Patellofemoral Instability: Difference between revisions
Michelle Lee (talk | contribs) No edit summary |
Michelle Lee (talk | contribs) No edit summary |
||
| Line 8: | Line 8: | ||
== Definition/Description == | == Definition/Description == | ||
A frequent cause of knee pain and knee disability is patellofemoral instability. Patellofemoral instability can be defined in different ways. One way is when the patient has undergone a traumatic dislocation of the patella. It can also describe a sign on physical examination, signifying the ability of the patella to be translated out of the trochlear groove of the femur in a passive manner. Moreover, patellofemoral instability can be a symptom, when the patient gives a feeling that the knee “gives way’’. This feeling occurs when the patella slips out of the trochlear groove. The relationships between the symptoms, injuries and diseases of the patellofemoral joint are often confusing for the therapist.[[|]]<ref>Fulkerson, J.P. et al., Disorders of the patellofemoral joint, USA, Williams &amp; Wilkins, 1997, p.175-187, 199-216, 275-297</ref> | A frequent cause of knee pain and knee disability is patellofemoral instability. Patellofemoral instability can be defined in different ways. One way is when the patient has undergone a traumatic dislocation of the patella. It can also describe a sign on physical examination, signifying the ability of the patella to be translated out of the trochlear groove of the femur in a passive manner. Moreover, patellofemoral instability can be a symptom, when the patient gives a feeling that the knee “gives way’’. This feeling occurs when the patella slips out of the trochlear groove. The relationships between the symptoms, injuries and diseases of the patellofemoral joint are often confusing for the therapist.[[|]]<ref>Fulkerson, J.P. et al., Disorders of the patellofemoral joint, USA, Williams &amp;amp; Wilkins, 1997, p.175-187, 199-216, 275-297</ref> | ||
<br> | <br> | ||
| Line 53: | Line 53: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Patellar instability is normally diagnosed through a comprehensive history of the patient's symptoms and functional objective assessment of the knee. Further scans such as MRI's and Ultrasound imaging can be performed to rule out any strutural defecits. | Patellar instability is normally diagnosed through a comprehensive history of the patient's symptoms and functional objective assessment of the knee. Further scans such as MRI's and Ultrasound imaging can be performed to rule out any strutural defecits. | ||
== Outcome Measures == | == Outcome Measures == | ||
| Line 59: | Line 59: | ||
There are many outcome measures that can be used with this condition, currently there are no specific reccomendations from COMET therefore it is up to the clinician to clinically reason which outcome measue would be most approprite for their paient. Here are a few: | There are many outcome measures that can be used with this condition, currently there are no specific reccomendations from COMET therefore it is up to the clinician to clinically reason which outcome measue would be most approprite for their paient. Here are a few: | ||
*[http://www.physio-pedia.com/File:Anterior_knee_pain_scale.pdf Anterior Knee Pain Scale ] | *[http://www.physio-pedia.com/File:Anterior_knee_pain_scale.pdf Anterior Knee Pain Scale ] | ||
*[http://www.physio-pedia.com/File:LEFS.pdf Lower Extremity Functional Scale] | *[http://www.physio-pedia.com/File:LEFS.pdf Lower Extremity Functional Scale] | ||
*[http://www.physio-pedia.com/File:Pain_assessment_scales.pdf Pain Assessment Scales] | *[http://www.physio-pedia.com/File:Pain_assessment_scales.pdf Pain Assessment Scales] | ||
*[http://www.physio-pedia.com/Numeric_Pain_Rating_Scale Numeric Pain Rating Scale ] | *[http://www.physio-pedia.com/Numeric_Pain_Rating_Scale Numeric Pain Rating Scale ] | ||
| Line 70: | Line 70: | ||
'''Physical Examination:'''<br>The second diagnostic step is a careful, complete and essential physical examination. The purpose of this examination is to reproduce the symptoms (pain/instability) and to locate the painful zone. The location can indicate which structure is injured, it is truly helpful to compose the diagnosis and to plan the treatment. | '''Physical Examination:'''<br>The second diagnostic step is a careful, complete and essential physical examination. The purpose of this examination is to reproduce the symptoms (pain/instability) and to locate the painful zone. The location can indicate which structure is injured, it is truly helpful to compose the diagnosis and to plan the treatment. | ||
< | '''Tests:<ref>Vicente Sanchis-Alfonso, Anterior Knee Pain and Patellar Instability, Second Edition, 2011, p108-120</ref>''' | ||
'''1) Fairbanks [http://www.physio-pedia.com/Moving_Patellar_Apprehension_Test#Technique patellar apprehension test]:''' | |||
The test is positive, when there is pain and muscle defensive contraction of lateral patellar dislocation with 20°–30° of knee flexion. The positive test indicates that lateral patellar instability is an important part of the patient’s problem. This may be so positive that the patient pulls the leg back when the therapist approaches the knee with his hand, preventing so any contact, or the patient grabs the therapist’s arm. <br> --> 100% sensitivity, 88.4% specificity, and overall accuracy of 94.1%<ref>Christopher S. Ahmad et al., The Moving Patellar Apprehension Test for Lateral Patellar Instability, The American Journal of Sports Medicine</ref> | |||
'''2) Patellar glide test:'''<br>This test is used to evaluate the instability. A medial/lateral displacement of the patella greater than or equal to 3 quadrants, with this test, is consistent with incompetent lateral/medial restraints. Lateral patellar instability is more frequent than medial instability. <br> | '''2) Patellar glide test:'''<br>This test is used to evaluate the instability. A medial/lateral displacement of the patella greater than or equal to 3 quadrants, with this test, is consistent with incompetent lateral/medial restraints. Lateral patellar instability is more frequent than medial instability. <br> | ||
== Physical Therapy Management <br> == | == Physical Therapy Management <br> == | ||
| Line 88: | Line 83: | ||
'''Nonoperative treatment:'''<br>It is a treatment that consists of immobilization followed by a period of structured rehabilitation. Immobilization is granted for healing of the soft tissues, especially the supporting structures on the medial side of the knee. Today brace treatment with early mobilization has become the norm, instead of the traditional immobilization of 3 to 6 weeks in a cylinder cast. | '''Nonoperative treatment:'''<br>It is a treatment that consists of immobilization followed by a period of structured rehabilitation. Immobilization is granted for healing of the soft tissues, especially the supporting structures on the medial side of the knee. Today brace treatment with early mobilization has become the norm, instead of the traditional immobilization of 3 to 6 weeks in a cylinder cast. | ||
Most of the time these therapies start with the initial straight-leg raises: | Most of the time these therapies start with the initial straight-leg raises: Quadriceps setting exercises and three sets of 15 to 20 [http://www.physio-pedia.com/Patellofemoral_Pain_Syndrome#Physical_Therapy_Management straight leg raises] are done four or five times a day during the acute period. Ice is applied for 20 minutes every 2 to 3 hours to reduce swelling.<ref>Reuven Minkowitz, M.D., Chris Inzerillo, M.D., and Orrin H.Sherman,M.D., Patella Instability, Bulletin of the NYU Hospital for Joint Diseases 2007</ref> <br>It is followed by stationary bicycle for passive and active motion, isotonic and isometric quadriceps strengthening. Between 3 and 8 weeks, the return to full activities was allowed when tenderness weakened and isotonic quadriceps strength was bilateral. <br>In up to two-third of the knees the results were good to excellent, these results consist of a first-time acute dislocation, compared with only 50% of those with a recurrent dislocation. In general, 73% were satisfied with their knees, but 16% were not and eventually decided to have surgical stabilization.<br>Those with acute patellar dislocation can expect an extended rehabilitation period before returning to sport, whether immobilized or not. | ||
=== <br>Patellofemoral Instability: Recurrent Dislocation of the Patella === | === <br>Patellofemoral Instability: Recurrent Dislocation of the Patella === | ||
'''Nonoperative treatment '''<br>Surgery is not necessarily needed for patients with patellofemoral malalignment | '''Nonoperative treatment '''<br>Surgery is not necessarily needed for patients with patellofemoral malalignment or relaxation of the patella. Adequate results can be achieved with a conservative exercise treatment program. It is very important in [http://www.physio-pedia.com/Patellofemoral_Pain_Syndrome#Physical_Therapy_Management the rehabilitation program to strengthen the quadriceps muscle and vastus medialis obliquus (VMO)]. It’s advised to follow the program which is similar to that followed after acute dislocation, but with more resistive exercises. This program can also be started early. In addition, a stabilization brace of the patella may help to prevent chronic recurrent subluxation.<ref>Barry P. Boden et al., Patellofemoral instability: evaluation and management, Journal of the American Academy of Orthopaedic Surgeons</ref><br><br> | ||
== Key Research == | == Key Research == | ||
*[http://jbjs.org/content/90/3/463 Acute Patellar Dislocation in Children and Adolescents: A Randomized Clinical Trial]<br> | *[http://jbjs.org/content/90/3/463 Acute Patellar Dislocation in Children and Adolescents: A Randomized Clinical Trial]<br> | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed])<br> == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed])<br> == | ||
Revision as of 16:00, 14 November 2016
Original Editors - Assia Dad as part of the Vrije Universiteit Brussel's Evidence-based Practice project
Top Contributors - Claudia Karina, Julie Plas, Admin, Michelle Lee, Rachael Lowe, Assia Dad, Kim Jackson, 127.0.0.1, Kai A. Sigel, WikiSysop and Niels Cornand
Definition/Description[edit | edit source]
A frequent cause of knee pain and knee disability is patellofemoral instability. Patellofemoral instability can be defined in different ways. One way is when the patient has undergone a traumatic dislocation of the patella. It can also describe a sign on physical examination, signifying the ability of the patella to be translated out of the trochlear groove of the femur in a passive manner. Moreover, patellofemoral instability can be a symptom, when the patient gives a feeling that the knee “gives way’’. This feeling occurs when the patella slips out of the trochlear groove. The relationships between the symptoms, injuries and diseases of the patellofemoral joint are often confusing for the therapist.[[|]][1]
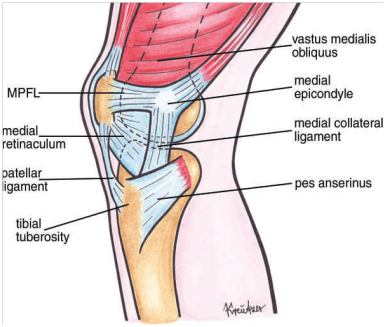
Figure1 Drawing of anatomic structures of the knee (medial view). Anatomic structures obscuring the MPFL have been left [2]
Clinically Relevant Anatomy[edit | edit source]
General anatomy of the patellofemoral joint
Many studies report the importance of the medial patellofemoral ligament (MPFL). The MPFL prevents the patella from translating laterally. The quadriceps is a dynamic stabilizer of the patella.
The patellomeniscal ligament and the medial retinacular fiber are also important medial stabilizers. [3]
Link: http://www.physio-pedia.com/Lateral_Collateral_Ligament_Injury_of_the_Knee
Epidemiology /Etiology[edit | edit source]
- Femoral anteversion
- Genu Valgum
- Patellar dysplasia
- Femoral dysplasia
- Vastus medialis obliquus atrophy
- High Q angle
- Pes planus
- Generalized hyperlaxity
Characteristics/Clinical Presentation[edit | edit source]
Patellofemoral instability may result in pain in and around the anterior aspect of the knee and the patella, this can be aggravated by activities such as up and down the stairs, sports such as running, hopping and jumping, and changing direction. This pain also feel like a dull ache and may be present after an aggravating activity such as sport in the younger population.
Upon fucntional assessment the patient may struggle with control of the patella, resulting in the patella being pull from midline, therefore to assss this you need to observe what is happening to the patella during static and dynamic movements such as squating / lunging. [4]
Differential Diagnosis[edit | edit source]
- Patellar dislocation may take place as a direct traumatic event (acute dislocation of the patella) in a patient with normal patellar alignment. It can also occur in a patient with pre-existing malalignment, especially if there is significant baseline subluxation.
- patellar subluxation: When the patella is transiently or permanently medial or lateral to its normal tracking course, then the patella may articulate abnormally.
Subluxation or lateral translation will involve transient lateral movement of the patella. In general, it is early in knee flexion such that the patient will experience a feeling of pain or instability. This form of patellar subluxation is rather a recurrent dislocation of the patella. It is essential to distinguish between this form of abnormal patellar alignment and tilt.
Types of subluxations:
• Minor Recurrent Subluxation
• Major Recurrent Subluxation
• Permanent Lateral Subluxation
Diagnostic Procedures[edit | edit source]
Patellar instability is normally diagnosed through a comprehensive history of the patient's symptoms and functional objective assessment of the knee. Further scans such as MRI's and Ultrasound imaging can be performed to rule out any strutural defecits.
Outcome Measures[edit | edit source]
There are many outcome measures that can be used with this condition, currently there are no specific reccomendations from COMET therefore it is up to the clinician to clinically reason which outcome measue would be most approprite for their paient. Here are a few:
- Anterior Knee Pain Scale
- Lower Extremity Functional Scale
- Pain Assessment Scales
- Numeric Pain Rating Scale
Examination[edit | edit source]
History:
The first diagnostic step is a detailed history. It is the most important clue for a correct diagnosis.
Physical Examination:
The second diagnostic step is a careful, complete and essential physical examination. The purpose of this examination is to reproduce the symptoms (pain/instability) and to locate the painful zone. The location can indicate which structure is injured, it is truly helpful to compose the diagnosis and to plan the treatment.
Tests:[5] 1) Fairbanks patellar apprehension test:
The test is positive, when there is pain and muscle defensive contraction of lateral patellar dislocation with 20°–30° of knee flexion. The positive test indicates that lateral patellar instability is an important part of the patient’s problem. This may be so positive that the patient pulls the leg back when the therapist approaches the knee with his hand, preventing so any contact, or the patient grabs the therapist’s arm.
--> 100% sensitivity, 88.4% specificity, and overall accuracy of 94.1%[6]
2) Patellar glide test:
This test is used to evaluate the instability. A medial/lateral displacement of the patella greater than or equal to 3 quadrants, with this test, is consistent with incompetent lateral/medial restraints. Lateral patellar instability is more frequent than medial instability.
Physical Therapy Management
[edit | edit source]
Patellofemoral Instability: acute dislocation of the patella[edit | edit source]
Nonoperative treatment:
It is a treatment that consists of immobilization followed by a period of structured rehabilitation. Immobilization is granted for healing of the soft tissues, especially the supporting structures on the medial side of the knee. Today brace treatment with early mobilization has become the norm, instead of the traditional immobilization of 3 to 6 weeks in a cylinder cast.
Most of the time these therapies start with the initial straight-leg raises: Quadriceps setting exercises and three sets of 15 to 20 straight leg raises are done four or five times a day during the acute period. Ice is applied for 20 minutes every 2 to 3 hours to reduce swelling.[7]
It is followed by stationary bicycle for passive and active motion, isotonic and isometric quadriceps strengthening. Between 3 and 8 weeks, the return to full activities was allowed when tenderness weakened and isotonic quadriceps strength was bilateral.
In up to two-third of the knees the results were good to excellent, these results consist of a first-time acute dislocation, compared with only 50% of those with a recurrent dislocation. In general, 73% were satisfied with their knees, but 16% were not and eventually decided to have surgical stabilization.
Those with acute patellar dislocation can expect an extended rehabilitation period before returning to sport, whether immobilized or not.
Patellofemoral Instability: Recurrent Dislocation of the Patella[edit | edit source]
Nonoperative treatment
Surgery is not necessarily needed for patients with patellofemoral malalignment or relaxation of the patella. Adequate results can be achieved with a conservative exercise treatment program. It is very important in the rehabilitation program to strengthen the quadriceps muscle and vastus medialis obliquus (VMO). It’s advised to follow the program which is similar to that followed after acute dislocation, but with more resistive exercises. This program can also be started early. In addition, a stabilization brace of the patella may help to prevent chronic recurrent subluxation.[8]
Key Research[edit | edit source]
Recent Related Research (from Pubmed)
[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1twh4oYFmCRoDmHROTQ3251NjD_yVyT1VCWLzSZT2ngN8DkQnw|charset=UTF-8|short|max=10: Error parsing XML for RSS
References
[edit | edit source]
- ↑ Fulkerson, J.P. et al., Disorders of the patellofemoral joint, USA, Williams &amp; Wilkins, 1997, p.175-187, 199-216, 275-297
- ↑ G. Diederichs et al., 2010, MR Imaging of patellar instability: Injury Patterns and Assessment of Risk Factors, Radiographics
- ↑ J.S. Mulford et al., 2007, Assessment and management of chronic patellofemoral instability, The journal of bone and joint surgery
- ↑ What are the symptoms of Patellofemoral pain? [Accessed 14th November2016] Available from: http://www.arthritisresearchuk.org/arthritis-information/conditions/patellofemoral-pain-syndrome/symptoms.aspx
- ↑ Vicente Sanchis-Alfonso, Anterior Knee Pain and Patellar Instability, Second Edition, 2011, p108-120
- ↑ Christopher S. Ahmad et al., The Moving Patellar Apprehension Test for Lateral Patellar Instability, The American Journal of Sports Medicine
- ↑ Reuven Minkowitz, M.D., Chris Inzerillo, M.D., and Orrin H.Sherman,M.D., Patella Instability, Bulletin of the NYU Hospital for Joint Diseases 2007
- ↑ Barry P. Boden et al., Patellofemoral instability: evaluation and management, Journal of the American Academy of Orthopaedic Surgeons
- DeLee, Jesse, David Drez, and Mark D. Miller. DeLee & Drez's Orthopaedic Sports Medicine Principles and Pratice. St. Louis, MO: Elsevier Science, 2003, p1534-p1572
- [2][3]Vicente Sanchis-Alfonso, Anterior Knee Pain and Patellar Instability, Second Edition, 2011, p108-120
- [4]Reuven Minkowitz, M.D., Chris Inzerillo, M.D., and Orrin H.Sherman,M.D., Patella Instability, Bulletin of the NYU Hospital for Joint Diseases 2007 (level of evidence 2A)
- Barry P. Boden et al., Patellofemoral instability: evaluation and management, Journal of the American Academy of Orthopaedic Surgeons (level of evidence 1C)
- [5]Christopher S. Ahmad et al., The Moving Patellar Apprehension Test for Lateral Patellar Instability, The American Journal of Sports Medicine (Level of evidence 3)