Palmaris Longus
Original Editor -
Top Contributors - Mudra Shah, Mandeepa Kumawat, Admin, Nikhil Benhur Abburi and Manisha Shrestha
Description[edit | edit source]
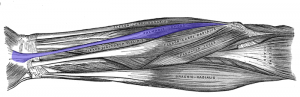
The Palmaris longus (PL) muscle is a long, slender muscle which is usually present in the volar compartment of the forearm, interposed between the Flexor Carpi Ulnaris and the Flexor Carpi Radialis muscles.
However, it has been accepted as a vestigial muscle since studies have shown that almost 30% of the population could be lacking this muscle either in one forearm (unilateral) or both the forearms (bilateral) but the percentage can always vary. The peculiarity associated with this muscle is not merely its presence or absence, but it's high degree of anatomical variations even when present.
Apart from its anatomical anomalies, there are other categories of variations of the Palmaris Longus muscle in terms of its prevalence amongst different ethnicities, it's absence being more common in women and bilateral as well as the higher occurrence on the left upper limb when unilateral[1].
Anatomy[edit | edit source]
Origin[2][edit | edit source]
Medial epicondyle of the Humerus via the common flexor tendon
Insertion[2][edit | edit source]
Palmar Aponeurosis and Flexor Retinaculum at the wrist joint
Nerve Supply[2][edit | edit source]
Arterial supply[3][edit | edit source]
Ulnar Artery
Function[edit | edit source]
- Palmaris longus synergistically works with the long flexors of the forearm to bring about flexion at the wrist joint and small joints of the hand.
- Apart from this, the muscle also helps in tightening the palmar aponeurosis.
Clinical tests to determine the presence of the muscle[edit | edit source]
Over the years, several clinical tests have been developed by practitioners from around the world to accurately detect the Palmaris Longus muscle. These tests merely rely upon certain positions of the wrist and hand in order to put the muscle in a state of tension so that it's tendon is both visible and palpable. The validity and reliability of the tests, however, show variations amongst each other[4].
1. Standard Test - Schaeffer's Test[4][edit | edit source]
- The first test developed in 1909
- Involves maintaining the forearm at 90 degrees first followed by moving the thumb in opposition towards the little finger with the wrist partially flexed.
2. Thompson's Test[4][edit | edit source]
- Maneuver involves first making a fist with the testing hand, followed by wrist flexion against the resistance with the thumb flexed over the other digits.
3. Mishra's Test[4][edit | edit source]
- Involves passive hyperextension of the Metacarpophalangeal Joints along with mild active wrist flexion.
4. Gangata's Test[4][edit | edit source]
- The initial testing position is the thumb in abduction. The subject is then asked to resist both thumb abduction and wrist flexion.
5. "Two Finger Sign" - Pushpakumar's Test[4][edit | edit source]
- The subjects are made to completely extend the 2nd and 3rd digits, flex the 4th and 5th digits with the first digit fully opposed and flexed.
6. "Four Finger Sign"[4][edit | edit source]
- Combines forced anteduction and pronation of the thumb at the first MCP with full extension of the second to fifth digits.
Clinical Significance[edit | edit source]
Compression neuropathies at the wrist are commonly encountered conditions in the clinical practice which involve either the Median nerve or the Ulnar nerve. In case of median nerve neuropathies, most of the documented cases have no external cause to be attributed but there have been cases where the etiological factor has been the presence of hypertrophied/anomalous muscles. There are three muscles which have been documented: the Palmaris Longus, the first (or second) Lumbrical and the Superficial Flexor of the 1st digit. In case of ulnar nerve neuropathies, idiopathic ulnar tunnel syndrome is rare and extrinsic causes have been identified. Anomalous muscles include Palmaris Longus, Abductor Digits Minimi and Flexor Carpi Ulnaris. In both Median and Ulnar nerve neuropathies, Palmaris longus is seen to be a common contributor to the pathological process[7].
Also, the Palmaris Longus tendon is of great importance for surgeons in particular, as it is widely used as tendon graft especially for upper limb tendon repair and tendon transfer surgeries.
References[edit | edit source]
- ↑ Sebastin SJ, Lim AY, Wong H. Clinical assessment of absence of the palmaris longus and its association with other anatomical anomalies-a Chinese population study. Annals-academy of Medicine Singapore. 2006 Apr 1;35(4):249.
- ↑ 2.0 2.1 2.2 Snell RS. Clinical Anatomy By Regions. 9th edition. Philadelphia: Lippincott Williams & Wilkins; 2012.
- ↑ Derek Moore. Palmaris Longus. Available from: https://www.orthobullets.com/anatomy/10023/palmaris-longus [Accessed: 12 June 2018]
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Kigera JW, Mukwaya S. Clinical Assessment of the Palmaris Longus–Accuracy of common tests. Annals of African Surgery. 2012;9(2).
- ↑ Schaeffer's Test for Palmaris Longus (CR) Available from https://www.youtube.com/watch?v=CXdSruxBM2g [last accessed 16/06/2018]
- ↑ Thompson's Test for Palmaris Longus (CR) Available from https://www.youtube.com/watch?v=oZXwD9i0bcQ [last accessed 16/06/2018]
- ↑ De Smet L. Median and ulnar nerve compression at the wrist caused by anomalous muscles. Acta orthopaedica belgica. 2002 Dec 1;68(5):431-8.