Parkinson's Disease (PD): A Case Study
Abstract[edit | edit source]
This case study is regarding Parkinson's Disease (PD) that is neurodegenerative disorder which causes an impairment in the production of dopamine in the brain(1).The absence of dopamine results in various deficiencies in the motor, physiological, and behavioural state of this population(2). The objective of this case study was to explore the effectiveness of Virtual Reality (VR) on motor function and quality of life in patients living with PD. Recent evidence has shown positive outcomes in motor function, cognition, and mental health(3). The following case illustrates a 66 year old woman who is diagnosed with late-onset stage three idiopathic Parkinson’s Disease. She has been referred to physiotherapy from her neurologist, and has partaken in an intervention in which a multi-faceted exercise program consisting of aerobic, resistance, and stretching movements. After three months of treatment, the patient was reassessed on all outcome measures, and specifically shown improvements in the BERG balance scale, improving her score to 53/56, a eight point increase from her initial score. This indicates that she has decreased her risk of falling. The TUG test was also reassessed and was completed in 13.0 seconds, which is also an improvement that indicates a lower risk of falling. Outcome measures of mini-BEST and dynamic gait index demonstrated no significant changes after interventions were implemented.
Introduction[edit | edit source]
Parkinson’s Disease is a progressive neurodegenerative condition that is caused by the death of dopaminergic neurons in the pars compacta within the midbrain. The Pars compacta is a dopamine producing region located in the substantia nigra of the midbrain(1). Dopamine is a neurotransmitter that is heavily involved in neural regulation of behavioral and physiological functions such as motivation, reward, coordination, balance, neuroendocrine control, and executive function(2). Motor symptoms of PD include uncontrollable tremor, bradykinesia, balance deficit, postural dysfunction, and rigidity(4). Non-motor symptoms include impaired memory, planning, mood (anxiety and depression), speech, smell, and sleep (insomnia) as well as fatigue and difficulty swallowing(4).
The purpose of this case study is to portray the positive effects of VR (Virtual Reality) on motor function and quality of life in patients living with PD. Previous research demonstrates the benefits of simulating external environments within the safety and comfort of a patient’s home on the efficacy of their rehabilitation program(3). Triegaardt et al. completed a meta analysis of ten papers (N = 343) and systematic review of 27 papers (N = 688) to investigate the use of virtual reality (VR) intervention strategies for patients with PD. Although the underlying mechanism that is responsible for how VR is beneficial for patients remains unknown, their findings demonstrate that VR is associated with a variety of improvements to physical and mental health when used in a rehabilitation program. The different domains that Triegaardt et al. examined include stride length, gait speed, balance, coordination, cognitive function, mental health, quality of life and activities of daily living(3). The current literature supports the active approach that incorporates various types of training including balance, endurance, strength, and flexibility. This case study will demonstrate how those training techniques play an important role in improving the motor function and quality of life in those living with PD(5).
Client Characteristics[edit | edit source]
Mrs. Tribianni is a 66 year old female who lives with her husband and dog in a two-storey house. Mrs. Tribianni is an elementary school teacher who teaches science and math. Prior to teaching children, Mrs. Tribianni was a competitive ballet dancer during her twenties. After she retired from dancing, she continued her passion by teaching ballet on the weekends. Approximately a year ago, Mrs. Tribianni noticed that her shoulder muscles were feeling stiffer than before and her hand would shake when she was relaxed. Mrs. Tribianni believed these issues were due to aging, so she did not consult her family physician until she had a fall. Mrs. Tribianni’s family physician referred her to a neurologist who diagnosed her with late-onset, stage 3 (middle stage) idiopathic Parkinson’s Disease. After her diagnosis, Mrs. Tribianni was referred to physiotherapy for balance, gait, and strengthening rehabilitation.
Examination Findings[edit | edit source]
Demographics
Full name: Mrs. Martina Tribianni (She/Her)
D.O.B: July 23, 1956
Sex: Female
Languages spoken: English, Italian
History of present illness
Diagnosis: Late onset stage 3 (middle stage) idiopathic Parkinson’s Disease
Current symptoms:
Rigidity: Patient noticed stiffness in the right side of the body initially, she now claims she feels stiffness on both sides. Bradykinesia: Patient mentions that it takes her longer to walk her dog now
Micrographia: Patient mentions that her handwriting has become smaller.
Tremor: Patient mentions that her shaking hand tends to significantly decrease when performing voluntary movements. However, she mentions it becomes worse when she feels stressed or anxious.
Postural instability: Patient mentions she has had a couple falls while teaching dance to her students. Currently, an assistant is helping her demonstrate dance movements to her students instead.
Fatigue: Patient mentions that as the day progresses, she starts to feel lethargic.
Anosmia: Patient claims she can’t smell spices while she is cooking
Sensory symptoms: Patient mentions she has noticed some aching pain in her lower back
Dysphagia: Patient mentions that her swallowing difficulties has prevented her from eating certain foods due to a fear of choking.
Sleep behaviour: Patient claims she has difficulty falling asleep at night and she sometimes feels drowsy during the day
Past Medical History: Fracture of the 5th metatarsal when she was 15 yrs old due to dance (no complications; fully healed), ankle sprain 5 months ago due to a fall (resolved). Patient had 3 other falls with no significant injuries.
Medications: Dopaminergic therapy (Levodopa/Carbidopa)
Health habits: No history of substance or alcohol abuse. Non-smoker. Patient mentions she drinks wine in social settings, once in a while.
Psychosocial: The patient mentions that she is experiencing feelings of sadness and frustration. Patient claims that her “shaking”, “heavy limbs”, and fear of falling affect her ability to dance. Patient also mentions that her inability to smell different spices while cooking has left her feeling frustrated as cooking with her husband is one of her hobbies.
Social History: Elementary school teacher and dance teacher. Lives with husband and their dog in a two-storey house that has 4 stairs to enter the home, and 10 stairs to reach the second floor. Hobbies include dancing, cooking, going for hikes, and spending time with friends and family.
Clinical Impression[edit | edit source]
Mrs. Tribianni is a 66-year-old female who has been diagnosed with late-onset stage 3 idiopathic PD. Mrs. Tribianni has an overall decrease in strength (3/5 MMT in UE/LE) and slight limitations in bilateral shoulder flexion and hip flexion. Upon observation, Mrs. Tribianni presents with facial masking, dysarthria, a right-sided dominant resting tremor, and moderate kyphosis. With gait, she is showing signs of freezing, difficulty turning, and a reduced arm swing. Outcome measures utilized in the assessment (TUG, BERG balance scale, Mini-BEST test, Dynamic gait index, and Activities-Specific Balance Conditions) indicate that she is at an increased risk of falling. All things considered, she is presenting with the cardinal signs of PD which are bradykinesia, rigidity, and postural instability.
This has taken a considerable toll on Mrs. Tribianni’s psychosocial state. Due to the inability to partake and enjoy her hobbies of cooking and dancing, she has now recently taken on a much more sedentary lifestyle since her PD onset. She feels her arms and legs are too heavy and stiff to partake in her favourite activities such as walking her dog with her husband, dancing to her students, and cooking independently (she is still partaking in these activities but in a modified capacity i.e. breaks during dog walks, assistance with ADL’s from husband, and instructing students rather than demonstrating). As a result, she is experiencing anxiety, frustration, and sadness due to her withdrawal from these activities. Furthermore, given her living situation, she is showing an increase in fatigue in and around her house, especially when climbing up and down the stairs.
Intervention[edit | edit source]
Short term goals
- Increase gait speed by 0.3m/s by the end of 3 weeks of treatment
- Patient will be able to perform a tandem stance for at least 30s with minimal assistance within 4 weeks
- Patient will increase strength in all bilateral shoulder movements to at least a grade 4/5 on the manual muscle testing scale by the end of 4 weeks
- Patient will increase strength in all bilateral hip and knee movements to at least a grade 4/5 on the manual muscle testing scale by the end of 4 weeks
Long term goals
- Patient will be able to stand up and teach for at least 50% of the time within 3 months
- Patient will be able to actively participate in playful activities with her dog in the next 4 months
Strengthening Interventions
- Strengthening exercises are very important for our patient as they will challenge her muscles and help gain back strength. Our patient has experienced weakness post PD onset, and it is therefore crucial for our team to integrate a strengthening program to ensure that we prevent muscle atrophy. We will begin with light functional exercises and eventually progress these exercises by increasing resistance. Refer to figure 1 for the week 1 strengthening program, the team will progress these strengthening exercises once the patient is comfortably performing them.
Stretching Interventions
- Stretching exercises are also extremely important to integrate into our patient’s treatment program as it will help increase her flexibility. Our patient presents with rigidity, so it is particularly important that we manage this and limit the muscle tone that she is experiencing by stretching out different muscle groups. Refer to figure 2 for the week 1 stretching program, the team will progress these stretches once the patient is comfortably performing them.
Balance interventions
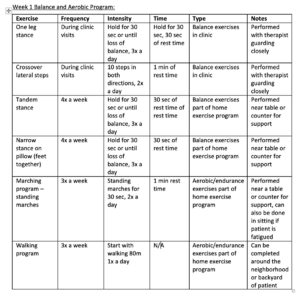
- Patient has trouble with a decreased base of support and scored lower than 52 on the Berg Balance scale, therefore exercises promoting balance and changing base of supports will help decrease risk of falls and increase confidence in themselves. In clinic, patient was given the following exercises and parameters; one leg stance with therapist guarding. Patient held this stance for 30 sec for 3 sets with the therapist nearby guarding. The other exercises done in clinic included crossover lateral steps with therapist guarding closely. Patient completed this 10 times in both directions for 2 sets.
- The home exercises program given to the patient included a tandem stance as well as a narrow stance on a pillow. The tandem stance was held for 30sec for 3 sets, 4x a week. The narrow stance on a pillow was also held for 30sec for 3 sets, 4x a week.
Aerobic/Endurance interventions
- Patient is only able to walk short distances before fatiguing and spends most of her teaching time sitting down. Therefore, providing endurance and aerobic training to the patient will help her be more functional and able to stand and walk further therefore targeting patient goals.
- As part of the home exercise program, the patient was given a marching and walking program. In the marching program the patient can perform in both sitting and standing depending on how patient feels that specific day. The goal is to complete these marches for 30 sec for 2 sets, 3x a week. This can also be done near a table or counter for support and balance purposes. The walking program given also progresses weekly, starting at 80m and progressing about 20m every week. Patient will perform both the marching and walking programs 3x a week.
Outcome[edit | edit source]
Mrs.Tribbiani was reassessed by our team 3 months after her initial visit. The BERG balance Scale was administered once again and Mrs.Tribbiani improved her score by 7 from her initial assessment. She has now scored a 52/56 indicating that she is at a decreased risk of falling. Specifically, she has shown improvement with maintaining balance with a decreased BoS. She could now effectively maintain balance with her feet close together and when in tandem stance. We are extremely pleased with the progress made with regards to her balance and we will continue to include balance interventions in her treatment plan going forward. The TUG test was also administered again and Mrs.Tribbiani completed this test in 13.0 seconds. This indicates that she is at a lower risk of falling and has greatly improved her balance and motor skills.
The MiniBEST was administered again and Mrs. Tribbiani’s score improved to a score of 73%. This score is above the threshold of 69%, meaning the risk of falling has significantly decreased. This increase in score indicates that Mrs.Tribbiani has improved her coordination and is more efficient with regards to her movements. In regards to the Dynamic gait index, Mrs. Tribbiani’s score increased to a 21/24. This again was above the threshold score of 19, indicating that she has a significantly decreased chance of falling and has increased confidence when ambulating. The patient is more confident in themselves and moves much more smoothly when walking or transitioning from sit to stand as well. Overall, Mrs. Tribbiani has shown significant improvements in the past 3 months.
The MiniBEST was administered again and Mrs. Tribbiani’s score improved to a score of 73%. This score is above the threshold of 69%, meaning the risk of falling has significantly decreased. This increase in score indicates that Mrs.Tribbiani has improved her coordination and is more efficient with regards to her movements. In regards to the Dynamic gait index, Mrs. Tribbiani’s score increased to a 21/24. This again was above the threshold score of 19, indicating that she has a significantly decreased chance of falling and has increased confidence when ambulating. The patient is more confident in themselves and moves much more smoothly when walking or transitioning from sit to stand as well. Overall, Mrs. Tribbiani has shown significant improvements in the past 3 months.
Objectively, an increase in ROM was observed both passively and actively. Both shoulder flexion and hip flexion increased bilaterally, and this is greatly due to the stretching and ROM exercises that Mrs. Tribbiani has been performing over the past 3 months of treatment. Her passive ROM felt less resisted and end-range was increased for all movements. The patient’s overall strength also increased as seen in her MMT scores. Mrs. Tribbiani’s upper extremity muscle groups increased to at least a 4/5, and this increase in strength can be attributed to the strengthening and endurance program designed by the therapist. The patient’s lower extremity muscle groups increased to a 4+/5, and she was able to walk over 250m without fatiguing. Mrs. Tribbiani seemed to enjoy the walking and marching programs and was keen on continuing the program to improve.
Discussion[edit | edit source]
Self-Study Questions[edit | edit source]
1) What are the 3 cardinal signs of someone who is diagnosed with Parkinson's Disease?
- A) Spasticity, Bradykinesia, Facial Masking
- B) Rigidty, Tremor, Bradykinesia
- C) Tremor, Freezing gait, Rigidity
- D) Shuffling gait, Tremor, Rigidity
2) What is the reasoning for a treatment plan that includes a strengthening program for someone who is diagnosed with Parkinson's Disease?
- A) Strengthening will calm down the central and peripheral nervous system thus reducing the resting tone of the muscle
- B) Strengthening will mitigate the imminent muscle atrophy
- C) Strengthening maintains the overall fitness of Parkinson's Disease
- D) None of the above
3) The effectiveness of Virtual Reality (VR) in treatment for Parkinson's Disease is:
- A) Virtual reality allows the patient to use imagery, allowing patients to envision how their functional capabilities would be if they were not diagnosed with PD
- B)Virtual reality provides patients with cognitive and motor experiences that mimic real world situations by incorporating different senses such as vision, audition, and tactile touch.
- C)Virtual reality is only effective when it is supplemented with passive therapies, and detrimental when supplemented with active therapies
- D) Virtual reality is not effective for the treatment of Parkinson's disease.