Pelvic Floor Dysfunction: Difference between revisions
No edit summary |
No edit summary |
||
| Line 368: | Line 368: | ||
* Third degree- the entire uterus descends outside the introitus of the body, causing total inversion of the vagina. <ref name=":12" /> | * Third degree- the entire uterus descends outside the introitus of the body, causing total inversion of the vagina. <ref name=":12" /> | ||
Rectocele prolapse occurs when the bowel and rectum bulge forwards against the lower part of the posterior wall of the vagina. Inadequate or ineffective suturing of episiotomies and perineal tear post childbirth. Constipation. Perineal splinting for bowel movement.<ref>Kuncharapu, I., Majeroni, B.A. and Johnson, D.W., 2010. Pelvic organ prolapse. ''Am Fam Physician''. Vol. 81, no. 9, pp.1111-1117.</ref> | Rectocele prolapse occurs when the bowel and rectum bulge forwards against the lower part of the posterior wall of the vagina. Inadequate or ineffective suturing of episiotomies and perineal tear post childbirth. Constipation. Perineal splinting for bowel movement.<ref>Kuncharapu, I., Majeroni, B.A. and Johnson, D.W., 2010. Pelvic organ prolapse. ''Am Fam Physician''. Vol. 81, no. 9, pp.1111-1117.</ref> | ||
Here is a video showing a summary of the pelvic floor anatomy and types of prolapses that can occur: | |||
{{#ev:youtube|v=aXGlt-HDrJU}} | |||
[[File:Risks.jpg|right|frameless|377x377px|<ref>MACFARLANE, K., 2018. Due Diligence and Keeping Lone Workers Safe [online]. [viewed 04 April 2018]. Available from: <nowiki>https://safetylineloneworker.com/blog/due-diligence-and-keeping-lone-workers-safe-2/</nowiki> </ref>]] | [[File:Risks.jpg|right|frameless|377x377px|<ref>MACFARLANE, K., 2018. Due Diligence and Keeping Lone Workers Safe [online]. [viewed 04 April 2018]. Available from: <nowiki>https://safetylineloneworker.com/blog/due-diligence-and-keeping-lone-workers-safe-2/</nowiki> </ref>]] | ||
Revision as of 20:15, 9 April 2018
Original Editors - Sarah Barnes, Chris Van Wyk, Amy McCarthy, Gina McLoughlin, John Lavin, Claire Ramsden and Carolinne Cieslak.
Top Contributors - Sarah Barnes, Carolinne Cieslak, Gina McLoughlin, Kim Jackson, Claire Ramsden, Chris Van Wyk, Amy McCarthy, John Lavin, Vidya Acharya, Nicole Hills and Rachael Lowe
Pelvic Floor Dysfunction[edit | edit source]
Below is an overview of this physiopedia page. If you would like to skip to a certain part within the page then use the image below to navigate your way to that information.
Introduction[edit | edit source]
Speaking about your nether-regions is never an easy thing to do! Problems with you pelvic floor (including incontinence, leaking, and pelvic organ prolapse) is no easy subject to bring up, especially when you are worried that there may be something wrong! Pelvic floor dysfunction is heavily underreported[1] as so many people don't feel comfortable speaking up about it.
This physiopedia page has been written to provide the public with some information on pelvic floor health, providing information on what the pelvic floor is, how to exercise it and what can happen if you don't. This patient guide also has information on how to access treatment from local NHS services, for example physiotherapy. This page has been designed to build upon previous resources available and to bring together important and valuable information on pelvic floor health, so it is all within one page for your easy reading.
Yer aff yer heid!! A am' nae talkin' about whats under ma breeks!!![edit | edit source]
Do you feel you are the only person with problems with your undercarriage?. . . .
You are not alone. Many people talking about pelvic health to be a difficult conversation to bring up.
In fact, 41-50% of women over 40 are affected by pelvic organ prolapse (information below)[2]. Only 17% of those with urinary incontinence seek medical help[3]. Pelvic floor dysfunction affects more women than men[4], however, men are affected!!! From these figures, 46% of people suffer with their symptoms for 1 to 5 years[3], 42% of people suffering with their symptoms for 5 years or more[3].
Issues with your netherregions are well known to have negative effects on your quality of life for both men and women [4]. Many individuals have reported negative affects on their home and work activities, personal relationships, social lives and mental wellbeing[1]. Pelvic floor dysfunction is also associated with depression, social isolation, anxiety and generally reduced quality of life[4].
Fear not! We have designed this patient guide to provide you with the information you need to take charge of your undercarriage and be leak free!!
We have designed a quick quiz (at the bottom of the page) for you to test your knowledge after reading through this guide. Have fun!!
Our mission:[edit | edit source]
To increase the public's knowledge and recognition of pelvic floor health, and empower individuals to seek professional help if they believe something to be wrong.
Our vision:[edit | edit source]
All members of the public will understand the implications of reduced pelvic floor health and the overall impact it has on daily activities and quality of life. Our aim, through education, is to empower the public to be proactive and seek advice from healthcare professionals. Through a partnership between the public and healthcare professionals, individuals will possess the correct tools to begin their journey of improving the symptoms of their pelvic floor dysfunction through increasing levels of personal self-management.
In support of our mission, we have designed a healthcare professional section (at the bottom of the page) specifically designed for physiotherapists and members of the public who would like to read further on the subject of pelvic floor health. This section includes academic journals and more detailed information on all aspects of pelvic floor dysfunction in addition to handy treatment advice and helpful ways to teach the pelvic floor exercises to patients.
Learning Outcomes[edit | edit source]
After exploring this wiki page, the reader should be able to:
Any problems with your water works?[edit | edit source]
Still feel the topic of pelvic floor health is a little awkward and uncomfortable? Not to worry here is Elaine Miller (a pelvic health physiotherapist and stand up comedian) to lighten the mood. This is Elaine's Edinburgh Fringe Festival performance Gusset Grippers. In this show she makes personal topics a more humorous topic.
Click here If you would like to know more about Elaine or her gigs.
Overview[edit | edit source]
What is the Pelvic Floor?[edit | edit source]
The pelvic floor is made up of a layer of muscles spanning the bottom of the pelvis that support the bladder and bowel in males [5] and bladder, bowel and womb in women. These structures that sit on top of the pelvic floor are known as our pelvic organs. The muscles run like a hammock from the front of the pelvis to the tailbone (coccyx) at the back, and side-to-side from one sitting bone to the other [6] as can be seen in the picture below.
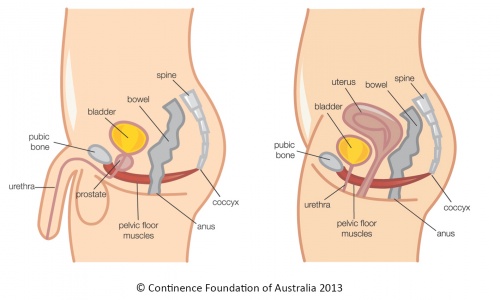
The pelvic floor muscles also have holes through which the urethra (tube through which urine (wee) exits our body from the bladder) and anus (exit at the end of our digestive system through which faeces (poo) pass) pass through in males and urethra, anus and vagina pass through in females[6]. The muscles are snug against these structures in order to hold the passages closed. Both the anus and urethra have extra circular muscles (called sphincters) that help to keep the passages closed and prevent any unwanted leaking or skid marks.[8]
Our pelvic floor muscles are similar to a trampoline, as they have the ability to move up and down. This occurs during breathing and is much easier to imagine if we consider our body as a cylinder. When we breath in our diaphragm (breathing muscle) pulls down to open our lungs[9], this is like the top of the cylinder pulling down. This pushes down of our internal organs and in order to avoid squashing these organs our pelvic floor and abdominal muscle relax are stretched down and out. This is like the bottom and sides of the cylinder stretching down and out to create more space for the organs. When we exhale like the top of the cylinder (the diaphragm) springs back to its normal position. As it does so the abdominals and pelvic floor muscles return to their normal positions also. A common problem experienced by people, is holding their breath during lifting activities or bowel movements. This can lead to pelvic floor weakness or dysfunctions by adding excess stress on these muscles.[10]
Click here to see a visual diagram of the diaphragm and pelvic floor muscles working together.
Pelvic floor muscles may be hidden but we do have the ability to control and train them just like the muscles in our arms or legs.
Functions of the Pelvic Floor Muscles:[edit | edit source]
The pelvic floor serves many important functions from being a basket to hold our organs to stopping us from pishing our pants to improving our sexual experience. The picture and paragraph below run through some of the main functions of our pelvic floor in more detail.
- Support internal pelvic organs in the correct positions (Bladder, bowel and womb).[5][11]
- Allow purposeful control of bladder and bowel habits using the sphincter muscles. This allows us to control the release of urine (wee), faeces (poo) and gas. This allows us to delay emptying until a convenient time when a toilet is available. This works bt the pelvic floor muscles tightening it lifts the pelvic organs up and the sphincter then tightens around the openings of the urethra and anus.[5][11]
- Allow the passage of urine and faeces out of the body due to the pelvic floor muscles relaxing and allowing the passages to open.[5][10]
- Sexual function[5]
- As mentioned above the pelvic floor muscles play a role in breathing by relaxing and increasing the space the lungs have to expand.[10]
- Additionally in pregnant women the pelvic floor offers support to the baby during pregnancy and also assists in the childbirth process.[5]
Strong pelvic floor muscles are important when we cough, laugh, sneeze or during lifting activities as there is extra force added to the abdomen and pelvic floor[10]. If these muscles are weak, stretched or not working as they should, pelvic floor dysfunction may occur and lead to signs and symptoms mentioned below. Some of these symptoms may be pressure felt in the pelvic region and/or bladder or bowel leaking occurring during laughing, coughing, sneezing or lifting.[13]
Urinary dysfunction, erectile dysfunction, premature ejaculation, painful ejaculation and chronic pelvic pain are some conditions that can be linked with weak pelvic floor muscles. Erectile function requires contraction of the pelvic floor muscles to block blood from leaving the penis. When the muscles are weak the outflow of blood from the penis is not stopped resulting in erectile dysfunction. Through learning voluntary control of the pelvic floor muscles this can help prevent premature ejaculation by learning how to relax and contract the muscles.[14] Urinary incontinence has a direct relationship with pelvic floor muscles. These muscles tighten as a closure mechanism for the tube from the bladder to the exit (urethra) and weakness of these muscle can cause leaking and dribbling.[15]
Prolapse is a common condition that can occur due to weak pelvic floor muscles in women. This occurs due to the womb, bladder, bowel or top of the vagina moving out of their normal positions and pushing into the vagina.This can cause pain and discomfort but can be improved with pelvic floor exercises and lifestyle changes which are mentioned in the treatment section of this wiki[16].
Signs and Symptoms of Pelvic Floor Dysfunction[edit | edit source]
There are a few well known signs and symptoms that people experience when they have a problem with their pelvic floor muscles. Many individuals have described some of these problems and feelings as normal, as they have been happening for so long. However, this shouldn't be the case!!
The following list of signs and symptoms are common for people with weak pelvic floor muscles.
If you are unsure whether you have a pelvic floor dysfunction or would like further information on each sign and symptom, the following website is extremely useful!! Women's and men's health physiotherapy.
Men:[edit | edit source]
- Constipation or bowel strains[17]
- Ongoing pain in your pelvic region, genitals or rectum.[18][19]
- A prolapse – may feel as though there is a bulge/ pressure in the rectum or a feeling of needing to use your bowels without actually needing to go. - Accidentally leaking urine when you exercise, laugh, cough or sneeze.[20][21][19]
- Feelings of urgency in needing to the bathroom, or not making it there in time.[20][21][22]
- Frequent need to urinate.[22]
- Difficultly emptying your bladder (discontinuous urination – stop and start multiple times) and bowels.[22]
- The feeling of needing to have several bowel movements during a short period of time.
- Accidentally passing wind.[20]
- Pain in your lower back that cannot be explained by other causes.[20]
- Pain in the testicles, penis (referred pain from the pelvic floor) or pelvis during intercourse.[18]
- Erectile dysfunction.[18][21][19]
- Painful ejaculation.[18][21][19]
- Premature ejaculation. [18][21]
For further information on the male pelvic floor go to: Pelvic floor advice for men - download the advice leaflet. OR. Male pelvic floor.
Women:[edit | edit source]
- Pain or numbness during intercourse.[20][17][19]
- Ongoing pain in your pelvic region, genitals or rectum.
- A prolapse – may be felt as a bulge in the vagina (feeling or seeing a bulge or lump in or coming out of your vagina) or a feeling of heaviness, discomfort, pulling, dragging or dropping sensation.[20]
- Accidentally leaking urine when you exercise, laugh, cough or sneeze (stress incontinence).[19][22]
- Feelings of urgency in needing to the bathroom, or not making it there in time.[22]
- Frequent need to urinate.[20][22]
- Difficultly emptying your bladder (discontinuous urination – stop and start multiple times) and bowels.[20][22]
- The feeling of needing to have several bowel movements during a short period of time.
- Constipation or bowel strains.[17]
- Accidentally passing wind.[20]
- Pain in your lower back that cannot be explained by other causes.[20]
Helpful websites for further information on the signs and symptoms of pelvic floor dysfunction: Health line or Pelvic floor first.
For further support for urinary or faecal incontinence you can visit the following NHS site: Living with incontinence.
Common Misconceptions[edit | edit source]
[1]- A patient personal experience of pelvic floor dysfunction, This is an interesting, personal and relatable video that explains pelvic floor dysfunction in real life terms .
It’s my fault isn’t it?[23][edit | edit source]
Being a female in the 21st century is certainly not an easy task. The role of a woman is diverse, demanding and challenging. Woman chop and change from being a mother, a lover, a homemaker to a successful business woman managing the hiring and firing in some of the worlds most successful and glamorous companies . Woman are athletes, breaking records for the highest jump in the Olympic games and setting new personal bests that challenges not only them but every other female on this planet to beat. Woman are the backbone of the fashion industry, selling our souls for the latest Louis Vuitton autumn spring collection which of course consists of utterly divine leather pants! The overall picture is, WOMAN ARE BUSY! ...
Woman who experience symptoms associated with Pelvic organ dysfunction such as incontinence, leaking, increase urgency and prolapse blame themselves[24]. Some woman feel "deserving" of these symptoms, due to lack of consistency or failure to prioritise their pelvic floor muscle training post childbirth or throughout the ageing process due to commitments in other roles[24]. Now, lets talk about the shame that comes with this! Shame, that awful uncomfortable, just brush it under the carpet word that woman associate with symptoms as mentioned above. Shame prevents reporting of such symptoms to healthcare professionals, not only due to the uncomfortable nature of the topic but interestingly, woman fear they will be judged or reprimanded for failure to train pelvic floor muscles as expected over the years[23]. Eye opening, right? Some woman feel that leaking, incontinence and even prolapse are "part of the parcel" of being a woman, and these are side effects that come with the job [24]. Some woman accept this faith and resign to a life of incontinence wear and multiple red cheeked situations. A pelvic floor contraction.... Queue the tumbleweed! One of the more difficult things in life to explain, we can all agree with that! Some woman have highlighted the difficulty communicating with healthcare professionals about how to actually do a pelvic floor contraction. Resulting in poor or incorrect technique and never truly exercising the pelvic floor muscles. . .
The silent private exercise:[25][edit | edit source]
Many things in life can be described as mysterious, for example, the Loch ness monster, the misplacement of socks post laundry day, that diminishing tub of ice-cream in the freezer when you swear you only had one bite. But, the biggest mystery of all, the nature of a pelvic floor contraction.
Finding the appropriate yet explicit language to explain a pelvic floor contraction is not an easy task. Exercising muscles that cannot be seen, are located in a private area of the body and associated with private function are not easily discussed. Hence, the mystery that surrounds pelvic floor muscle training. A study was conducted to evaluate healthcare professionals skills at explaining pelvic floor muscle contraction to patients. One patient involved in this study, described the explanation given as "sketchy and confusing [25]". Difficulty grasping this technique has been a cause of embarrassment for woman and many feel silly as they struggle to get their head around engaging the pelvic floor muscles correctly! In an attempt to contract the pelvic floor muscle, some common errors are made. Contraction of other muscles such as the rectus abdominus (tummy muscle ) glutes and adductors (The muscle the Kardashians have made famous!) instead of the true internal pelvic floor muscles. Also, compensatory movements such as pelvic tilts, breath holding and straining can give the illusion of a pelvic floor contraction. In fact, this study found that 57% of woman adopt some form of compensatory movement when attempting to contract the pelvic floor[24]. Frustrating, right?
Will pelvic floor muscle training work?[25] [24][edit | edit source]
Hell yeah it works!!
Want a bigger bicep? Simple, operation bicep curl and problem solved! Dreams of that Kardashian derriere? 50 squats a day and I am as good as Kim K right ? Want a stronger pelvic floor? Hell yes! See ya later incontinence !... yeah.. hmm.. okay, perhaps that is not as attractive the other examples granted. Some woman really struggle to commit to pelvic floor exercises due to the absence of noticeable benefit. No immediate or visible effect from training leads woman to feel as though there is no return for their efforts and some woman feel that pelvic floor muscle training is a waste of time[25]. And okay, granted, the nature of pelvic floor exercises is not going to set everyone's world on fire. Give me Aqua-aerobics and some Bonnie Tyler any day! Some woman find pelvic floor exercises tedious, a daily battle and downright boring. The nature of the pelvic floor contraction involves a lot of thinking about ones "private " area. And exercising that "private "area needs concentration, peace and quiet. Many woman feel uncomfortable and simply unable to exercise the pelvic floor around others[25]. Allocating time specifically to this and finding a quite place without distraction is not always easy. As a result, some woman have great difficulty factoring pelvic floor exercises into their daily routine.
Prolapse, incontinence and leaking, that's a female problem right?[26][edit | edit source]
Men are from Venus and woman are from Mars. In some respects yes! But, when it comes to the pelvic floor muscle, we all originate from the same planet! Meaning, regardless of gender pelvic floor muscle training is essential for both men and woman. Prolapse, incontinence and leakage are widely believed to be a female issue. As woman give birth and go through the process of labor, and are subject to hormonal changes throughout the ageing process, it is understandable why some men believe they can dodge the pelvic floor bullet! Unfortunately guys, that bullet is coming straight for you! Males are not exempt from pelvic floor muscle training, as the same risks apply. Studies conducted found that nearly 66% of men are unaware that males are required to do pelvic floor muscle training[26]. But please, don't panic guys, we are here to help! There is a general under reporting of symptoms within the male population when it comes to the tell tale signs that all is not well in the land of the pelvic floor, stigma, embarrassment and the discomfort associated with discussing this issue prevents a lot of males from reporting these symptoms. In general, the body of evidence in this area lies within the female population, there is a lack of research investigating the male experience of pelvic floor muscle training.
Are you at risk?[edit | edit source]
The following risk factors (modifiable: usually lifestyle related such as smoking, and non-modifiable, such as age/genetics), may contribute to the growing population with pelvic floor dysfunction.The predispositions for pelvic organ prolapse, urinary (pee)/fecal (poo) incontinence, erectile dysfunction (all part of pelvic floor dysfunction), include several factors. A combination of changes in anatomy/physiology, genetics, and lifestyle, play a role in the presentation of pelvic floor conditions.
The common risk factors for both males and females have been illustrated in the diagram below in yellow circles. Predispositions unique to each gender include blue circles for males and pink for females.
Men:[edit | edit source]
- Prostate surgery: Specific pelvic floor disorders include urinary (pee) incontinence and erectile dysfunction, which are quite common post-operatively in up to 89% of men[27]. Frequently, after the procedure, these conditions present as having poor bladder control, weakness in pelvic floor muscles (especially urinary sphincters) and changed pelvic nerve supply [28].
Women:[edit | edit source]
- Age: Menopausal age (48-55) increases risk for developing pelvic organ prolapse by 21.1% [30][31]
- Direct injury to pelvic floor muscles controlling urination and loss of pelvic floor muscle tension: The injury to this muscle from vaginal delivery or direct fall onto groin, often forces other anatomical structures called ligaments, to compensate by giving more support than normal to the affected pelvic floor muscles. However, ligaments and muscles have a different biological design and serve a unique purpose in the body mechanics. By changing their normal functioning, over time, the pelvic floor structures lose their strength, resulting in the occurrence of pelvic organ prolapse [32].
- Pregnancy and the nature of childbirth: Vaginal birth, prolonged labour, instrumental delivery (use of spoon-like tools to help baby out of birth canal), episiotomy (surgical procedure to increase opening in vagina), parity (weight and number of children) have also been known to increase the pelvic floor dysfunction risk by 4-16% [30][32][33].
- Genetics and family history: Women who have a family history of pelvic organ prolapse, are more likely to have the condition[34].In females who are experiencing urinary (pee)incontinence, the connective tissue (supports pelvic floor) may be genetically weak[35] [36].
- Hysterectomy (surgical removal of womb): This procedure often damages and weakens the pelvic muscles. Therefore, it is known to increase chances of being more predisposed to pelvic organ prolapse[31] [37]. The risk also increases to 60% for developing urinary incontinence after hysterectomy among middle-aged women [38].
Both Genders:[edit | edit source]
- Previous injury to pelvic region (e.g. fall or pelvic radiotherapy): A fall causing injury to the pelvic structures, including those responsible for urination or reproduction can present as pelvic floor dysfunction. Side effects of pelvic radiotherapy involve weakening of pelvic floor muscles in both men and women. In men, radiation for prostate cancer influences erectile dysfunction, and urinary incontinence[39]. For women, pelvic radiation may also lead to urinary (pee) incontinence [40].
- Increased abdominal pressure: Frequent coughing (symptom of chronic lung disease, smoking, hay fever) and persistent sneezing cause overusing pelvic floor muscles. This weakens pelvic floor structures and can lead to release of urine (pee) without control [41].It is often presented as pelvic organ prolapse in women and urinary (pee) incontinence in men[32][42].
- Constipation/heavy lifting: Constipation is caused by changes in pelvic floor muscles and increase in abdominal pressure during bowel movement. These persistent conditions can damage nerves and appear as pelvic floor dysfunction symptoms, such as fecal (poo) incontinence[44]. Occupations that require frequent heavy lifting, add pressure to the bladder and influence urinary(pee) incontinence in both genders[45]. Women who perform prolonged heavy lifting, are 9.6 times more at risk of developing pelvic organ prolapse[36].
- Intense physical effort: Elite athletes, engaging in high impact sports (e.g. trampolining, running, gymnastics) compared to low impact sports (e.g. golf), tend to experience increase in abdominal pressure, which over time, often leads to urinary (pee) incontinence[36][35].
- Obesity: Being overweight, may be associated with urinary (pee) incontinence in both genders and pelvic organ prolapse in women, compared to those with healthy weight[30][35][39]. Simple modifications such as healthy diet or increase in physical activity may be prescribed to reduce the risk for these conditions.
- History of back pain: Low back pain might be related to pelvic floor muscle dysfunction. This is because the pelvic muscles have a role of providing stability for the lower back and bladder control continence. As a result, the discomfort can prevent normal movement, including the use of pelvic floor muscles. Consequently, they become weaker, unable to support the pelvic floor organs changing urinary (peeing) function[46].
For more information, you can refer to the links provided below:
For males and females
Common problems with pelvic floor muscles [48]
Treatment [edit | edit source]
Pelvic floor dysfunction is a very treatable condition. Many ways exist to treat pelvic floor problems conservatively and should generally be considered as the first-line option prior to more aggressive procedures such as surgery[49][50][51]. Treatment will vary according to the nature of the condition or reason behind the dysfunction. A health care practitioner, such as your GP or a physiotherapist, will help you decide which one is best for you:
Conservative:[edit | edit source]
Physiotherapy & Exercise:[edit | edit source]
- Pelvic floor muscle training is a very important part of improving pelvic floor dysfunction and is valuable to both men and women[52]. Pelvic floor exercise aims to increase the strength, endurance and co-ordination of the muscles, which improves their overall function[51]. Weak or damaged PF muscles can’t do their job properly and this can contribute to many problems such as incontinence and organ prolapse. A strong pelvic floor will help to prevent incontinence, provide support to pelvic organs and even improve your sex life![53]
- There are many different methods to do exercise your pelvic floor muscles, a physiotherapist or GP that specializes in pelvic health is best suited to teach you how to do these essential exercises. Some specialists may use other techniques as well to help treatment[53]. Please see the links below for some helpful information.
- The NHS has also developed a very handy app to help provide information, additional resources and even reminders about doing pelvic floor exercises! Please visit their site for more information: The Squeezy app
- To exercise your pelvic floor, it's handy to think of 'lifting and squeezing' as if you're trying to stop your wee or stop from passing gas! Please see the links below for more information on pelvic floor muscle training.
Female information leaflet from the British Association of Urological Surgeons
Male information leaflet from the British Association of Urological Surgeons
Below are links for progressive pelvic floor exercises that you can try at home!:
| [54] | [55] | [56] | [57] | [58] |
Additional videos for you to try:
Youtube video: Pelvic floor exercises for men
Youtube video: Pelvic floor exercises for beginners
Lifestyle Changes:[edit | edit source]
- These may be suggested by the GP to help improve certain aspects of your condition. For example, quitting smoking, increasing your physical activity and improving your diet to achieve a healthier weight are all great strategies to improve your symptoms and overall quality of life as there will be less stress on your pelvic floor. [49]
- Another helpful tip is to try and reduce alcoholic drinks or those with caffeine as it can irritate the bladder (coffee, tea, cola etc.), while also trying to get enough water intake throughout the day to stay hydrated. [59]
- Certain strategies may be used in every-day situations as well. For example, tightening up your pelvic floor muscles prior to lifting heavy loads, or when possible, sharing the load with another person to lighten it and reduce the strain. This will help to prevent any unwanted leakage or damage.[52]
Pharmacological:[edit | edit source]
- Various drugs can be prescribed if based on the reason for pelvic floor problems, and your GP will decide with you if these are necessary. Drug therapy is particularly common for urinary incontinence and depending on the type of incontinence you’re experiencing, different medications are available[51].
- For example, if you have a stress incontinence, there are drugs to that help reduce leakage and hormone replacement therapies for post-menopausal women. If you have an over-active bladder or urge incontinence, there are medications to help relax the bladder and reduce the frequency of urination.[60]
- Drug therapy is even more effective when used in combination with other strategies like pelvic floor exercises and lifestyle changes.[60]
For more information, please see this NHS website.
Surgical:[edit | edit source]
- In some cases, when other strategies have been unsuccessful in achieving your treatment goals, surgery may be a treatment option for you. Depending on your specific condition, various procedures exist to address the problem.
- For example, urge and stress incontinence have multiple types of procedures to alter the pelvic structures or insert supports such as mesh slings, both in the goal of improving functions.[61]
- Slightly less invasive options are also available, such as injections of Botox for urge incontinence or bulking agents to help reduce stress incontinence.[62]
For more information on bladder procedures, please visit this site.
For more information on urinary incontinence procedures, please visit this NHS website.
Surgery implications:FIT THESE INTO SENTENCES>
- For those who have a pelvic floor disorder, 1 in 9 will undergo surgery.
- Prolapse surgery is often prone to failure[2].
- 30% require repeat operations[2].
- Synthetic mesh is a common surgical method[2].
- However, there are often complications and there is a 35% removal rate[2].
Access to services[edit | edit source]
Each NHS Boards across Scotland has different process and guidelines to get referred to a Pelvic health/women’s health physiotherapist. Below outline this process in different areas to help direct each patient to the right area.
NHS Forth Valley:[edit | edit source]
For Women’s health you are able to self refer through the following link - Self referral form
If you are having continence problems during and after pregnancy or pelvic floor dysfunction- NHS forth valley ask you to complete the screening tool ICIQ Form (Link below), this will help you decide if you need to refer for a 1:1 assessment with a specialist physiotherapist. If you score more than 10 when you add the totals for questions number 3,4 and 5 we would suggest print, read and complete the self Pelvic Bladder Self Referral Form (link below) and send to the physiotherapy department at either Forth Valley Royal Hospital or Stirling Community Hospital.
Pelvic Bladder self referral form
Alternately, your GP or midwife can also refer you to the services.
NHS Lothian:[edit | edit source]
Treatment for continence symptoms is offered in several departments within Edinburgh Community Physiotherapy Service. Currently the departments offering this service are:[edit | edit source]
- Craigroyston Health Clinic
- Leith Community Treatment Centre
- Slateford Medical Practice
- South Queensferry Health Centre
- Tollcross Health Centre
Conditions which can be helped include:[edit | edit source]
- Stress urinary incontinence (leakage on coughing, sneezing, laughing etc)
- Urgency, frequency and nocturia (needing to empty your bladder urgently and often and getting up at least twice overnight to go to the loo)
- Symptoms of mild prolapse (sensation of something coming down)
- Weak pelvic floor after childbirth including any of the above symptoms
- Men with urinary incontinence can be treated at Leith Community Treatment Centre
The service can be accessed by referral from any of the following:[edit | edit source]
- Self referral – by calling nhs 24 on the number 111 or for Bladder Problems use the Self referral form
- A referral from your GP or any Health Care Professional (nurse, midwife etc)
NHS Borders:[edit | edit source]
Bladder, bowel and pelvic floor service role is to promote continence by offering advice, treatment and management options. Delivered by a skilled team comprising of:
- Principal Physiotherapist Bladder, Bowel and Pelvic Floor Service - Lead Clinician Bladder, Bowel and Pelvic Floor Service
- Specialist Physiotherapist Bladder, Bowel and Pelvic Floor Service
- Bladder, Bowel and Pelvic Floor Service Nurse
The service can be contacted in the following ways:-[edit | edit source]
- A referral from your GP
- A referral from any healthcare professional.
- Self referral - you can refer yourself by telephoning 01896 824555 and leaving your details on the confidential answer phone.
NHS Highland:[edit | edit source]
Service can be accessed by:[edit | edit source]
NHS Highland physiotherapists have re-launching their self referral service for continence and other pelvic health problems. New self referral forms are available from GP practices throughout Highland.
Self referral forms can be returned to the addresses on the form, or handed in to your nearest physiotherapy department. Alternatively you can leave a message for Alison Clarke on 07748761847
Pelvic health Physio self referral form
Not in these areas:[edit | edit source]
If you live outside these areas don’t worry you will still be able to access the help you require, but unfortantly due to limited information available at the time of making this page we suggest making an appointment with your GP to discuss the how to get you the hel you need.
Conclusion:[edit | edit source]
We hope that you enjoyed this physiopedia resource about Pelvic Floor Health and Dysfunction. More importantly, we hope that you learned a lot about your pelvic floor and have a better understanding of the important role it has. If you're someone who is having any issues related to your pelvic floor, we hope this new knowledge will encourage you to speak up and seek help from your healthcare specialist, as well as giving you some helpful tips on self-management so you can take control of your own pelvic floor and life!
A little quiz to hopefully show yourself what you have learnt along the way, so give it a go!
1.Name 3 functions of the pelvic floor?
2.Why is having a strong pelvic floor important?
3.Can you name 3 signs and symptoms for each male and female?
4.Can you name 2 risk factors for pelvic floor dysfunction for males, females and both?
5.What 2 ways a physiotherapist may do to treat pelvic floor dysfunction?
6.Who to can you contact to get referred to pelvic floor physiotherapy?
7.What NHS approved app that was developed to help with your pelvic floor exercises?
8.Can you describe the steps to performing a pelvic floor contraction?
9.Name 2 lifestyle changes you try to aid pelvic floor function?
(Please scroll down for answers...)
Information for healthcare professionals (Physiotherapy specific)[edit | edit source]
Detailed anatomy and overview of the pelvic floor[edit | edit source]
- The pelvic floor is a funnel shaped structure covering the base of the pelvis from the pubic symphysis anteriorly to the coccyx posteriorly and stretches from one ischial tuberosity to the other. It consists of two main muscles, the levator ani and the coccygeus.[63]
- The levator ani muscle is a broad thin muscle that is made up of a group of 3 muscles, pubococcygeus, puborectalis and iliococcygeus. The muscles join in the middle of the pelvis except for at the prostrate in males and vagina and urethra in females.
- Pubococcygeus originates from both sides of the body of the pubis lateral to the puborectalis muscle and anterior to the obturator canal at the tendinous arch. It travels posterior and medial to insert onto the perineum, coccyx and anococcygeal ligament.
- Puborectalis is a U-shaped muscle that originates on both sides on the pubic body just lateral to the pubic symphysis. The muscle runs posterior and encircles the rectum so both side join together. Some fibers join the external anal sphincter. Contraction of this muscle causes the anorectal junction to bend 90 degrees. This maintains faecal continence during contraction and enables defecation on relaxation. Some fibers may extend towards the urethra in both male and females and to the vagina in females, aiding with urinary continence.
- Iliococcygeus originates from the ishial spines and posterior portion of the obturator internus. It travels posterior and medially and inserts onto the anococcygeal ligament and coccyx. [64]
- Coccygeus is also known as the ischiococcygeus muscle. It is a small muscle that makes up the posterior portion of the pelvic floor. It originates from the sacrospinous ligament and ischial spine and inserts on to the lateral borders of inferior sacrum and superior coccyx.[65]
- Urogenital Diaphragm: Deep transverse perineal, Sphincter urethrae
- Sphincters and erectile muscles of the urogenital and intestinal tract: External anal sphincter, Bulbospongiosus, Ischiocavernosus, Superficial transverse perineal
For more information on the anatomy of the pelvic floor please visit: http://teachmeanatomy.info/pelvis/muscles/pelvic-floor/ and [/www.youtube.com/watch%3Fv%3DP3BBAMWm2Eo%26t%3D316s https://www.youtube.com/watch?v=P3BBAMWm2Eo&t=316s]
Types of Prolapse:[edit | edit source]
A prolapse is when a structures has slipped down from its normal position and bulges into the vagina. There are multiple types of prolapse depending on which structures have moved.
Cystocele prolapse is also known as dropped bladder and is the bulging of the bladder into the vagina. It occurs due to the weakening of the pubocervical fascia between the bladder and vaginal wall allowing the bladder to displace downwards and backwards against the anterior wall of the vagina. A pouch may also form in the bladder resulting in retention of residual urine. Symptoms include urinary frequency, incomplete emptying of the bladder, recurrent UTI’s and stress incontinence.[66]

Urethrocoele prolapse is the displacement of the female urethra into the vagina. Due to the urethra being closely attached to the anterior wall of the vagina it can sag backwards and downwards when it receives insufficient support from the vagina or surrounding fascia. This is the least common form of prolapse and is most common in post-menopausal women and pre-pubertal girls.[68]
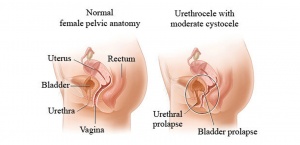
Cystourethrocoele is a combination of a cystocoele and urethrocoele and it is the most common type of prolpase. This is when the the bladder and urethra bulge into the vagina. Symptoms may be associated with urinary stress incontinence, and urinary retention or recurrent urinary tract infections or both.[70]
Enterocoele is when the small bowel pushes down from the abdomen onto the posterior wall of the vagina through the rectovaginal septum and causes a herniateion (Space between rectum and vagina). An enteroceoele usually accompanies a uterine prolapse.[71]
Uterine prolapse occurs when there is a lack of support allowing the uterus and cervix to descend from its normal position towards the vaginal opening and sometimes protrude out of the vagina. This can occur along with a vaginal prolapse where the vaginal vault descends due to weakening in the vaginal walls causing the vagina to invert. This prolapse is associated with a cystocoele and enterocoele prolapses. There is 3 degrees of uterine prolapse:
- First degree- the cervix remains within the vagina
- Second degree – descent if the cervix to the introitus
- Third degree- the entire uterus descends outside the introitus of the body, causing total inversion of the vagina. [66]
Rectocele prolapse occurs when the bowel and rectum bulge forwards against the lower part of the posterior wall of the vagina. Inadequate or ineffective suturing of episiotomies and perineal tear post childbirth. Constipation. Perineal splinting for bowel movement.[72]
Here is a video showing a summary of the pelvic floor anatomy and types of prolapses that can occur:
Risk factors[edit | edit source]
The chances of developing pelvic floor dysfunction among men and women have increased over the past few years. According to Berghmans et al. (2015)[74], this tendency will most likely continue. The incidence rates of individuals experiencing problems with their pelvic floor are predicted to increase by 35% between 2010-2030 [75].
These statistics emphasize the importance of expanding knowledge related to the risk factors for pelvic floor dysfunction. When assessing a patient, physiotherapists should focus on detailed subjective examination including past medical history and presenting condition/complaint, as this may reveal potential predispositions. Goal-centred conversations with the patients can provide guidance in planning a treatment, and where applicable, liaising with appropriate healthcare professionals to ensure a holistic approach to care.
Men[edit | edit source]
- Prostate surgery: In general, scientific literature examining pelvic floor dysfunction among males is limited. However, prostate surgery has been identified as a potential risk factor according to available evidence-based sources [76][77]. Specific pelvic floor disorders include urinary incontinence and erectile dysfunction, which are quite common post-operatively (up to 89% men suffer from these conditions)[27]. Individuals who undergo this procedure, may experience disturbance in pelvic floor muscles (especially urinary sphincters) and altered nerve supply to the area. In prostatectomy, the prostate (partially regulating continence) is removed, increasing probability for incontinence. The urinary sphincter nerves may occasionally be damaged during surgery due to their proximity to the prostate. As a result, the patients might later experience poor bladder control[28]. Cavernous nerves responsible for erectile function, may also be disrupted[78].
Women[edit | edit source]
- Age:Females experiencing menopause, are at increased risk for developing pelvic organ prolapse by 21.1%[30]. Wu et al. (2014)[31] assessed the relationship between age and number of pelvic floor disorders. They revealed that with each decade, the risk dramatically increased. This is most likely due to the hormonal fluctuations which change the functioning of female urogenital structures. It includes weakening of the pelvic floor, as the muscle mass tends to decrease during aging [79].
- Direct injury to levator ani (ex. vaginal delivery, fall on groin) and loss of tone in pelvic muscles: This involves the levator ani changing position and widening of genital hiatus, causing the pelvic structures to rely on the connective tissue for support. Over time, this alteration results in weakening or tearing of the tissue/collagen and may contribute to the occurrence of pelvic organ prolapse [32].
- Pregnancy and the nature of childbirth: Overstretching/damaging of the pudendal nerve during vaginal birth, prolonged labour, instrumental (foreceps) delivery,episiotomy (surgical procedure to increase opening in vagina), weight and number of children (parity) have also been known to increase the Ppelvic floor dysfunction isk by 4-16%[30][32][33]. These findings have been supported tthrough biomechanical models of the pelvic floor. The researchers revealed that during the crowning of fetal head in vaginal birth, there is a greater risk for the avulsion of levator ani leading to a potential prolapse. Additionally, episiotomy has been suggested to increase anal lacerations and therefore, incontinence risk [33]. A set of studies within the systematic review noted parity to be a risk factor for primary Ppelvic organ prolapse s well[30].
- Genetics: Women who have a positive family history of pelvic organ prolapse, are more likely to inherit the condition[34]. Campneau et al. (2011)[80], showed that the risk for pelvic organ prolapse increased 1.4 times in the genetically predisposed group, after controlling for vaginal deliveries, hysterectomy and incontinence. Additionally, evidence shows that in females who are experiencing urinary incontinence, the connective tissue of the pelvic floor muscles may be genetically weak[35][36].
- Low socioeconomic status: This factor, especially among racial minorities, may contribute to poorer access to adequate information regarding pelvic floor dysfunction[31] [32].The lack of resources create a challenge in recognizing the symptoms and importance of seeking professional support in a timely manner. Hartigan and Smith (2018)[81], presented that women of poorer socioeconomic status scored lower on the incontinence quiz than their higher socioeconomic status counterparts. Consequently, there is a strong emphasis on public education to reduce the risk of pelvic floor dysfunction.
- Hysterectomy (surgical removal of uterus): This procedure often damages and weakens the pelvic muscles. Therefore, it is known to increase chances of being more predisposed topelvic organ prolapse [31] [37]. In the study group, the incidence of postoperative complications after hysterectomy, including urinary and fecal incontinence was significantly higher than in the control group[37]. Being middle-aged, as an additional factor to post-hysterectomy, increases the risk to 60% for developing urinary incontinence[38] .
Both genders[edit | edit source]
- Previous trauma to pelvic region (e.g. fall or pelvic radiotherapy): This is particularly common in less physically active men who underwent pelvic radiotherapy for prostate cancer. The side effects of the treatment, including decreased tone of pelvic floor muscles, are more prominent in this group of patients. As a result of the pelvic muscles weakening, men are more susceptible to experience erectile impairment and urinary incontinence symptoms[39]. In women, pelvic radiation, as suggested by Walters (2017)[40] has created an additional risk factor for urinary incontinence and for developing pelvic floor dysfunction symptoms. In order to assure quality of life and avoid many discomforts, men and women should require further screening to receive the optimal treatment.
- Increased abdominal pressure: Chronic coughing (symptom of chronic lung disease, smoking, hay fever) and frequent sneezing, have been shown to contribute to pelvic organ prolapse in women[32]. It has been related to overuse of pelvic floor muscles and ligaments supporting the pelvic organs that occurs as the pressure increases within the abdomen. This weakens the anatomical structures and leads to pelvic organ prolapse [42]. For men, it usually presents as urinary incontinence. The frequent increase in intra-abdominal pressure can lead to opening of the sphincter, despite absence of bladder contraction[40].
- Constipation/heavy lifting: Constipation is caused by the altered mechanics (incoordination) of the pelvic floor muscles and increase in intra-abdominal pressure during attempted evacuation. These persistent conditions can lead to nerve damage and appearance of pelvic floor dysfunction symptoms, such as fecal incontinence[82]. Occupations that require frequent heavy lifting, add pressure to the bladder and influence urinary incontinence in both genders[45]. Evidence also shows that women who perform prolonged heavy lifting, are 9.6 times more at risk of developing pelvic organ prolapse[36].
- Prolonged vigorous physical exertion: Elite athletes, engaging in high impact sports (e.g. trampolining, running, gymnastics) compared to low impact sports (e.g. golf), have reported to experience an increase in abdominal pressure through overstretching/overloading of the pelvic floor muscles. Over time the strain and changes in strength of pelvic floor muscles, have shown to be a potential risk for urinary incontinence[35][36][83]. The implications were also suggested in a study that compared women training competitively on a weekly basis with a non-athletic group. The authors found that athletes were 2.5 times more likely to develop urinary incontinence than the non-athletic group[36].
- Increased BMI (above 25)/Obesity: Being overweight as measured by BMI, was strongly associated with urinary incontinence symptoms in both genders as was true for pelvic organ prolapse in women, compared to those with normal BMI values (18.5-24.9)[30][35][39]. With every 5 unit increase in BMI, the urinary incontinence risk rises to 20-70%. This is because of the increased intra-abdominal pressure that adds vesical compression and urethral movement. The continued weakening of pelvic floor muscles, nerve supply, and supporting structures, contribute to ineffective function[84].
- History of back pain: Low back pain has been noted to be closely related to pelvic floor muscle dysfunction. This is because the pelvic muscles have a role of providing stability for the lower back and bladder control continence. As a result, the discomfort experienced may cause individuals to avoid movement including the use of pelvic floor muscles. These muscles then become weak, unable to support the pelvic floor organs and alter urinary function. The researchers have found that due to pain levels in the low back, participants’ abilities to maximally contract the pelvic floor muscles was limited. Additionally, low back pain was attributed to loss of motor control in pelvic floor muscles, presenting as genito-urinary dysfunctions (i.e.urinary incontinence)[46].
- What is the role of the physio and assessment
- Implications:
- Urinary incontinence affects 69% of those with pelvic floor disorders. - PT
- Faecal incontinence affects 3.6 per 100,000 women aged 60-89. -PT
Financial burden:[edit | edit source]
- Physiotherapists and other healthcare professionals have an important role in reducing the financial constraints placed on the NHS.
- It is now understood that physiotherapists can improve patient outcomes predominantly through promoting self-management. This can be done through education on pelvic floor muscle training and lifestyle modifications which have already been described.
- Future focus on these areas should have a positive financial impact to the NHS.
- Currently, pelvic floor dysfunction has a huge financial burden to both the patient and the health service.
- Recent data on the costs for Scotland was not identified and the costs to the NHS as a whole does not appear to be well established.
- Hagen et al (2014) highlight that about 29,000 prolapse repairs were done in England between 2010 and 2011 which cost around £60 million.
- Estimations for the UK have been made by examining other countries data. For example, Cooper et al (2015) note that urinary incontinence in Sweden and the US accounts for 2% of their healthcare budget. They highlight that 2% of the UK budget would equate to £2.1 billion.
- Milsom et al (2014) reviewed the combined economic burden of urinary incontinence to several countries. Their findings indicate that for Canada and five European countries including the UK the combined cost was €7 billion a year with the UK accounting for €595 million of this total.
- Other evidence reviewed suggested that the combined burden for five European countries including the UK was €2.9 billion.
- Interestingly, the review also noted that the cost of urinary incontinence is expected to rise by 25% in the next ten years due to the aging population.
- Incontinence and pelvic floor exercises, surgery for (Critique and synthesis papers) (Who most benefits from PFE)
- Child birth
- Neuro-post stroke- PT more focused on mobility
- Age- Elderly
- Males- Erectile dysfunction, post surgery
- Summary of where more research needs to be done and PFE need to be incorporated in to
- More teaching of PFH in university.
- Emerging role of physio within stroke, elderly and long term care patients to increase PFE and decrease incontinence
- ?most research has been in child birth females and lacking in elderly, stroke and males
- Prevalence and impact for NHSThere is a lack of research of evidence surrounding pelvic floor health from a physiotherapy perspective; most research exists from nursing etc.
There is a bigger lack of research surrounding male pelvic floor health and implications of dysfunction etc.
There is a lack of awareness through a gap in the current education of student physiotherapists.
Evidence for physiotherapy[edit | edit source]
The evidence for physiotherapy:[edit | edit source]
Lifestyle:
- Weight loss is associated with is associated with improvements in urinary incontinence, particularly when combined with exercise[85].
- Strenuous activity or heavy lifting may be a predisposing factor for prolapse. There is limited evidence to support this and recommendations appear to be based on an understanding of the anatomy and physiology of prolapse[86].
- Some evidence suggests that decreasing fluid intake by 25% may decrease frequency, urgency and nocturia but may not improve incontinence[85].
- Caffeine reduction has been suggested to alleviate incontinence. However, the evidence for this is limited. A review by Gurovich et al (2016) found that caffeine restriction did not improve urinary incontinence symptoms[87]. Other evidence from Gleeson et al (2013) suggests that urinary incontinence is more prevalent in those with high caffeine intake[88]. Reducing caffeine intake may reduce overall fluid intake which may be the mechanism leading to improved symptoms. For this reason, reducing caffeine may be useful.
- The NICE guidelines recommend a trial of caffeine reduction in women with overactive bladder, to trial higher or lower fluid intake in women with UI or overactive bladder and recommend losing weight if BMI is over 30.
Exercise:
- Pelvic floor muscle training has been shown to be beneficial for both urinary incontinence and prolapse symptoms. Findings from a review by Dumoulin et al (2015) suggest that pelvic floor muscle training provides better outcomes compared to a control group in women with urinary incontinence[89]. Li et al (2016) found that those with pelvic organ prolapse undertaking pelvic floor muscle training had significantly greater improvements in subjective prolapse symptoms and objective prolapse severity compared to a control group[90].
- Pelvic floor training also seems to improve sexual function. The findings from a review by Ferreira et al (2015) suggest that pelvic floor muscle training can improve sexual function or at least one sexual variable in women with pelvic floor dysfunction[91].
- Interesting findings from two RCTs also corroborate the evidence for pelvic floor muscle training[92][93]. Alves et al (2015) found that twelve group sessions of pelvic floor muscle training increased pelvic floor muscle contractility (p = 0.01) while decreasing urinary symptoms (p < 0.01) and anterior pelvic organ prolapse (p = 0.03)[92]. Hagen et al (2014) found similar results with one to one sessions[93]. They did note that longer term investigations are required to strengthen the evidence.
- When prescribing a pelvic floor muscle training programme, adherence is important. According to a consensus statement by Dumoulin et al (2015), a structured PFMT programme, an enthusiastic physiotherapist, audio prompts, use of established theories of behavior change, and user-consultations seem to increase adherence[94].
- The identified evidence fails to make any recommendations on the optimal dosage of pelvic floor muscle training.
- The NICE guidelines recommend a trial supervised PFMT programme for at least 3 months as first line treatment for those with stress or urinary incontinence. At least 8 contractions three times a day.
Limitations and future research
- The evidence on pelvic floor dysfunction is lacking with the vast majority of the research focusing on urinary incontinence in particular.
- There is little evidence showing the effectiveness of lifestyle interventions. A lot of recommendations appear to be based on mechanistic and anecdotal evidence.
- Although pelvic floor muscle training appears to be effective, the optimal type and dosage of this training has not been established.
- Almost all of the literature and guidelines on pelvic floor dysfunction focuses on the female population. Far more research is required in the male population.
Quiz answers
1.Name 3 functions of the pelvic floor? Any of the following
- Support internal pelvic organs in the correct positions (Bladder, bowel and vagina).
- Allow conscious control of bladder and bowel habits using the sphincter muscles. This allows us to control the release of urine (wee), faeces (poo) and gas and to delay emptying until a convenient time. This works as the pelvic floor muscles contract and the pelvic organs are lifted up. The sphincter then tightens around the openings of the urethra and anus.
- Allow the passage of urine and faeces out of the body due to the pelvic floor muscles relaxing and allowing the passages to open.
- Sexual function
- In males the pelvic floor muscles are important in erectile function by increasing rigidity and ejaculation by improving control and coordination between circulation, pelvic floor muscles.
- In females voluntary contraction of the pelvic floor muscles can contribute to sexual sensation.
- As mentioned above the pelvic floor muscles play a role in breathing by relaxing and increasing the space the lungs have to expand.
- Additionally in pregnant women the pelvic floor offers support to the foetus during pregnancy and also assists in the childbirth process.
2.When and why is having a strong pelvic floor important?
- During coughing, laughing, sneezing or during lifting activities there is extra force added to the abdomen and therefore additional pressure down onto the pelvic floor
3.Can you name 3 signs and symptoms for each male and female?any of the following
Male
- Constipation or bowel strains
- Ongoing pain in your pelvic region, genitals or rectum.
- A prolapse – may feel as though there is a bulge/ pressure in the rectum or a feeling of needing to use your bowels without actually needing to go. - Accidentally leaking urine when you exercise, laugh, cough or sneeze.
- Feelings of urgency in needing to the bathroom, or not making it there in time.
- Frequent need to urinate.
- Difficultly emptying your bladder (discontinuous urination – stop and start multiple times) and bowels.
- The feeling of needing to have several bowel movements during a short period of time.
- Accidentally passing wind.
- Pain in your lower back that cannot be explained by other causes.
- Pain in the testicles, penis (referred pain from the pelvic floor) or pelvis during intercourse.
- Erectile dysfunction.
- Painful ejaculation.
- Premature ejaculation.
Female
- Pain or numbness during intercourse.
- Ongoing pain in your pelvic region, genitals or rectum.
- A prolapse – may be felt as a bulge in the vagina (feeling or seeing a bulge or lump in or coming out of your vagina) or a feeling of heaviness, discomfort, pulling, dragging or dropping sensation.
- Accidentally leaking urine when you exercise, laugh, cough or sneeze (stress incontinence).
- Feelings of urgency in needing to the bathroom, or not making it there in time.
- Frequent need to urinate.
- Difficultly emptying your bladder (discontinuous urination – stop and start multiple times) and bowels.
- The feeling of needing to have several bowel movements during a short period of time.
- Constipation or bowel strains.
- Accidentally passing wind.
- Pain in your lower back that cannot be explained by other causes.
- 4.Can you name 2 risk factors for pelvic floor dysfunction for males, females and both? Any of the following
Male:
- Prostate surgery
Women:
- Age: Menopausal age (48-55)
- Pregnancy and the nature of childbirth
- Genetics and family history
- Hysterectomy (surgical removal of uterus)
Both Genders:
- Previous injury to pelvic region (e.g. fall or pelvic radiotherapy)
- Increased abdominal pressure
- Constipation/heavy lifting
- Intense physical effort
- Obesity
- History of back pain
5.What 2 ways a physiotherapist my do to treat pelvic floor dysfunction?
- Teach you about how to do your pelvic floor exercise
- Advice of lifestyle modifications you can try
6.Who to can you contact to get referred to pelvic floor physiotherapy?
- Area dependant:
- Self referral
- GP referral
- Midwife referral
7.What NHS approved app that was developed to help with your pelvic floor exercises?
- Squeezy
8.Can you describe the steps to performing a pelvic floor contraction
*******Will add this in when its in the treatment section
9.Name 2 lifestyle changes you try to aid pelvic floor function?
- Reduce caffeine and other irritants of the bladder
- The “knack”
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 ABRAMS, P., SMITH, A.P. and COTTERILL, N., 2015. The impact of urinary incontinence on health‐related quality of life (HRQoL) in a real‐world population of women aged 45–60 years: results from a survey in France, Germany, the UK and the USA. BJU International. vol. 115, no. 1, pp. 143-152.
- ↑ 2.0 2.1 2.2 2.3 2.4 MAXWELL, M., SEMPLE, K., WANE, S., ELDERS, A., DUNCAN, E., ABHYANKAR, P., WILKINSON, J., TINCELLO, D., CALVELEY, E. and MACFARLANE, M., 2017. PROPEL: implementation of an evidence based pelvic floor muscle training intervention for women with pelvic organ prolapse: a realist evaluation and outcomes study protocol. BMC Health Services Research. vol. 17, no. 1, pp. 843.
- ↑ 3.0 3.1 3.2 COOPER, J., ANNAPPA, M., QUIGLEY, A., DRACOCARDOS, D., BONDILI, A. and MALLEN, C., 2015. Prevalence of female urinary incontinence and its impact on quality of life in a cluster population in the United Kingdom (UK): a community survey. Primary Health Care Research & Development. vol. 16, no. 4, pp. 377-382.
- ↑ 4.0 4.1 4.2 BEDRETDINOVA, D., FRITEL, X., ZINS, M. and RINGA, V., 2016. The effect of urinary incontinence on health-related quality of life: is it similar in men and women? Urology. vol. 91, pp. 83-89.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 CONTINENCE FOUNDATION OF AUSTRALIA., 2018. Pelvic Floor Muscles in Men [online] [viewed 28 March 2018] Available from:https://www.continence.org.au/pages/pelvic-floor-men.html
- ↑ 6.0 6.1 PELVIC FLOOR FIRST., 2016. The Pelvic Floor [online] [viewed 23 March 2018]. Available from:http://www.pelvicfloorfirst.org.au/pages/the-pelvic-floor.html
- ↑ CONTINENCE FOUNDATION OF AUSTRALIA., 2018. Pelvic Floor Muscles [online] [viewed 6 April 2018]. Available from:https://www.continence.org.au/pages/how-do-pelvic-floor-muscles-help.html
- ↑ PELVIC OBSTETRIC AND GYNAECOLOGICAL PHYSIOTHERAPY., 2016. Pelvic Floor Muscles Exercise for Men [online] [viewed 22 March 2018]. Available from:http://pogp.csp.org.uk/publications/pelvic-floor-muscle-exercises-men
- ↑ PELVIC CORE FIRST., 2016. The Pelvic Floor and Core [online] [viewed 29 March 2018]. Available from:http://www.pelvicfloorfirst.org.au/pages/the-pelvic-floor-and-core.html
- ↑ 10.0 10.1 10.2 10.3 PELVIC HEALTH AND REHAB CENTRE., 2017. Understanding Pelvic Floor Movement [online] [Viewed 28 March 2018]. Available from:https://www.pelvicpainrehab.com/low-tone-pelvic-floor-dysfunction/4587/pelvic-floor-movement/
- ↑ 11.0 11.1 11.2 11.3 FOUNDATION PHYSIOTHERAPY., 2018. 5 Basic Functions of your Pelvic Floor [online] [viewed 29 March 2018]. Available from:http://www.foundationphysio.com/5-basic-functions-of-your-pelvic-floor/
- ↑ PROSTATE.NET., 2016. Erectile Dysfunction and the Pelvic Floor Connection [online] [viewed 19 March 2018]. Available from: https://prostate.net/articles/erectile-dysfunction-pelvic-floor-connection
- ↑ BETTER HEALTH CHANNEL., 2017. Pelvic Floor [online] [viewed 28 March 2018]. Available from:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pelvic-floor
- ↑ MALE PELVIC FLOOR., 2012. Sexual Dysfunction and the Male Pelvic Floor [online] [viewed 29 March 2018]. Available from:http://malepelvicfloor.com/sd.html
- ↑ MALE PELVIC FLOOR., 2012. Urinary Dysfunction and the Male Pelvic Floor [online] [viewed 29 March 2018]. Available from:http://malepelvicfloor.com/urinary.html
- ↑ NHS CHOICES., 2018. Pelvic Organ Prolapse Overview [online] [viewed 29 March 2018]. Available from: https://www.nhs.uk/conditions/pelvic-organ-prolapse/
- ↑ 17.0 17.1 17.2 HEALTHLINE., 2017. Pelvic Floor Dysfunction [online] [viewed 26 March 2018]. Available from: https://www.healthline.com/health/pelvic-floor-dysfunction#symptoms
- ↑ 18.0 18.1 18.2 18.3 18.4 MALE PELVIC FLOOR., 2012. Male Pelvic Floor - Advanced Massage and Bodywork [online] [viewed 26 March 2018]. Available from: http://malepelvicfloor.com/sd.html
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 WOMEN'S AND MEN'S HEALTH PHYSIOTHERAPY., 2017. Leading the way in pelvic health [online] [viewed 28 March 2018]. Available from: http://www.wmhp.com.au/
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 20.6 20.7 20.8 20.9 PELVIC FLOOR FIRST., 2017. Pelvic Floor First [online] [viewed 26 March 2018]. Available from: http://www.pelvicfloorfirst.org.au/pages/how-can-i-tellif-i-have-a-pelvic-floor-problem.html
- ↑ 21.0 21.1 21.2 21.3 21.4 PELVIC OBSTECTRIC AND GYNAECOLOGICAL PHYSIOTHERAPY., 2016. Pelvic floor muscle exercises (for men) [online] [viewed 26 March 2018]. Available from: http://pogp.csp.org.uk/publications/pelvic-floor-muscle-exercises-men
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 22.6 NHS CHOICES., 2017. Living with incontinence [online] [viewed 28 March 2018]. Available from: https://www.nhs.uk/Livewell/incontinence/Pages/Livingwithincontinence.aspx
- ↑ 23.0 23.1 HAY-SMITH, E., RYAN, K. and DEAN, S., 2007. The silent, private exercise: experiences of pelvic floor muscle training in a sample of women with stress urinary incontinence. Physiotherapy. vol. 93, no. 1, pp. 53-61.
- ↑ 24.0 24.1 24.2 24.3 24.4 .MASON, L., GLENN, S., WALTON, I. and HUGHES, C., 2001. The instruction in pelvic floor exercises provided to women during pregnancy or following delivery. Midwifery. 2001, vol. 17, no. 1, pp. 55-64.
- ↑ 25.0 25.1 25.2 25.3 25.4 NEELS, H., DE WACHTER, S., WYNDAELE, J., VAN AGGELPOEL, T. and VERMANDEL, A., 2018. Common errors made in attempt to contract the pelvic floor muscles in women early after delivery: A prospective observational study. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 01, vol. 220, pp. 113-117.
- ↑ 26.0 26.1 HIRSCHHORN, A.D., KOLT, G.S. and BROOKS, A.J., 2013. Barriers and enablers to the provision and receipt of preoperative pelvic floor muscle training for men having radical prostatectomy: a qualitative study. BMC Health Services Research. vol. 13, no. 1, pp. 305.
- ↑ 27.0 27.1 DOREY,G., 2013. Pelvic floor exercises after radical prostatectomy. British Journal of Nursing.October,vol.14, no.5, pp.457-464.
- ↑ 28.0 28.1 HOYLAND, K., VASDEV, N., ABROF, A. and BOUSTEAD, G., 2014. Post-radical prostatectomy incontinence: etiology and prevention. Reviews in urology. October, vol.16, no.4, p.181-188.
- ↑ DURAN, S., 2014. Pregnant Woman [online]. [viewed 04 April 2018]. Available from: https://dribbble.com/shots/1447791-Pregnant-Woman
- ↑ 30.0 30.1 30.2 30.3 30.4 30.5 30.6 VERGELDT, T.F., WEEMHOFF, M., INTHOUT, J. and KLUVIERS, K.B., 2015. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. International urogynecology journal. November, vol.26, no.11, pp.1559-1573.
- ↑ 31.0 31.1 31.2 31.3 31.4 WU, J.M., VAUGHN, C.P., GOODE, P.S., REDDEN, D.T., BURGIO, K.L., RICHTER, H.E. and MARKLAND, A.D., 2014. Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstetrics and gynecology, January, vol. 123, no.1, p.141-148.
- ↑ 32.0 32.1 32.2 32.3 32.4 32.5 32.6 KUNCHARAPU, I., MAJERONI, B.A. and JOHNSON, D.W., 2010. Pelvic organ prolapse. Am Fam Physician. May, vol.81, no.9, pp.1111-1117.
- ↑ 33.0 33.1 33.2 HANDA, V.L., BLOMQUIST, J.L., McDERMOTT, K.C., FRIEDMAN, S. and MUNOZ, A., 2012. Pelvic floor disorders after childbirth: effect of episiotomy, perineal laceration, and operative birth. Obstetrics and gynecology. February,vol.119, no.2, p.233-239.
- ↑ 34.0 34.1 LINCE, S.L., van KEMPEN, L.C., VIERHOUT, M.E. and KLUVIERS, K.B., 2012. A systematic review of clinical studies on hereditary factors in pelvic organ prolapse. International urogynecology journal. October, vol.23, no.10, pp.1327-1336.
- ↑ 35.0 35.1 35.2 35.3 35.4 35.5 BO, K., 2012. Urinary incontinence, pelvic floor dysfunction, exercise and sport. Sports Medicine. June,vol.34, no.7, pp.451-464.
- ↑ 36.0 36.1 36.2 36.3 36.4 36.5 36.6 NYGAARD, I.E. and SHAW, J.M., 2016. Physical activity and the pelvic floor. American Journal of Obstetrics & Gynecology. February, vol. 214, no.2, pp.164-171.
- ↑ 37.0 37.1 37.2 LUKANOVIC, A. and DRAZIC, K., 2010. Risk factors for vaginal prolapse after hysterectomy. International Journal of Gynecology & Obstetrics. July, vol.110, no.1, pp.27-30.
- ↑ 38.0 38.1 HUMALAJARVI, N., AUKEE P., KAIRALUOMA, M.V., STACH-LEMPINEN, B., SINTONEN, H., VALPAS, A. and HEINONEN, P.K., 2014. Quality of life and pelvic floor dysfunction symptoms after hysterectomy with or without pelvic organ prolapse. European Journal of Obstetrics and Gynecology and Reproductive Biology. November, vol.182, no.1, pp.16-21.
- ↑ 39.0 39.1 39.2 39.3 THOMAS, R.J., HOLM, M., WILLIAMS, M., BOWMAN, E., BELLAMY, P., ANDREYEV, J. and MAHER, J., 2013. Lifestyle factors correlate with the risk of late pelvic symptoms after prostatic radiotherapy. Clinical Oncology. April, vol. 25, no.4, pp.246-251.
- ↑ 40.0 40.1 WALTERS, M.D., 2017. Pelvic floor disorders in women: an overview. Revista de Medicina de la Universidad de Navarra. October, vol. 48, no. 4, pp.9-18.
- ↑ KHANDELWAL, C. and KISTLER, C., 2013. Diagnosis of urinary incontinence. Am Fam Physician. April, vol. 87, no.8, pp.543-550.
- ↑ 42.0 42.1 CHOI, K.H. and HONG, J.Y., 2014. Management of pelvic organ prolapse. Korean journal of urology. November, vol.55, no.11, pp.693-702.
- ↑ COBB, R.,2018. Animation LOL GIF by Robbie Cobb [online]. [viewed 04 April 2018]. Available from: https://giphy.com/gifs/laugh-dennys-diner-3oEduQQQAR2a4y6Cek
- ↑ JAMSHED, N., LEE, Z.E. and OLDEN, K.W., 2011. Diagnostic approach to chronic constipation in adults. American family physician. August, vol. 84, no.3, p.299-306.
- ↑ 45.0 45.1 NASER, S.S.A. and SHAATH, M.Z., 2016. Expert system urination problems diagnosis. World Wide Journal of Multidisciplinary Research and Development, vol.2, no.5, pp.9-19.
- ↑ 46.0 46.1 ARAB, A.M., BEHBAHANI, R.B., LORESTANI, L. and AZARI, A., 2010. Assessment of pelvic floor muscle function in women with and without low back pain using transabdominal ultrasound. Manual therapy. June, vol.15, no.3, pp.235-239.
- ↑ PELVIC FLOOR FIRST., 2017. Who's at risk? [online] [viewed 28 March 2018]. Available from: www.pelvicfloorfirst.org.au/pages/are-you-at-risk.html
- ↑ CONTINENCE FOUNDATION OF AUSTRALIA., 2018. Common problems with pelvic floor muscles [online] [viewed 28 March 2018]. Available from: https://www.continence.org.au/pages/what-can-happen-to-the-pelvic-floor-muscles.html
- ↑ 49.0 49.1 CLEVELAND CLINIC., 2018. Pelvic floor dysfunction. [online]. [viewed March 10, 2018]. Available from: https://my.clevelandclinic.org/health/diseases/14459-pelvic-floor-dysfunction/management-and-treatment
- ↑ ROBERT, M., and ROSS, S., 2006. Conservative management of urinary incontinence. Journal of Obstetrics and Gynaecology Canada. Vol. 28 (12), pp. 1113-1118.
- ↑ 51.0 51.1 51.2 AYELEKE, R., HAY-SMITH, E. & OMAR, M., 2015. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database of Systematic Reviews.
- ↑ 52.0 52.1 KNOWLES, K., 2018. Pelvic floor Dysfunction [online]. PHYSIOWORKS [viewed online March 26, 2018]. Available from: https://physioworks.com.au/Injuries-Conditions/Regions/pelvic-floor-dysfunction
- ↑ 53.0 53.1 PHYSIOTHERAPY NEW ZEALAND., 2018. How Physio can help: Pelvic Floor Disorders. [online]. [viewed March 10, 2018]. Available from: http://physiotherapy.org.nz/your-health/how-physio-can-help/pelvic-floor-disorders
- ↑ USMLEFastTrack. Progressive PFE Episode 1. Available from: https://www.youtube.com/watch?v=HrRjumD_o4s [last accessed 10/03/18]
- ↑ USMLEFastTrack. Progressive PFE Episode 2. Available from: https://www.youtube.com/watch?v=lwM_wwjerv8&list=PLqo18HBnle8zPU3gLkr9l49iAotngDB21&index=7 [last accessed 10/03/18]
- ↑ USMLEFastTrack. Progressive PFE Episode 3. Available from: https://www.youtube.com/watch?v=lp0ND0s3ZHQ&list=PLqo18HBnle8x4NKtYCobjU3DYmnJrOJA-&index=3 [last accessed 10/03/18]
- ↑ USMLEFastTrack. Progressive PFE Episode 4. Available from: https://www.youtube.com/watch?v=wRKhtfbJHdo [last accessed 10/03/18]
- ↑ USMLEFastTrack. Progressive PFE Episode 5. Available from: https://www.youtube.com/watch?v=OKvP3C8-Jxc&index=5&list=PLqo18HBnle8x4NKtYCobjU3DYmnJrOJA-[last accessed 10/03/18]
- ↑ SASKATCHEWAN MINISTRY OF HEALTH, 2014. Information for women about urinary incontinence and vaginal prolapse. [online]. [viewed March 26, 2018]. Available from: http://www.sasksurgery.ca/pdf/self-management-incontinence.pdf
- ↑ 60.0 60.1 NHS., 2018. Urinary Incontinence. [online]. [viewed March 10, 2018]. Available from: https://www.nhs.uk/conditions/urinary-incontinence
- ↑ NHS, 2018. Urinary Incontinence - Surgery and Procedures [online]. [viewed March 26, 2018]. Available from: https://www.nhs.uk/conditions/urinary-incontinence/surgery/
- ↑ NATIONAL INSTITUTE OF CHILD HEALTH AND HUMAN DEVELOPMENT, 2018. How are pelvic floor disorders commonly treated? [online]. [viewed March 26, 2018] Available from: https://www.nichd.nih.gov/health/topics/pelvicfloor/conditioninfo/treatment
- ↑ Moore, K.L., Dalley, A.F. and Agur, A.M., 2013. Clinically oriented anatomy. Lippincott Williams & Wilkins.
- ↑ Palastanga, N. and Soames, R., 2011. Anatomy and human movement, structure and function. Elsevier Health Sciences.
- ↑ Drake, R., Vogl, A.W. and Mitchell, A.W., 2009. Gray's Anatomy for Students E-Book. Elsevier Health Sciences.
- ↑ 66.0 66.1 Hendrix, S.L., Clark, A., Nygaard, I., Aragaki, A., Barnabei, V. and McTiernan, A., 2002. Pelvic organ prolapse in the Women's Health Initiative: gravity and gravidity. American Journal of Obstetrics & Gynecology. Vol. 186, no. 6, pp.1160-1166.
- ↑ MAYO CLINIC., 2014. Anterior Prolapse (Cystocele) [online] [viewed 9 April 2018]. Available from: https://www.mayoclinic.org/diseases-conditions/cystocele/symptoms-causes/syc-20369452
- ↑ Polden, M. and Mantle, J., 1990. Physiotherapy in obstetrics and gynaecology. Elsevier Health Sciences.
- ↑ THE URETHRA CLINIC., 2017. Controversies in Management of Pelvic Fracture Urethral Injuries [online] [viewed 9 April 2018]. Available from:[/www.theurethraclinic.com/blog/controversies-management-pelvic-fracture-urethral-injuries/ https://www.theurethraclinic.com/blog/controversies-management-pelvic-fracture-urethral-injuries/]
- ↑ Jelovsek, J.E., Maher, C. and Barber, M.D., 2007. Pelvic organ prolapse. The Lancet. Vol. 369, no. 9566, pp.1027-1038.
- ↑ Weber, A.M. and Richter, H.E., 2005. Pelvic organ prolapse. Obstetrics & Gynecology. Vol. 106, no. 3, pp.615-634.
- ↑ Kuncharapu, I., Majeroni, B.A. and Johnson, D.W., 2010. Pelvic organ prolapse. Am Fam Physician. Vol. 81, no. 9, pp.1111-1117.
- ↑ MACFARLANE, K., 2018. Due Diligence and Keeping Lone Workers Safe [online]. [viewed 04 April 2018]. Available from: https://safetylineloneworker.com/blog/due-diligence-and-keeping-lone-workers-safe-2/
- ↑ BERGHMANS, B., NIEMAN, F., LEUE, C., WEEMHOFF, M., BREUKINK, S. and VAN KOEVERINGE, G., 2016. Prevalence and triage of first contact pelvic floor dysfunction complaints in male patients referred to a Pelvic Care Centre. Neurourology and urodynamics. April,vol.35, no.4, pp.487-491.
- ↑ KIRBY, A.C., LUBER, K.M. and MENEFEE, S.A., 2013. An update on the current and future demand for care of pelvic floor disorders in the United States. American Journal of Obstetrics & Gynecology. August, vol.209, no.6, pp.584-e1.
- ↑ NHS TRUST., 2014. National Health Service [online]. [viewed 19th March 2018]. Available from: http://www.ouh.nhs.uk/patient-guide/leaflets/files/11124Ppelvic.pdf
- ↑ CSP., 2014. Chartered Society of Physiotherapy [online]. [viewed 19 March 2018]. Available from: www.csp.org.uk/sites/files/csp/secure/pogp-pelvicfloor-male.pdf
- ↑ GLINA, S., 2011. Erectile dysfunction after radical prostatectomy. Drugs & aging. April, vol.28, no.4, pp.257-266.
- ↑ FROTA, I.P.R., ROCHA, A.B.O., NETO, J.A.V., VASCONCELOS, C.T.M., DE MAGALHAES, T.F., KARBAGE, S.A.L., AUGUSTO, K.L., NASCIMENTO, S.L.D., HADDAD, J.M. and BEZERRA, L.R.P.S., 2018. Pelvic floor muscle function and quality of life in postmenopausal women with and without pelvic floor dysfunction. Acta obstetricia et gynecologica Scandinavica.
- ↑ CAMPEAU, L., GORBACHINSKY, I., BADLANI, G.H. and Andersson, K.E., 2011. Pelvic floor disorders: linking genetic risk factors to biochemical changes. BJU international, October, vol.108, no.8, pp.1240-1247.
- ↑ HARTIGAN, S.M. and SMITH, A.L., 2018. Disparities in Female Pelvic Floor Disorders. Current urology reports. February, vol.19, no.2, p.16-22.
- ↑ JAMSHED, N., LEE, Z.E. and OLDEN, K.W., 2011. Diagnostic approach to chronic constipation in adults. American family physician. August, vol. 84, no.3, p.299-306.
- ↑ CONTINENCE FOUNDATION AUSTRALIA 2016. [online] [viewed 17 March 2018]. Available from: http://www.pelvicfloorfirst.org.au/pages/are-you-at-risk.html.
- ↑ RAMALINGAM, K. and MONGA, A., 2015. Obesity and pelvic floor dysfunction. Best practice & research Clinical obstetrics & gynaecology. May, vol.29, no.4, pp.541-547.
- ↑ 85.0 85.1 DUMOULIN, C., HUNTER, K.F., MOORE, K., BRADLEY, C.S., BURGIO, K.L., HAGEN, S., IMAMURA, M., THAKAR, R., WILLIAMS, K. and CHAMBERS, T., 2016. Conservative management for female urinary incontinence and pelvic organ prolapse review 2013: Summary of the 5th International Consultation on Incontinence. Neurourology and Urodynamics. vol. 35, no. 1, pp. 15-20.
- ↑ DWYER, L. and KEARNEY, R., 2017. Conservative management of pelvic organ prolapse. Obstetrics, Gynaecology & Reproductive Medicine.
- ↑ GUROVICH, M., FAGERSTROM, C., PRIETO, M. and SANCHEZ, H., 2016. Recommendations for Caffeine Intake Reduction in Women with Urinary Incontinence: A Systematic Review of Literature. Int J Womens Health Wellness. vol. 2, pp. 035.
- ↑ GLEASON, J.L., RICHTER, H.E., REDDEN, D.T., GOODE, P.S., BURGIO, K.L. and MARKLAND, A.D., 2013. Caffeine and urinary incontinence in US women. International Urogynecology Journal. vol. 24, no. 2, pp. 295-302.
- ↑ DUMOULIN, C., HAY‐SMITH, J., HABÉE‐SÉGUIN, G.M. and MERCIER, J., 2015. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: A short version Cochrane systematic review with meta‐analysis. Neurourology and Urodynamics. vol. 34, no. 4, pp. 300-308.
- ↑ LI, C., GONG, Y. and WANG, B., 2016. The efficacy of pelvic floor muscle training for pelvic organ prolapse: a systematic review and meta-analysis. International Urogynecology Journal. vol. 27, no. 7, pp. 981-992.
- ↑ FERREIRA, C.H.J., DWYER, P.L., DAVIDSON, M., DE SOUZA, A., UGARTE, J.A. and FRAWLEY, H.C., 2015. Does pelvic floor muscle training improve female sexual function? A systematic review. International Urogynecology Journal. vol. 26, no. 12, pp. 1735-1750.
- ↑ 92.0 92.1 ALVES, F.K., RICCETTO, C., ADAMI, D.B., MARQUES, J., PEREIRA, L.C., PALMA, P. and BOTELHO, S., 2015. A pelvic floor muscle training program in postmenopausal women: A randomized controlled trial. Maturitas. Jun, vol. 81, no. 2, pp. 300-305.
- ↑ 93.0 93.1 HAGEN, S., STARK, D., GLAZENER, C., DICKSON, S., BARRY, S., ELDERS, A., FRAWLEY, H., GALEA, M.P., LOGAN, J. and MCDONALD, A., 2014. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. The Lancet. vol. 383, no. 9919, pp. 796-806.
- ↑ DUMOULIN, C., ALEWIJNSE, D., BO, K., HAGEN, S., STARK, D., VAN KAMPEN, M., HERBERT, J., HAY‐SMITH, J., FRAWLEY, H. and MCCLURG, D., 2015. Pelvic‐Floor‐Muscle Training Adherence: Tools, Measurements and Strategies—2011 ICS State‐of‐the‐Science Seminar Research Paper II of IV. Neurourology and Urodynamics. vol. 34, no. 7, pp. 615-621.
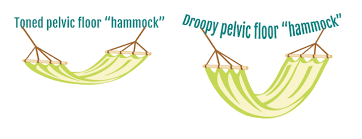
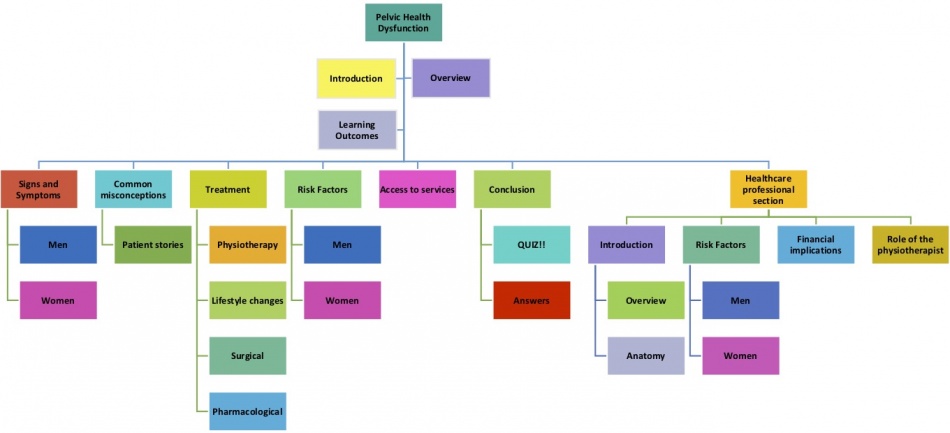
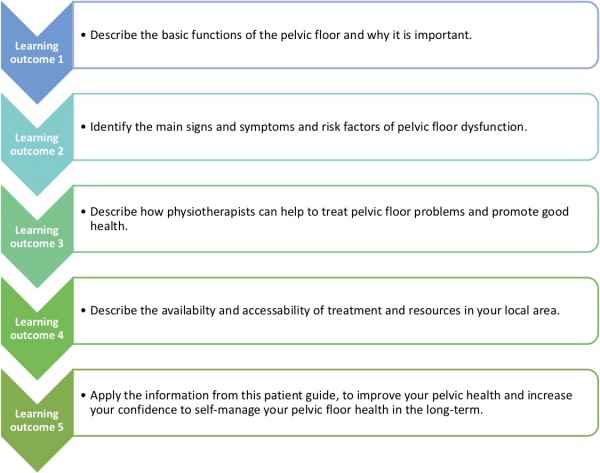
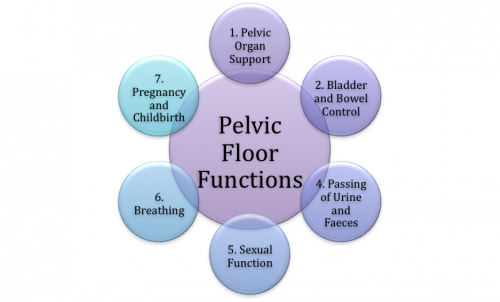
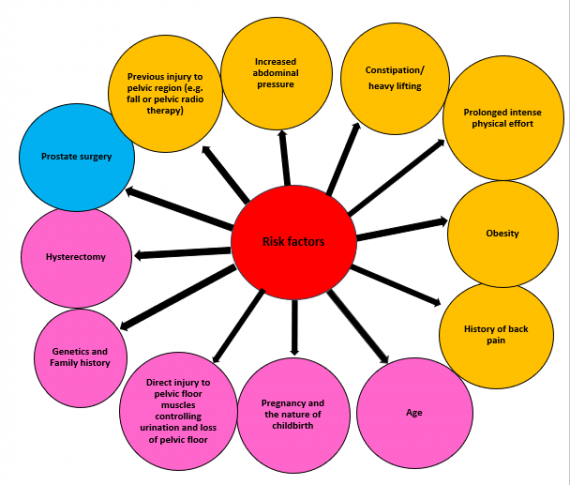
![[29]](/images/thumb/1/13/Pregnancy_as_a_risk_factor_for_women.gif/300px-Pregnancy_as_a_risk_factor_for_women.gif)
![[43]](/images/thumb/b/b7/Heavy_lifting-risk_factors.gif/300px-Heavy_lifting-risk_factors.gif)

![[73]](/images/thumb/e/e1/Risks.jpg/377px-Risks.jpg)






