Overview of Global Health: Difference between revisions
No edit summary |
No edit summary |
||
| Line 48: | Line 48: | ||
* '''Economics''': Neoliberalism has affected healthcare and for-profit healthcare around the world, creating a significant wealth gap in many countries. In terms of rehabilitation and healthcare services, this gap affects who can access appropriate services.<ref name=":6" /> | * '''Economics''': Neoliberalism has affected healthcare and for-profit healthcare around the world, creating a significant wealth gap in many countries. In terms of rehabilitation and healthcare services, this gap affects who can access appropriate services.<ref name=":6" /> | ||
* '''Food''': It is important to understand the global food system and how it affects our food supply, food sovereignty and nutrition value. Regarding rehabilitation and healthcare, we must consider that food is our body's source of fuel and that where/how we get food influences our mental health and impacts non-communicable diseases.<ref name=":6" /> | * '''Food''': It is important to understand the global food system and how it affects our food supply, food sovereignty and nutrition value. Regarding rehabilitation and healthcare, we must consider that food is our body's source of fuel and that where/how we get food influences our mental health and impacts non-communicable diseases.<ref name=":6" /> | ||
* '''Climate and the environment''': | * '''Climate and the environment''': With climate change, we must consider how heat exposure and increasing temperatures influence physical activity, manual work, etc.<ref name=":6" /> It is also important to note that a various factors including climate change, urbanisation, the migration and trade of animals, travel and tourism, etc. have all had an impact on the development, re-emergence and spread of zoonoses (i.e. a disease / infection that is transmitted from vertebrate animals to humans or humans to animals).<ref>Rahman MT, Sobur MA, Islam MS, Ievy S, Hossain MJ, El Zowalaty ME, et al. [https://www.mdpi.com/2076-2607/8/9/1405 Zoonotic diseases: etiology, impact, and control. Microorganisms]. 2020 Sep 12;8(9):1405.</ref> A number of factors have been identifed as triggers for the development of zoonotic diseases, including changes in: | ||
** human and animal behaviour. | |||
** habitat | |||
** ecology | |||
** vector biology | |||
** pathogen adaptability | |||
** change in farm practices | |||
** livestock production systems | |||
** food safety | |||
** urbanisation | |||
** deforestation | |||
** climate change | |||
* '''One Health''':<ref name=":5">Mackenzie JS, Jeggo M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6630404/ The One Health approach-why is it so important?] Trop Med Infect Dis. 2019 May 31;4(2):88.</ref> This framework considers the connected system between animal, environment, and human health.<ref name=":6" /> | * '''One Health''':<ref name=":5">Mackenzie JS, Jeggo M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6630404/ The One Health approach-why is it so important?] Trop Med Infect Dis. 2019 May 31;4(2):88.</ref> This framework considers the connected system between animal, environment, and human health.<ref name=":6" /> | ||
** The concept of One Health has been around for at least 200 years - initially, it was known as One Medicine, then One World, One Health and now One Health.<ref name=":5" /> | ** The concept of One Health has been around for at least 200 years - initially, it was known as One Medicine, then One World, One Health and now One Health.<ref name=":5" /> | ||
Revision as of 23:34, 4 September 2023
Top Contributors - Jess Bell, Robin Tacchetti and Kim Jackson
Introduction[edit | edit source]
Global health is a broad term. Global health intends "to promote health and prevent and treat diseases for all people in all countries across the globe".[1] It transcends geographical, national and cultural boundaries by targeting populations in all countries.[1] A key goal of global health is to protect the world's population from health threats while delivering cost-effective services.[2] However, as will be discussed in this page, there is no universally accepted definition of global health,[3][4] and many interconnected systems must be considered when attempting to understand health and global health.
History of Global Health[edit | edit source]
The Canadian Institutes of Health Research (CIHR)'s Framework for Action on Global Health Research[5] outlines how our concept of global health has changed over time.
- Initially, we had what could be termed Global Health 1.0 or "tropical medicine". This area of health was very much connected with the legacy of colonialism and imperialism.[6] It was conceived as "Protection of colonial representatives from tropical diseases".[5]
- This concept morphed and changed into what has been termed Global Health 2.0. In this model, the focus was on wealthier countries helping those with less.[5]
- Finally, we currently have what is termed Global Health 3.0 where there is "Collective action to address shared risks and responsibilities".[6]
To read more about the framework outlined by the CIHR, please see: Global Health 3.0. CIHR's Framework for Action on Global Health Research 2021-2026.[5]
To find out more about global health in general, please read:
- Global Health – emergence, hegemonic trends and biomedical reductionism[7]
- Dismantling and reimagining global health education[8]
Defining Global Health[edit | edit source]
In recent years, there has been extensive debate on how we define global health.[3] In 2009, Koplan et al.[9] attempted to create a common definition for global health, distinct from the related areas of public health and international health.[3]
- According to Koplan et al.,[9] the modern concept of public health developed in the mid-19th century in England, Europe and the United States "as part of both social reform movements and the growth of biological and medical knowledge (especially causation and management of infectious disease)"[9]
- International health can be traced back to "colonial roots in hygiene and tropical medicine (TM) through to the mid-20th century with its geographic focus on developing countries."[3]
In a recent systematic review, Salm et al.[3] explored the current definitions for global health and attempted to determine if a "common conceptualisation has been established". In their review, they identified the following themes:[3]
- Global health can be considered "a multiplex approach to worldwide health improvement taught and pursued through research institutes"[3]
- It is a domain of research, healthcare and education
- It is multifaceted ("disciplinary, sectoral, cultural, national")
- Global health can be considered an "ethical initiative that is guided by justice principles"[3]
- It has its roots in values like equity and social justice
- Global health can be considered "a form of governance that yields national, international, transnational and supranational influence through political decision-making, problem identification, the allocation and exchange of resources across borders"[3]
- It is a political field that includes power relations at multiple scales
- It is determined by globalisation and international interdependence
- Issues related to global health cross national borders
- It is problem-oriented
- Global health has many meanings with "historical antecendents and an emergent future"[3]
- It is "dis/similar" to public health, international health and tropical medicine
- The definition for global health remains vague
For more information, please read: Defining global health: findings from a systematic review and thematic analysis of the literature.[3]
Interconnected Systems[edit | edit source]
When considering health and global health, we must also explore other interconnected systems.
- Economics: Neoliberalism has affected healthcare and for-profit healthcare around the world, creating a significant wealth gap in many countries. In terms of rehabilitation and healthcare services, this gap affects who can access appropriate services.[6]
- Food: It is important to understand the global food system and how it affects our food supply, food sovereignty and nutrition value. Regarding rehabilitation and healthcare, we must consider that food is our body's source of fuel and that where/how we get food influences our mental health and impacts non-communicable diseases.[6]
- Climate and the environment: With climate change, we must consider how heat exposure and increasing temperatures influence physical activity, manual work, etc.[6] It is also important to note that a various factors including climate change, urbanisation, the migration and trade of animals, travel and tourism, etc. have all had an impact on the development, re-emergence and spread of zoonoses (i.e. a disease / infection that is transmitted from vertebrate animals to humans or humans to animals).[10] A number of factors have been identifed as triggers for the development of zoonotic diseases, including changes in:
- human and animal behaviour.
- habitat
- ecology
- vector biology
- pathogen adaptability
- change in farm practices
- livestock production systems
- food safety
- urbanisation
- deforestation
- climate change
- One Health:[11] This framework considers the connected system between animal, environment, and human health.[6]
- The concept of One Health has been around for at least 200 years - initially, it was known as One Medicine, then One World, One Health and now One Health.[11]
- Again, there is no single definition for One Health. Most commonly, it is defined as: "a collaborative, multisectoral, and transdisciplinary approach—working at the local, regional, national, and global levels—with the goal of achieving optimal health outcomes recognizing the interconnection between people, animals, plants, and their shared environment".[11]
- One Health considers "consequences, responses, and actions at the animal–human–ecosystems interfaces",[11] including:
- the increased burden of disease (particularly in resource-poor settings) due to emerging and endemic zoonoses
- antimicrobial resistance in humans, animals, or the environment
- food safety
- However, it is important to note that One Health also considers various disciplines and domains, environmental and ecosystem health, social sciences, ecology, wildlife, use of land and biodiversity.[11]
- Factors at a community level: We must understand how certain social constructs (e.g. gender, class, race) impact an individual's agency, empowerment and advocacy when obtaining healthcare.
Determinants of Health[edit | edit source]
The many interconnected factors that impact health and health outcomes are referred to as determinants of health. Examples of determinants of health can include genetics, behaviour, environment and physical influences, medical care, social and structural determinants.
Social determinants of health (SDH) are the circumstances in which we are born, develop, live, earn, and age. SDH include economic conditions, housing, nutrition, the environment, transportation, and education.[12]
WHO defines social determinants of health as “complex, integrated, and overlapping social structures and economic systems that include the social environment, physical environment, and health services; structural and societal factors that are responsible for most health inequities. Social determinants of health are shaped by the distribution of money, power and resources at global, national, and local levels, which are themselves influenced by policy choices."
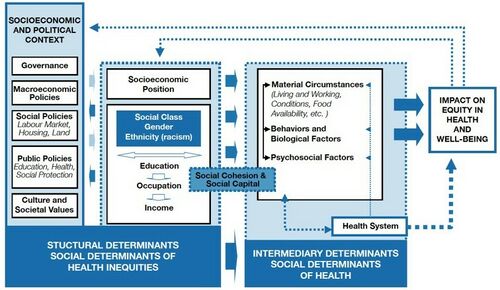
Structural determinants are upstream root causal factors that influence downstream determinants and health conditions. Examples include, but are not limited to, power, education, economic system, land policies and social positions.[6] The WHO Conceptual Framework illustrates the relationship between structural and intermediary determinants of health and their impact on health equity (see Figure 1).
Given the ongoing COVID-19 pandemic, recent social movement and the increasing discussion on diversity, equity and inclusion initiatives across all sectors, it is vital to understand how racism, xenophobia and discrimination are structural determinants of health.[6] The Lancet recently published a series of papers illustrating how these determinants intersect with systems of power, such as politics, education, and scientific knowledge production, that continue to impact health equity across minority groups. It is important as rehabilitation professionals to recognise and examine how these social constructs influence many levels of our healthcare system, spanning leadership research, biases and patient contact.
See these articles here:
- Racism, xenophobia, discrimination, and the determination of health
- Racism, xenophobia, and discrimination: mapping pathways to health outcomes
- Intersectional insights into racism and health: not just a question of identity
- Confronting the consequences of racism, xenophobia, and discrimination on health and health-care systems
Concluding Points[edit | edit source]
- Global health must consider more than just medical care - it must also address "other underlying drivers of health, social and political determinants, and non-health sectoral issues."[4]
- If we are to improve outcomes and achieve equity in health, global health must also consider culture, human behaviour, governance, law, politics, various regulations, and institutional frameworks.[4]
- Power dynamics in global health have tended to undervalue research from low- and middle-income countries.[4]
For more information on power asymmetries in global health, please see:
- Who is a global health expert?[4]
- Addressing power asymmetries in global health: Imperatives in the wake of the COVID-19 pandemic[13]
References[edit | edit source]
- ↑ 1.0 1.1 Chen X, Li H, Lucero-Prisno DE, Abdullah AS, Huang J, Laurence C, Liang X, Ma Z, Mao Z, Ren R, Wu S. What is global health? Key concepts and clarification of misperceptions. Global health research and policy. 2020 Dec;5(1):1-8.
- ↑ De Cock KM, Simone PM, Davison V, Slutsker L. The new global health. Emerging Infectious Diseases. 2013 Aug;19(8):1192.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 Salm M, Ali M, Minihane M, Conrad P. Defining global health: findings from a systematic review and thematic analysis of the literature. BMJ Glob Health. 2021 Jun;6(6):e005292.
- ↑ 4.0 4.1 4.2 4.3 4.4 Ojiako CP, Weekes-Richemond L, Dubula-Majola V, Wangari MC. Who is a global health expert? PLOS Glob Public Health. 2023 Aug 17;3(8):e0002269.
- ↑ 5.0 5.1 5.2 5.3 Canadian Institutes of Health Research, Instituts de Recherche en Santé du Canada. Global Health 3.0. 2021-2026. Framework for Action on Global Health Research. 2021. Available from: https://cihr-irsc.gc.ca/e/52503.html [Accessed 1 September 2023].
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 Lai D. Global Health for Rehabilitation Professionals Course. Plus, 2023.
- ↑ Holst J. Global Health - emergence, hegemonic trends and biomedical reductionism. Global Health. 2020 May 6;16(1):42.
- ↑ Gichane MW, Wallace DD. Dismantling and reimagining global health education. Glob Health Action. 2022 Dec 31;15(1):2131967.
- ↑ 9.0 9.1 9.2 Koplan JP, Bond TC, Merson MH, Reddy KS, Rodriguez MH, Sewankambo NK, et al. Towards a common definition of global health. Lancet. 2009 Jun 6;373(9679):1993-5.
- ↑ Rahman MT, Sobur MA, Islam MS, Ievy S, Hossain MJ, El Zowalaty ME, et al. Zoonotic diseases: etiology, impact, and control. Microorganisms. 2020 Sep 12;8(9):1405.
- ↑ 11.0 11.1 11.2 11.3 11.4 Mackenzie JS, Jeggo M. The One Health approach-why is it so important? Trop Med Infect Dis. 2019 May 31;4(2):88.
- ↑ World Health Organization. Social Determinants of Health. Available from: https://www.who.int/health-topics/social-determinants-of-health (last accessed 1 September 2023).
- ↑ Abimbola S, Asthana S, Montenegro C, Guinto RR, Jumbam DT, Louskieter L, et al. Addressing power asymmetries in global health: Imperatives in the wake of the COVID-19 pandemic. PLoS Med. 2021 Apr 22;18(4):e1003604.