfunction [online]. PHYSIOWORKS [viewed online March 26, 2018]. Available from: https://physioworks.com.au/Injuries-Conditions/Regions/pelvic-floor-dysfunction
- ↑ 53.0 53.1 PHYSIOTHERAPY NEW ZEALAND., 2018. How Physio can help: Pelvic Floor Disorders. [online]. [viewed March 10, 2018]. Available from: http://physiotherapy.org.nz/your-health/how-physio-can-help/pelvic-floor-disorders
- ↑ USMLEFastTrack. Progressive PFE Episode 2. Available from: https://www.youtube.com/watch?v=lwM_wwjerv8&list=PLqo18HBnle8zPU3gLkr9l49iAotngDB21&index=7 [last accessed 10/03/18]
- ↑ USMLEFastTrack. Progressive PFE Episode 3. Available from: https://www.youtube.com/watch?v=lp0ND0s3ZHQ&list=PLqo18HBnle8x4NKtYCobjU3DYmnJrOJA-&index=3 [last accessed 10/03/18]
- ↑ USMLEFastTrack. Progressive PFE Episode 4. Available from: https://www.youtube.com/watch?v=wRKhtfbJHdo [last accessed 10/03/18]
- ↑ USMLEFastTrack. Progressive PFE Episode 5. Available from: https://www.youtube.com/watch?v=OKvP3C8-Jxc&index=5&list=PLqo18HBnle8x4NKtYCobjU3DYmnJrOJA-[last accessed 10/03/18]
- ↑ SASKATCHEWAN MINISTRY OF HEALTH, 2014. Information for women about urinary incontinence and vaginal prolapse. [online]. [viewed March 26, 2018]. Available from: http://www.sasksurgery.ca/pdf/self-management-incontinence.pdf
- ↑ 59.0 59.1 NHS., 2018. Urinary Incontinence. [online]. [viewed March 10, 2018]. Available from: https://www.nhs.uk/conditions/urinary-incontinence
- ↑ NHS, 2018. Urinary Incontinence - Surgery and Procedures [online]. [viewed March 26, 2018]. Available from: https://www.nhs.uk/conditions/urinary-incontinence/surgery/
- ↑ NATIONAL INSTITUTE OF CHILD HEALTH AND HUMAN DEVELOPMENT, 2018. How are pelvic floor disorders commonly treated? [online]. [viewed March 26, 2018] Available from: https://www.nichd.nih.gov/health/topics/pelvicfloor/conditioninfo/treatment
- ↑ NHS FORTHVALLEY., 2018. Pelvic Floor dysfunction. [online]. [Viewed March 8, 2018]. Available from: https://nhsforthvalley.com/health-services/az-of-services/maternity/womens-health-physiotherapy/continence-during-and-following-pregnancy/
- ↑ NHS LOTHIAN., 2018. Continence. [online]. [Viewed March 16, 2018]. Available from: http://www.nhslothian.scot.nhs.uk/Services/A-Z/ECPS/ClinicsServices/Pages/Continence.aspx
- ↑ NHS BORDERS., 2018. Bladder, Bowel and pelvic floor service. [online]. [Viewed April 3, 2018]. Available from: http://www.nhsborders.scot.nhs.uk/patients-and-visitors/our-services/allied-health-professionals/bladder,-bowel-and-pelvic-floor-service/
- ↑ NHS HIGHLAND., 2018. Physiotherapy – NHS Highland. [online]. [Viewed April 10, 2018]. Available from: http://www.nhshighland.scot.nhs.uk/Services/Pages/Physiotherapy-Raigmore.aspx
- ↑ NHS TAYSIDE., 2018. Continence Advisory and Treatment Service (CATS). [online]. [Viewed April 10, 2018]. Available from: http://www.nhstayside.scot.nhs.uk/OurServicesA-Z/ContinenceAdvisoryandTreatmentService/index.htm
- ↑ Moore, K.L., Dalley, A.F. and Agur, A.M., 2013. Clinically oriented anatomy. Lippincott Williams & Wilkins.
- ↑ Palastanga, N. and Soames, R., 2011. Anatomy and human movement, structure and function. Elsevier Health Sciences.
- ↑ Drake, R., Vogl, A.W. and Mitchell, A.W., 2009. Gray's Anatomy for Students E-Book. Elsevier Health Sciences.
- ↑ 70.0 70.1 Hendrix, S.L., Clark, A., Nygaard, I., Aragaki, A., Barnabei, V. and McTiernan, A., 2002. Pelvic organ prolapse in the Women's Health Initiative: gravity and gravidity. American Journal of Obstetrics & Gynecology. Vol. 186, no. 6, pp.1160-1166.
- ↑ MAYO CLINIC., 2014. Anterior Prolapse (Cystocele) [online] [viewed 9 April 2018]. Available from: https://www.mayoclinic.org/diseases-conditions/cystocele/symptoms-causes/syc-20369452
- ↑ Polden, M. and Mantle, J., 1990. Physiotherapy in obstetrics and gynaecology. Elsevier Health Sciences.
- ↑ Jelovsek, J.E., Maher, C. and Barber, M.D., 2007. Pelvic organ prolapse. The Lancet. Vol. 369, no. 9566, pp.1027-1038.
- ↑ THE URETHRA CLINIC., 2017. Controversies in Management of Pelvic Fracture Urethral Injuries [online] [viewed 9 April 2018]. Available from:[/www.theurethraclinic.com/blog/controversies-management-pelvic-fracture-urethral-injuries/ https://www.theurethraclinic.com/blog/controversies-management-pelvic-fracture-urethral-injuries/]
- ↑ Weber, A.M. and Richter, H.E., 2005. Pelvic organ prolapse. Obstetrics & Gynecology. Vol. 106, no. 3, pp.615-634.
- ↑ MAYO CLINIC., 2017. Small Bowel Prolapse (Enterocele) [online] [viewed 9 April 2018] . Available from: https://www.mayoclinic.org/diseases-conditions/enterocele/symptoms-causes/syc-20377661
- ↑ MAYO CLINIC., 2017. Small Bowel Prolapse (Enterocele) [online] [viewed 9 April 2018] . Available from: https://www.mayoclinic.org/diseases-conditions/enterocele/symptoms-causes/syc-20377661
- ↑ Kuncharapu, I., Majeroni, B.A. and Johnson, D.W., 2010. Pelvic organ prolapse. Am Fam Physician. Vol. 81, no. 9, pp.1111-1117.
- ↑ MAYO CLINIC., 2017. Small Bowel Prolapse (Enterocele) [online] [viewed 9 April 2018] . Available from: https://www.mayoclinic.org/diseases-conditions/enterocele/symptoms-causes/syc-20377661
- ↑ MACFARLANE, K., 2018. Due Diligence and Keeping Lone Workers Safe [online]. [viewed 04 April 2018]. Available from: https://safetylineloneworker.com/blog/due-diligence-and-keeping-lone-workers-safe-2/
- ↑ BERGHMANS, B., NIEMAN, F., LEUE, C., WEEMHOFF, M., BREUKINK, S. and VAN KOEVERINGE, G., 2016. Prevalence and triage of first contact pelvic floor dysfunction complaints in male patients referred to a Pelvic Care Centre. Neurourology and urodynamics. April,vol.35, no.4, pp.487-491.
- ↑ KIRBY, A.C., LUBER, K.M. and MENEFEE, S.A., 2013. An update on the current and future demand for care of pelvic floor disorders in the United States. American Journal of Obstetrics & Gynecology. August, vol.209, no.6, pp.584-e1.
- ↑ NHS TRUST., 2014. National Health Service [online]. [viewed 19th March 2018]. Available from: http://www.ouh.nhs.uk/patient-guide/leaflets/files/11124Ppelvic.pdf
- ↑ CSP., 2014. Chartered Society of Physiotherapy [online]. [viewed 19 March 2018]. Available from: www.csp.org.uk/sites/files/csp/secure/pogp-pelvicfloor-male.pdf
- ↑ GLINA, S., 2011. Erectile dysfunction after radical prostatectomy. Drugs & aging. April, vol.28, no.4, pp.257-266.
- ↑ FROTA, I.P.R., ROCHA, A.B.O., NETO, J.A.V., VASCONCELOS, C.T.M., DE MAGALHAES, T.F., KARBAGE, S.A.L., AUGUSTO, K.L., NASCIMENTO, S.L.D., HADDAD, J.M. and BEZERRA, L.R.P.S., 2018. Pelvic floor muscle function and quality of life in postmenopausal women with and without pelvic floor dysfunction. Acta obstetricia et gynecologica Scandinavica.
- ↑ CAMPEAU, L., GORBACHINSKY, I., BADLANI, G.H. and Andersson, K.E., 2011. Pelvic floor disorders: linking genetic risk factors to biochemical changes. BJU international, October, vol.108, no.8, pp.1240-1247.
- ↑ HARTIGAN, S.M. and SMITH, A.L., 2018. Disparities in Female Pelvic Floor Disorders. Current urology reports. February, vol.19, no.2, p.16-22.
- ↑ JAMSHED, N., LEE, Z.E. and OLDEN, K.W., 2011. Diagnostic approach to chronic constipation in adults. American family physician. August, vol. 84, no.3, p.299-306.
- ↑ CONTINENCE FOUNDATION AUSTRALIA 2016. [online] [viewed 17 March 2018]. Available from: http://www.pelvicfloorfirst.org.au/pages/are-you-at-risk.html.
- ↑ RAMALINGAM, K. and MONGA, A., 2015. Obesity and pelvic floor dysfunction. Best practice & research Clinical obstetrics & gynaecology. May, vol.29, no.4, pp.541-547.
- ↑ 92.0 92.1 92.2 DUMOULIN, C., HUNTER, K.F., MOORE, K., BRADLEY, C.S., BURGIO, K.L., HAGEN, S., IMAMURA, M., THAKAR, R., WILLIAMS, K. and CHAMBERS, T., 2016. Conservative management for female urinary incontinence and pelvic organ prolapse review 2013: Summary of the 5th International Consultation on Incontinence. Neurourology and Urodynamics. vol. 35, no. 1, pp. 15-20.
- ↑ 93.0 93.1 93.2 93.3 MILSOM, I., COYNE, K.S., NICHOLSON, S., KVASZ, M., CHEN, C.I. and WEIN, A.J., 2014. Global prevalence and economic burden of urgency urinary incontinence: a systematic review. European Urology. Jan, vol. 65, no. 1, pp. 79-95.
- ↑ 94.0 94.1 94.2 HAGEN, S., STARK, D., GLAZENER, C., DICKSON, S., BARRY, S., ELDERS, A., FRAWLEY, H., GALEA, M.P., LOGAN, J. and MCDONALD, A., 2014. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. The Lancet. vol. 383, no. 9919, pp. 796-806.
- ↑ DWYER, L. and KEARNEY, R., 2017. Conservative management of pelvic organ prolapse. Obstetrics, Gynaecology & Reproductive Medicine.
- ↑ GUROVICH, M., FAGERSTROM, C., PRIETO, M. and SANCHEZ, H., 2016. Recommendations for Caffeine Intake Reduction in Women with Urinary Incontinence: A Systematic Review of Literature. Int J Womens Health Wellness. vol. 2, pp. 035.
- ↑ GLEASON, J.L., RICHTER, H.E., REDDEN, D.T., GOODE, P.S., BURGIO, K.L. and MARKLAND, A.D., 2013. Caffeine and urinary incontinence in US women. International Urogynecology Journal. vol. 24, no. 2, pp. 295-302.
- ↑ 98.0 98.1 98.2 NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE., 2015. Urinary incontinence in women: management [online] [viewed 12 April 2018]. Available from: https://www.nice.org.uk/guidance/cg171
- ↑ DUMOULIN, C., HAY‐SMITH, J., HABÉE‐SÉGUIN, G.M. and MERCIER, J., 2015. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: A short version Cochrane systematic review with meta‐analysis. Neurourology and Urodynamics. vol. 34, no. 4, pp. 300-308.
- ↑ LI, C., GONG, Y. and WANG, B., 2016. The efficacy of pelvic floor muscle training for pelvic organ prolapse: a systematic review and meta-analysis. International Urogynecology Journal. vol. 27, no. 7, pp. 981-992.
- ↑ FERREIRA, C.H.J., DWYER, P.L., DAVIDSON, M., DE SOUZA, A., UGARTE, J.A. and FRAWLEY, H.C., 2015. Does pelvic floor muscle training improve female sexual function? A systematic review. International Urogynecology Journal. vol. 26, no. 12, pp. 1735-1750.
- ↑ 102.0 102.1 ALVES, F.K., RICCETTO, C., ADAMI, D.B., MARQUES, J., PEREIRA, L.C., PALMA, P. and BOTELHO, S., 2015. A pelvic floor muscle training program in postmenopausal women: A randomized controlled trial. Maturitas. Jun, vol. 81, no. 2, pp. 300-305.
- ↑ DUMOULIN, C., ALEWIJNSE, D., BO, K., HAGEN, S., STARK, D., VAN KAMPEN, M., HERBERT, J., HAY‐SMITH, J., FRAWLEY, H. and MCCLURG, D., 2015. Pelvic‐Floor‐Muscle Training Adherence: Tools, Measurements and Strategies—2011 ICS State‐of‐the‐Science Seminar Research Paper II of IV. Neurourology and Urodynamics. vol. 34, no. 7, pp. 615-621.
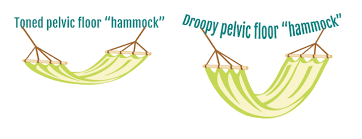
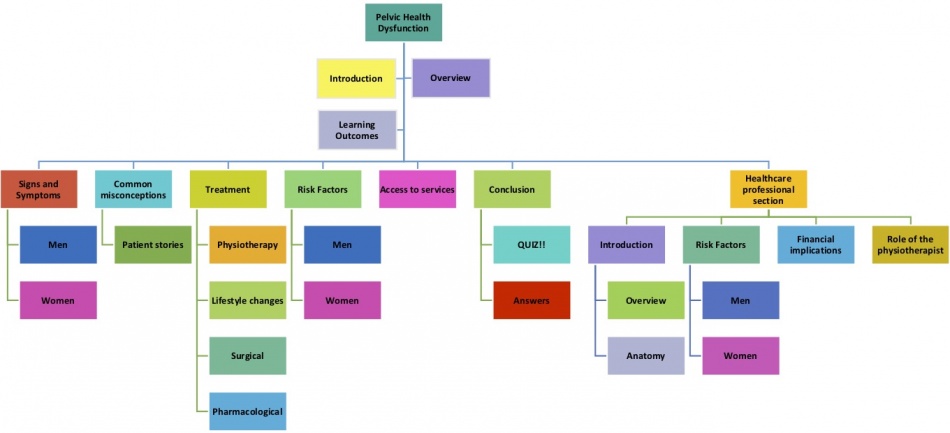
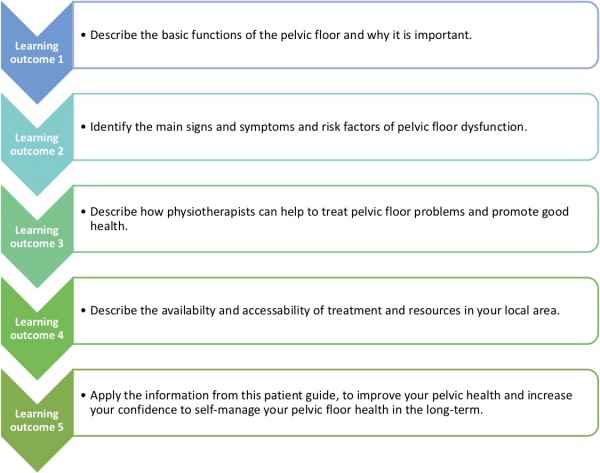
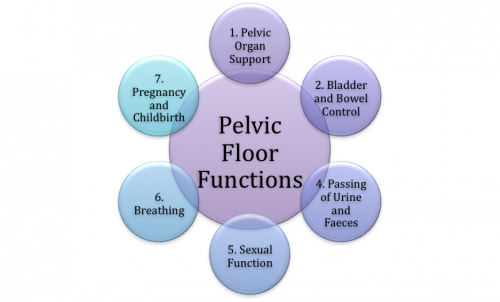

![[29]](/images/thumb/1/13/Pregnancy_as_a_risk_factor_for_women.gif/300px-Pregnancy_as_a_risk_factor_for_women.gif)
![[44]](/images/thumb/b/b7/Heavy_lifting-risk_factors.gif/300px-Heavy_lifting-risk_factors.gif)