Manual Therapy Techniques For The Lumbar Spine: Difference between revisions
No edit summary |
mNo edit summary |
||
| (43 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors ''' - [[User:Jenny Arnatt|Jenny Arnatt]], [[User:Tabitha Eddleston|Tabitha Eddleston]], [[User:Victoria Jovcic|Victoria Jovcic]], [[User:Lizzie Wakeham|Lizzie Wakeham]] | '''Original Editors ''' - [[User:Jenny Arnatt|Jenny Arnatt]], [[User:Tabitha Eddleston|Tabitha Eddleston]], [[User:Victoria Jovcic|Victoria Jovcic]], [[User:Lizzie Wakeham|Lizzie Wakeham]] as part of the [[Nottingham University Spinal Rehabilitation Project]]<br> | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
In principle, any of the structures within the lumbar spine that receive innervation from the nervous system can be a source of back pain. Thus back pain can arise from any of the ligaments, muscles, fascia, joints or discs of the Lumbar Spine. Read more information on [[Low Back Pain|low back pain]]. | |||
==Mobilisations== | |||
<span style="line-height: 1.5em;">Mobilisations primarily consist of passive movements which can be classified as physiological or accessory </span><ref>Porter, S., (2005). Dictionary of Physiotherapy. London. Elsevier.</ref><span style="line-height: 1.5em;">. The purpose is to provide short term pain relief and to restore pain-free, functional movements by achieving full range at the joint </span><ref>Maitland, G., Hengeveld. E., Banks, K. and English, K., (2005). Maitland's Vertebral Manipulation. 7th Edition. London. Elsevier.</ref><span style="line-height: 1.5em;">.</span> | |||
Joint mobilisation is a treatment technique which can be used to manage musculoskeletal dysfunction <ref>Hertling D., and Kessler, R., (1996) Management of Common Musculoskeletal Disorders. Baltimore: Lippincott, Williams & Wilkins.</ref>, by restoring the motion in the respective joint <ref>Randall, T., Portney, L., and Harris, BA., (1992). Effects of Joint Mobilization on Joint Stiffness and Active Motion of the Metacarpal-Phalangeal Joint. Journal of Orthopaedic & Sports Physical Therapy. Vol 16, (1) 30-36.</ref>. The techniques are performed by physiotherapists and fall under the category of manual therapy. Spinal mobilisation is described in terms of improving mobility in areas of the spine that are restricted <ref name="Korr (1977)">Korr, IM., (1977). The neurobiologic mechanisms in manipulative therapy. New York, Plenum Press.</ref>. Such restriction may be found in joints, connective tissues or muscles. By removing the restriction by mobilisation the source of pain is reduced and the patient experiences symptomatic relief. This results in gentle mobilisations being used for pain relief while more forceful, deeper mobilisations are effective for decreasing joint stiffness. <ref name="Maitland(1986)">Maitland, GD., (1986). Vertebral manipulation. 5th edition. Sydney, Butterworths.</ref>. | |||
==Effects and Mechanisms== | |||
Research has shown that mobilisation used as therapy can produce significant mechanical and neurophysiological effects <ref>Wright, A., (1995). Hypoalgesia post-manipulative therapy: a review of a potential neurophysiological mechanism. Manual Therapy, Vol 1, 11-16</ref> <ref>Bialosky, J., Bishop, M., Price, D., Robinson, M., and George, S., (2009). The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Therapy, Vol 14, 531-538.</ref> <ref>Gross, A., Miller, J.,D'Sylva, J., Burnie, S., Goldsmith, C., Graham, N., Haines, T., Bronfort, G., and Hoving J., (2010). Manipulation or Mobilisation for Neck Pain. Cochrane Database of Systematic Reviews, Issue 1, 1-90</ref> <ref>Zusman, M., (2011). Mechanism of mobilization. Physical Therapy Reviews, Vol 16, (4) 233-236.</ref>. The explanations of these effects - the mechanism of mobilisation - is still relatively unknown, especially in regards to the spine, and is subject to further research <ref>Krouwel, O., Hebron, C., and Willet, E., (2010). An investigation into the potential hypoalgesic effects of different amplitudes of PA mobilisation on the lumbar spine as measured by pressure pain thresholds (PPT). Manual Therapy, Vol 15, 7-12</ref>.<br>However, several theories have been established in accordance with the effects seen, including the effects of pain relief, increasing range of motion and the influence on the autonomic nervous system. | |||
=== Pain Relief === | |||
Mobilisations offer pain relief through hypoalgesia - decreasing the nervous system's sensitivity to painful stimuli. There are various potential mechanisms of this neurophysiological effect: | |||
# Pain gating<br>Pain gating refers to the theory that stimulation of the mechano-receptive peripheral afferent nerves in the muscles produce sensory input that interferes with nociceptive impulses at the spinal cord <ref>Pickar, JG., and Wheeler, JD., (2001). Response of muscle proprioceptors to spinal manipulative like loads in the anesthetized cat. Journal of Manipulative and Physiological Therapeutics, Vol 24, 2–11.</ref>. The input from the larger sensory nerves inhibits the transmission of pain through the smaller nociceptive nerves to the brain, leading to a pain-relieving result <ref>BJA., (2002). Editorial I - Gate Control Theory of pain stands the test of time. British Journal of Anaesthesia, Vol 88 (6) 755-757.</ref>. Therefore, the processes of stimulating mechanoreceptors via mobilisation produce short term pain relief through the mechanism of pain gating <ref>Zusman, M., (1986). Spinal Manipulative Therapy: Review of Some Proposed Mechanisms, and a New Hypothesis. The Australian Journal of Physiotherapy, Vol 32 (2) 89-99</ref>. However, the pain gate theory only explains the pain-relieving effect during the mobilisation, not any long term effects post-treatment. Therefore it is hypothesised that any longer-term pain-relieving effects are mediated by higher brain mechanisms <ref>Krouwel, O., Hebron, C., and Willet, E., (2010). An investigation into the potential hypoalgesic effects of different amplitudes of PA mobilisation on the lumbar spine as measured by pressure pain thresholds (PPT). Manual Therapy, Vol 15, 7-12</ref> | |||
# Descending mechanisms and supraspinal regions<br>Research has shown that mobilisation leads to activation of pain inhibitory pathways that originate in the midbrain and travel down the spinal cord - the descending pathways <ref>Krouwel, O., Hebron, C., and Willet, E., (2010). An investigation into the potential hypoalgesic effects of different amplitudes of PA mobilisation on the lumbar spine as measured by pressure pain thresholds (PPT). Manual Therapy, Vol 15, 7-12</ref> <ref>Zusman, M., (2011). Mechanism of mobilization. Physical Therapy Reviews, Vol 16 (4) 233-236.</ref> <ref>Grayson, J., Barton, T., Cabot, P., and Souvlis, T., (2012), Spinal manual therapy produces rapid onset analgesia in a rodent model. Manual Therapy, Vol 17, 292-297.</ref>. The pathway stimulation works to provide pain relief by suppression of pain through this inhibitory mechanism. <br>In addition to this these descending pathways, research has shown a trend where regions of the brain responsible for central pain processing are suppressed during mobilisation <ref>Bialosky, J., Bishop, M., Price, D., Robinson, M., and George, S., (2009). The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Therapy, Vol 14, 531-538.</ref>. | |||
# Adaptation<br>It has been hypothesised that mobilisation promotes adaptations of the nervous system <ref>Refshauge, K., and Gass, E., (2004). Musculoskeletal Physiotherapy: clinical science and evidence-based practice. 2nd Edition. Oxford. Butterworth Heinemann.</ref> with a decrease in the level of neural input from the painful site. Research also suggests that mobilisations increase the pain threshold levels - relative hypoalgesia <ref>Wright, A., (1995). Hypoalgesia post-manipulative therapy: a review of a potential neurophysiological mechanism. Manual Therapy, Vol 1, 11-16</ref>. It has been suggested that this could be due to electrochemical changes in the regulation of threshold potential <ref>Zusman, M., (1986). Spinal Manipulative Therapy: Review of Some Proposed Mechanisms, and a New Hypothesis. The Australian Journal of Physiotherapy, Vol 32 (2) 89-99</ref>. | |||
===== | === Increasing Range of Motion === | ||
Mobilisations are often used with the objective to increase the range of motion of the joint through stretching of fibrous tissue <ref>Refshauge, K., and Gass, E., (2004). Musculoskeletal Physiotherapy: clinical science and evidence-based practice. 2nd Edition. Oxford. Butterworth Heinemann.</ref>. This stretching may cause the tissue to 'creep'. The phenomenon of creep relates to the ability of tissues to change shape over time as a constant load is applied. The creep deformation is not permanent and, once the load is removed, the tissue will slowly resume its original length <ref>Threlkeld, A., (1992). The Effects of Manual Therapy on Connective Tissue. Physical Therapy, Vol 72 (12) 893-902.</ref>. However, in the short term, this mechanical effect of mobilisation enables an increase in range of motion at the joint. | |||
< | === Influence on Autonomic Nervous System === | ||
Mobilisation has been found to influence sympathetic activity, affecting heart rate, blood pressure <ref>Zusman, M., (2011). Mechanism of mobilization. Physical Therapy Reviews, Vol 16 (4) 233-236.</ref> and respiratory rate <ref>Wright, A., (1995). Hypoalgesia post-manipulative therapy: a review of a potential neurophysiological mechanism. Manual Therapy, Vol 1, 11-16</ref>. These sympathetic responses could possibly be linked to another evidenced effect of mobilisation - changes in blood component levels. Teodorczyk-Injeyan et al (2006) found that mobilisation effected the levels of blood components, with a reduction in inflammatory proteins. Therefore it was suggested that mobilisation could be a potential therapeutic modality to reduce inflammatory response - working as an anti-inflammatory mechanism, though the exact explanation for this process is unknown <ref>Teodorczyk-Injeyan, J., Injeyan, H., and Ruegg, R,. (2006). Spinal manipulative therapy reduces inflammatory cytokines but not substance P production in normal subjects. Journal of Manipulative and Physiological Therapeutics, Vol 29, 14–21</ref>. | |||
Bialosky et al (2009)<ref>Bialosky, J., Bishop, M., Price, D., Robinson, M., and George, S., (2009). The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Therapy, Vol 14, 531-538.</ref> suggested that the mechanical and neurophysiological effects explored here are interlinked. They proposed that a mechanical force initiates a chain of neurological responses, which would then produce the outcomes associated with manual therapy.<br>This proposal was illustrated in their model of the mechanisms of manual therapy<ref>Bialosky, J., Bishop, M., Price, D., Robinson, M., and George, S., (2009). The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Therapy, Vol 14, 531-538.</ref>. | |||
< | The effects of mobilisation and the mechanisms responsible are not fully understood and more research is needed to provide evidence for the theories discussed. It is also important to note that variables such as the placebo effect and psychological factors may also pertain to the effects seen <ref>Ernst, E., (2000). Does spinal manipulation have specific treatment effects? Family Practice, Vol 17, 554–556.</ref>. <u></u><u></u><u></u> | ||
== | === Effects of Mobilisation on Stiffness and Pain === | ||
Mobilisations involving pressure onto the vertebra can be used to increase joint range of motion, and also to produce and analgesic effect. | |||
Manual therapy and mobilisations can be used to treat 5 symptom groups:<ref name="Maitland et al, 2005" /><ref name="Fabio, 1992">Fabio R. (1992) Efficacy of manual therapy. Physical Therapy Vol 72, Issue 12</ref> | |||
*Pain | |||
*Stiffness | |||
*Pain associated with stiffness | |||
*Pain | |||
*Stiffness | |||
*Pain associated with stiffness | |||
*Momentary jabs of pain | *Momentary jabs of pain | ||
*Disorders directly related to a specific diagnosis | *Disorders directly related to a specific diagnosis | ||
< | === Stiffness === | ||
'''For patients whose joint stiffness is limiting normal function'''.<ref name="Maitland et al. 2005" /> First, assess the patient's movement using physiological movements, select the movement that has limited ROM and needs to be stretched. Then accessory movements can be used. Pressure applied through the thumb or pisiform against the vertebrae in the direction of the movement that is stiff. | |||
Staccato techniques are used to move a stiff joint through its maximum range before the bordering joints have time to start moving as well. If there are no symptoms from the joint, then the speed of the staccato can be quicker, however, if symptoms are moderate, then the movements need to be more fluid. | |||
There is evidence to suggest that different segments of the lumbar spine will react slightly differently, for example; when a PA is performed on L3, 4 and 5, they tend to move into extension, and all three segments will move in response to a PA on one vertebra. However, with L1 and L2, the lower L3, 4 and 5 segments move relatively into flexion. The physiotherapist needs to be aware of the effect of a PA mobilisation on neighbouring vertebra segments <ref name="Powers et al, 2003">Powers CM, Kulig K, Harrison J, Bergman G (2003). Segmental mobility of the lumbar spine during a posterior to anterior mobilization: assessment using dynamic MRI. Clinical Biomechanics 18:80-83</ref> | |||
=== Pain === | |||
'''For patients who have severe pain that is limiting movement'''<ref name="Maitland et al. 2005" />. The joint being treated should be positioned in a symptom-free way. To decide between accessory movements and physiological movements, the one, which can be performed with the larges amplitude of movement, most comfortable for the patient, is used. If a joint is painful, oscillations in mobilisations should be smoothly and even, so that changes between the on and off pressure cannot be detected. | |||
< | == Types of Mobilisations == | ||
Mobilisations can significantly decrease localised pain in the short term, about 24 hours, and can potentially lead to a greater decrease of pain long term compared to no treatment <ref name="Hanrahan et al 2005">Hanrahan S, Bonnie L, et al (2005) The short-term effects of joint mobilizations on acute mechanical low back dysfunction in collegiate athletes. Journal of athletic training 40(2)</ref>. To most effectively treat the pain, the symptomatic level of vertebra should be selected rather than a randomly selected level <ref name="Chiradejnant et. al. 2002">• Chiradejnant A, Latimer J, Maher CG, Stepkovitch N, (2002) Does the choice of spinal level treated during posterioanterior (PA) mobilisation affect the treatment outcome? Physiotherapy Theory and Practice 18, 165-174</ref> | |||
=== Accessory Movements === | |||
*Pressure is applied through the thumb or pisiform to produce large amplitude of movement, with very little pressure and without any degree of stiffness felt. | |||
*The amplitude of the movement should be as large as possible without causing any pain. As symptoms improve, then the amplitude of the movements can increase gradually, although mobilisations have been shown to have a beneficial hypoalgesic regardless of amplitude. <ref name="Krouwel, Hebron and Willett, 2009">Krouwel O, Hebron C, Wilet E, (2009) An investigation into the potential hypoalgesic effects of different amplitudes of PA mobilisations on the lumbar spine as measured by pressure pain thresholds (PPT). Manual Therapy 15:7-12</ref> | |||
=== Physiological Movements === | |||
When these are used they should not cause any discomfort | |||
*Any movements should be in the painless direction, in a large, slow, smooth manner, stopping before the onset of any discomfort. As the patient’s symptoms and ROM improve, the technique can be taken into a known and controlled degree of discomfort. | *Any movements should be in the painless direction, in a large, slow, smooth manner, stopping before the onset of any discomfort. As the patient’s symptoms and ROM improve, the technique can be taken into a known and controlled degree of discomfort. | ||
== Grading Mobilisations == | |||
Mobilisation techniques can be performed in different positions of the range, using small or large amplitudes of movements, which are divided into four grades<ref name="Maitland et al. 2005">Maitland, G.D., Hengeveld. E., Banks, K. and English, K.eds., 2005,Vertebral Manipulation, Edition 7, London, Butterworth Heinsmann.</ref>. | |||
=== Grade of Movement === | |||
'''I '''A small-amplitude movement near the starting position of the range | |||
'''II '''A large-amplitude of movement that carries well into the range. It can occupy any part of the range that is free of any stiffness or muscle spasm that does move into stiffness or muscle spasm | '''II '''A large-amplitude of movement that carries well into the range. It can occupy any part of the range that is free of any stiffness or muscle spasm that does move into stiffness or muscle spasm | ||
| Line 91: | Line 76: | ||
'''III''' Also a large-amplitude movement, but one that does move into stiffness or muscle spasm | '''III''' Also a large-amplitude movement, but one that does move into stiffness or muscle spasm | ||
'''IV''' A small-amplitude movement stretching into stiffness or muscle spasm | '''IV''' A small-amplitude movement stretching into stiffness or muscle spasm | ||
== Contraindications/Precautions to Vertebral Mobilisations<ref name="Gibbons 2001">Gibbons P, Tehan P, (2001) Patient positioning and spinal locking for lumbar spine rotation manipulation. Manual Therapy, 6(3), 130-138</ref><ref name="Maitland te al. 2005">Maitland, G.D., Hengeveld. E., Banks, K. and English, K.eds., 2005,Vertebral Manipulation, Edition 7, London, Butterworth Heinsmann.</ref> == | |||
*Neurological: | *Neurological: | ||
| Line 103: | Line 84: | ||
*Radiological changes: | *Radiological changes: | ||
**Patients with rheumatoid arthritis and osteoporosis are contraindications to forceful mobilizations.<br> Any pathology leading to significant bone weakening such as tumours, infections, long-term corticosteroid medication, fracture | **Patients with rheumatoid arthritis and osteoporosis are contraindications to forceful mobilizations.<br> Any pathology leading to significant bone-weakening such as tumours, infections, long-term corticosteroid medication, fracture | ||
**Patients with vertigo need close supervision | |||
**Patients with vertigo need close supervision | |||
*Hypermobility: | *Hypermobility: | ||
**If a vertebra in the spine was hypermobile compared to the other vertebra, care must be taken to avoid putting excessive strain on the hypermobile joint | **If a vertebra in the spine was hypermobile compared to the other vertebra, care must be taken to avoid putting excessive strain on the hypermobile joint | ||
| Line 114: | Line 94: | ||
*Pregnancy | *Pregnancy | ||
*Musculoskeletal deformity | *Musculoskeletal deformity | ||
**Spondylolysis, | **Spondylolysis, spondylolisthesis | ||
== Mobilisations of the Lumbar Spine == | |||
'''<u></u>''' | |||
===Passive Physiological Intervertebral Movements (PPIVMs)=== | |||
Passive Physiological Intervertebral Movements (PPIVMs) are most often used in an assessment capacity rather than as a treatment therapy. PPIVMs are used to determine a range of properties of spinal movement that will guide the use of manual therapy techniques <ref>Magee, D., Zachazewski, J., Quillen, W., (2008). Pathology and Intervention in Musculoskeletal Rehabilitation. Missouri. Elsevier.</ref>. PPIVMs test the movement available at the spinal level identified by application of a passive physiological motion <ref>Binkley, J., Stratford, P., and Gill, C., (1995). Interrater Reliability of Lumbar Accessory Motion Mobility Testing. Physical Therapy, Vol 75 (9) 786-795.</ref> and palpating between adjacent spinous process or articular facets <ref>Hertling, D., and Kessler, R., (2006). Management Of Common Musculoskeletal Disorders: Physical Therapy Principles And Methods. 4th edition. Philadelphia. Lippincott Williams & Wilkins.</ref>. While the therapist passively moves the spine they can note the range of motion, any muscle spasm or provocation of pain <ref>Hertling, D., and Kessler, R., (2006). Management Of Common Musculoskeletal Disorders: Physical Therapy Principles And Methods. 4th edition. Philadelphia. Lippincott Williams & Wilkins.</ref>. They can confirm any restriction of motion seen in active movement and can also identify hypermobility <ref>Porter, S., and Tidy, N., 2008. Tidy's Physiotherapy. 14th Edition. London. Elsevier.</ref>. Additionally the spine can be taken to the end of range and there the therapist can apply over pressure to assess the end-feel of the movement <ref>Maitland, G., Hengeveld. E., Banks, K. and English, K., (2005). Maitland's Vertebral Manipulation. 7th Edition. London. Elsevier.</ref>. In this way PPIVMs can help the therapist to identify location, nature, severity and irritability of symptoms. | |||
== | ==== Reliability ==== | ||
Research has shown that PPIVMs have a good intra-tester reliability <ref>Binkley, J., Stratford, P., and Gill, C., (1995). Interrater Reliability of Lumbar Accessory Motion Mobility Testing. Physical Therapy, Vol 75 (9) 786-795.</ref>. However, the inter-tester reliability has often been questioned and some research has reported it to be poor <ref>Binkley, J., Stratford, P., and Gill, C., (1995). Interrater Reliability of Lumbar Accessory Motion Mobility Testing. Physical Therapy, Vol 75 (9) 786-795.</ref> <ref>Phillips, D., Twomey, L., (1996). A comparison of manual diagnosis with a diagnosis established by a uni-level lumbar spinal block procedure. Manual therapy, Vol 2, 82-87.</ref>. Research has shown that PIVMs testing in flexion has high specificity (99%) but low sensitivity (5%) <ref>Abbott, J., (2007). Passive intervertebral motion tests for diagnosis of lumbar segmental instability. Australian Journal of Physiotherapy, Vol 53, 66.</ref>. | |||
' | ==== Method ==== | ||
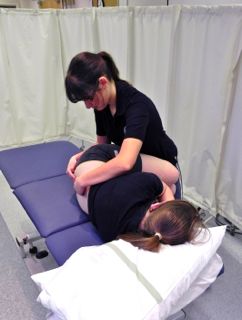
(see Fig. 1) <ref>Maitland, G., Hengeveld. E., Banks, K. and English, K., (2005). Maitland's Vertebral Manipulation. 7th Edition. London. Elsevier.</ref> | |||
* <u></u>The patient lies on their side with hips and knees flexed . The therapists positions themselves in front of the patient. | |||
* The therapist reaches under the patients knees, lifting them up and resting the patients lower legs against the therapists upper thighs. | |||
* Leaning over the patient the therapist places one arm over the patients scapular to prevent backward rotation of thorax. | |||
* The therapist places their fingers on the spinous process of the segment to be assessed for movement | |||
* To produce passive flexion the therapist rocks from side to side with their pelvis, carrying the patients legs along with them. | |||
* Opening and closing of the interspinous gaps can be felt as the patient is passively flexed.<br><br>From this position passive extension can also be assessed.<br> <br>When palpating/assessing the lower lumbar spine the movement will need to be performed in relatively more flexion when assessing the upper lumbar spine movement <ref>Maitland, G., Hengeveld. E., Banks, K. and English, K., (2005). Maitland's Vertebral Manipulation. 7th Edition. London. Elsevier.</ref>.<br> | |||
[[Image:Physiological flexion positioning.jpg|center|Physiological flexion positioning]] Fig 1. Physiological flexion positioning | |||
===== | ===== PPIVMs in Alternate Planes ===== | ||
* Beyond Flexion Extension, Lumbar PPIVMs and PAIVMs can be performed in Extension, Side-flexion, Rotation and in a combination of planes | |||
====== Side-flexion ====== | |||
* The pt is positioned in side lying facing the PT. They are asked to slide close to the edge of the table. | |||
* PT’s cranial arm hooks under the pt’s top arm & the PT’s hand palpates for segmental motion. | |||
* PT’s caudal hand holds the pt’s legs above the ankles with the pt’s legs against the PT’s thighs. | |||
* Side bending motion is introduced by the PT’s arms & body by raising or lowering the patients distal legs. Can do ipsi- & contralateral SB. | |||
* Overpressure (PAIVM) can be done with cranial hand while stabilizing the bottom segments through the pelvis. | |||
===== | ====== Rotation ====== | ||
* The pt is positioned in side lying facing the PT. They are asked to slide close to the edge of the table. | |||
* PT’s cranial arm hooks under the pt’s top arm & the PT’s hand palpates for segmental motion. | |||
* PT’s caudal arm stabilizes the pt’s pelvis against the PT’s body & the caudal hand palpates for motion of the inferior segment. | |||
* Rotation motion is introduced by the PT’s cranial arm & body. | |||
* Overpressure (PAIVM) can be done with cranial hand while stabilizing the bottom segment with the caudal hand. | |||
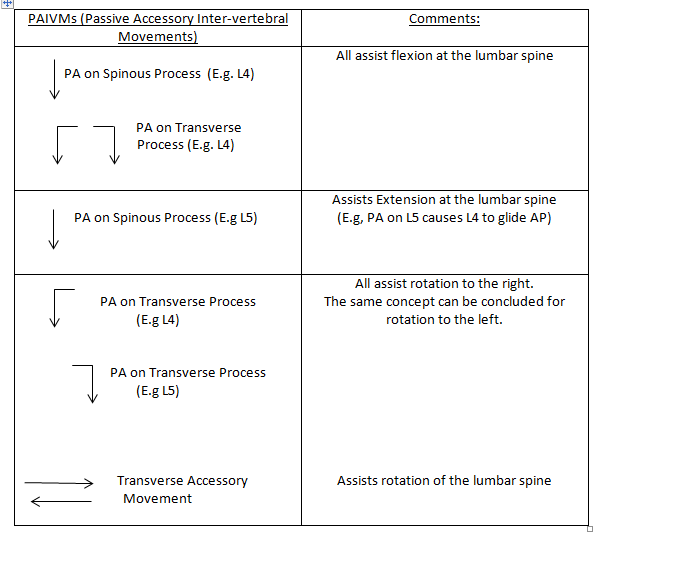
=== Central Posteroanterior (PA) Mobilisation Technique === | |||
A Passive accessory intervertebral movement (PAIVM) is a mobilisation technique that produces movement of a mobile vertebral segment without the active participation of muscles related to the movement<ref name="Maitland et al, 2005" />. Posteroanterior (PA) mobilisations of the lumbar spine are achieved by applying a force on to a vertebral segment in a posteroanterior direction (Back to front). | |||
*PA mobilisations are a commonly used manual therapy technique that has shown to be effective at reducing pain in patients with low back pain (LBP) | *PA mobilisations are a commonly used manual therapy technique that has shown to be effective at reducing pain in patients with low back pain (LBP) <ref>Shum, G.L., Tsung, B.Y. and Lee, R.L., 2012, 'The immediate effect of posteroanterior Mobilisation on reducing back pain and the stiffness of the lumbar spine', Archive of Physical Medicine and Rehabilitation, doi: 10.1016/j.apmr.2012.11.020</ref>. So far, evidence suggests immediate pain relief following treatment, and also some evidence suggests an increased range of movement (ROM) of lumbar extension <ref>McCollam, R.L. Cindy, B.J., 1993, 'Effects of Postero-anterior Mobilization on lumbar extension and flexion', Journal of Manual & Manipulative Therapy, vol 1, No.4.</ref> <ref>Powers, C.M., Beneck, G.J., Hulig, K., Landel, R.F. and Fredericson, M., 2008, 'Effects of a single session of posterior-to-anterior spinal mobilization and press-up exercise on pain and response with lumbar spine extension in people with nonspecific low back pain', Journal of the American Physical Therapy Association, Vol.88, Pp.485-493.</ref> <ref>Shum, G.L., Tsung, B.Y. and Lee, R.L., 2012, 'The immediate effect of posteroanterior Mobilisation on reducing back pain and the stiffness of the lumbar spine', Archive of Physical Medicine and Rehabilitation, doi: 10.1016/j.apmr.2012.11.020</ref>. However, literature is still variable on the overall effects of ROM and pain. | ||
*During flexion, the superior vertebral body and its inferior facet joints move relatively anteriorly and superiorly on the inferior vertebral body and its superior facet joints. Therefore, to aid flexion the mobilisation needs to be applied to the vertebra above the stiff/painful vertebra to facilitate the anterior-superior translation of the facet joints. | *During flexion, the superior vertebral body and its inferior facet joints move relatively anteriorly and superiorly on the inferior vertebral body and its superior facet joints. Therefore, to aid flexion the mobilisation needs to be applied to the vertebra above the stiff/painful vertebra to facilitate the anterior-superior translation of the facet joints. | ||
Technique | ==== Technique ==== | ||
Starting Position (see Fig. 2): | |||
Starting Position: | |||
*Patient lying in prone | *Patient lying in prone | ||
*Therapist stands to side of patient placing their pisiform/ulnar surface of hand over the selected spinous process (SP) with their wrist in full extention. Other hand placed ontop of hand to reinforce. | *Therapist stands to side of patient placing their pisiform/ulnar surface of hand over the selected spinous process (SP) with their wrist in full extention. Other hand placed ontop of hand to reinforce. (See Fig. 3). | ||
*Therapist's shoulders should be directly above the SP with elbows slightly bent. | *Therapist's shoulders should be directly above the SP with elbows slightly bent. | ||
Method | ==== Method ==== | ||
*Therapist uses their body weight to apply a PA force to the selected SP by leaning their body over their arms and performing rocking movements to provide oscillatory movements of the vertebra. | *Therapist uses their body weight to apply a PA force to the selected SP by leaning their body over their arms and performing rocking movements to provide oscillatory movements of the vertebra. | ||
On initial assessment and treatment, if the patient has very limited movement, a pillow can be placed underneath their abdomen, or the head end of plinth can be raised to position the Lumbar spine in relative extension. Similarly, if the patient cannot tollerate pressure directly through the spinous process, the therapist can apply pressure either side of the SP with either thumb on the transverse processes (bilateral PA). | |||
Equally, as the patient’s pain and stiffness reduces the position of the patient can be altered to increase flexion nearer to end of range. This can be done by either lowering the foot section of the plinth or kneeling the patient on the floor by the foot of the plinth with his trunk flexed over the plinth ( approx. 20 degrees flexion) <ref name="Maitland et al, 2005">Maitland, G.D., Hengeveld. E., Banks, K. and English, K.eds., 2005,Vertebral Manipulation, Edition 7, London, Butterworth Heinsmann.</ref> | Equally, as the patient’s pain and stiffness reduces the position of the patient can be altered to increase flexion nearer to end of range. This can be done by either lowering the foot section of the plinth (see Fig. 4) or kneeling the patient on the floor by the foot of the plinth with his trunk flexed over the plinth ( approx. 20 degrees flexion) <ref name="Maitland et al, 2005">Maitland, G.D., Hengeveld. E., Banks, K. and English, K.eds., 2005,Vertebral Manipulation, Edition 7, London, Butterworth Heinsmann.</ref> | ||
[[Image:Central Posteroanterior (PA) Mobilisation Technique.jpg|Central posteroanterior mobilisation technique with lumbar spine in neutral]] | [[Image:Central Posteroanterior (PA) Mobilisation Technique.jpg|center|Central posteroanterior mobilisation technique with lumbar spine in neutral]] Fig. 2. Central posteroanterior mobilisation technique with lumbar spine in neutral<br> | ||
[[Image:Hand positioning for central PA.jpg|Hand positioning for central PA]] | [[Image:Hand positioning for central PA.jpg|center|Hand positioning for central PA]] Fig. 3. Hand positioning for central PA | ||
[[Image:PA mobilisation technique with lumbar flexion.jpg|center|PA mobilisation technique with lumbar flexion]] Fig. 4. PA mobilisation technique with lumbar flexion<br> | |||
=== | === Mobilisations with Movement (MWMs) === | ||
Mobilisations with Movement is a manual therapy technique which was developed by Brian Mulligan, for the treatment of musculoskeletal dysfunction <ref>Jonas. (2005). Mosby's Dictionary of Complementary and Alternative Medicine, Elsevier.. Available: http://medical-dictionary.thefreedictionary.com/mobilization+with+movement. Last accessed 11th Jan 2013.</ref>. It involves performing a sustained force (accessory glide) while a previously painful (problematic) movement is performed<ref>Vicenzino. (2009). Mulligans: Mobilisations with movement. Available: http://www.bmulligan.com/conference/downloads/vicenzino_keynote1_MUllConf09.pdf. Last accessed 11th Jan 2013.</ref>. | |||
Usually, the technique is indicated if, during its application the technique enables the impaired joint to move more freely without pain or impediment<ref>Mulligan B. Mobilisation with movement (MWM’s). Journal offckLRManual and Manipulative Therapy 1993;1:154–6.</ref> | Usually, the technique is indicated if, during its application, the technique enables the impaired joint to move more freely without pain or impediment<ref>Mulligan B. Mobilisation with movement (MWM’s). Journal offckLRManual and Manipulative Therapy 1993;1:154–6.</ref>. Mulligan does not prescribe grades of movement or oscillatory movements. He prescribes taking the joint through its full range of movement and this entails taking it into resistance. When performing MWMs, the direction of the applied force is typically perpendicular to the plane of movement or impaired action and in some instances, it is parallel to the treatment plane <ref>Mulligan B. (1992). Extremity joint mobilisations combined with movements. New Zealand Journal of Physiotherapy, 20:28–9.</ref><ref>Mulligan B. (1996). Mobilisations with movement (MWM’S) for the hip jointfckLRto restore internal rotation and flexion. Journal of Manual and Manipulative Therapy, 4:35–6.</ref>. | ||
There have been reports of clinical cases and case | There have been reports of clinical cases and case series which have described the success of MWMs in the management of various musculoskeletal conditions<ref>Stephens G. Lateral epicondylitis. Journal of Manual and ManioulativefckLRTherapy 1995;3:50–8.</ref><ref>Vicenzino B, Wright A. Effects of a novel manipulative physiotherapyfckLRtechnique on tennis elbow: a single case study. Manual TherapyfckLR1995;1(1):30–5.</ref><ref>Hetherington B. Lateral ligament strains of the ankle: do they exist?fckLRManual Therapy 1996;1(5):274–5.</ref><ref>O’Brien T, Vicenzino B. A study of the effects of Mulligan’sfckLRmobilization with movement treatment of lateral ankle pain usingfckLRa case study design. Manual Therapy 1998;3(2):78–84.</ref><ref>Miller J. Case study: Mulligan concept management of ‘‘tennis elbow’’.fckLROrthopaedic Division Review 2000;3:45–7.</ref><ref>Exelby L. The locked lumbar facet joint: intervention using mobilizationsfckLRwith movement. Manual Therapy 2001;6(2):116–21.</ref><ref>Folk B. Traumatic thumb injury management using mobilization withfckLRmovement. Manual Therapy 2001;6(3):178–82.</ref>. See Exelby<ref>Exelby L. The locked lumbar facet joint: intervention using mobilizationsfckLRwith movement. Manual Therapy 2001;6(2):116–21</ref> for success in MWMs in the lumbar spine<br> | ||
===== MWMs to increase Flexion of the Lumbar Spine ===== | |||
Key MWMs: | |||
# Side-lying flexion-extension | |||
# Central and unilateral SNAG in standing | |||
# Standing belt lumbar traction | |||
# Snag in four-point kneeling | |||
==== | ==== Technique One ==== | ||
Starting position | Starting position | ||
*Patient in side lying facing therapist. | *Patient is in side-lying facing therapist. | ||
*The patient's knees should be bent towards their chest in mid lumbar flexion and rested on the | *The patient's knees should be bent towards their chest in mid lumbar flexion and rested on the therapist's hips. | ||
* | *The therapist places their forearms along the patients back to palpate between adjacent spinous processes. | ||
==== Method ==== | |||
*The therapist produces flexion and extension of the lumbar spine by swaying hips left to right (and vice versa) | |||
*To isolate flexion, the problematic level is palpated and when passively moving the spine into flexion a sustained PA force is applied to the spinous process throughout the movement of flexion and then released.<br> | |||
N.B *Correct plinth height is essential for this technique. | |||
* | ** It may take multiple attempts of the MWMs to find the correct level of the lumbar spine to decrease pain and/or stiffness.<u></u> | ||
* | ==== Technique Two ==== | ||
<u></u>Starting Position (See Fig. 5): | |||
*Patient in standing perpendicular to the therapist. | |||
*Therapist's need to stabilise pelvis via placing the cup of hand other the ASIS. | |||
*Therapist to palpate between adjacent spinous processes. | |||
==== Method ==== | |||
*The patient actively flexes the lumbar spine and then extends to return to the neutral position. | |||
*To isolate flexion, again, the problematic level is palpated and when the patient actively moves into flexion, a sustained PA force is applied to the spinous process throughout the movement. | |||
[[Image:MWM - flexion in standing.jpg|center|MWM - flexion in standing technique]] Fig. 5 Flexion in standing technique | |||
| |||
<u></u> | <u></u> | ||
==== <u></u>Technique Three ==== | |||
<u></u>Starting Position: | <u></u>Starting Position (See Fig. 6): | ||
*Patient in | *Patient in sitting, facing away from therapist. | ||
* | *The pelvis is stabilised via a belt being placed around the patients ASIS's and around the therapist's ischial tuberosity. | ||
*Therapist to palpate between adjacent spinous processes. | *Therapist to palpate between adjacent spinous processes. | ||
==== Method ==== | |||
(See Fig. 7) | |||
*The patient actively flexes the lumbar spine and extends to a neutral position. | |||
*The therapist maintains the tension on the belt throughout all movement. | |||
*The patient actively flexes lumbar spine and | *The problematic level is palpated and when the patient actively moves into flexion, a sustained PA force is applied throughout the whole movement of flexion to the spinous process. | ||
* | |||
N.B * The therapist should have bent knees and be able to lean onto the belt to increase the tension of the belt. <ref>Mulligan. (1995). Spinal Mobilisations with Leg Movement (Further Mobilisations with Movement). Journal of Manipulative Therapy. 3 (1), pg25-7.</ref><br> | |||
[[Image:MWM - flexion with belt in sitting upright.jpg|center|MWM - flexion with belt in sitting upright]] Fig. 6. Flexion with belt in sitting upright | |||
[[Image:MWM - flexion with belt in sitting with forward flexion.jpg|center|MWM - flexion with belt in sitting with forward flexion]] Fig. 7. Flexion with belt in sitting with forward flexion | |||
== Technique 4: Snag in four-point kneeling == | |||
Patient starts in four-point, therapist places hand under stomach and over sacrum | |||
[[File:4 snag.png|thumb]] | |||
We gently guide the patients buttock towards their feet | |||
We apply a snag as the patient moves between flexion and tension | |||
=== Recording === | |||
< | <u></u>[[Image:Assesment.png|center]] | ||
== Prescription of Mobilisations == | |||
< | Thus far, there is no definitive evidence for the optimum duration, frequency or amplitude for mobilisation techniques. Most researchers have investigated subject responses' to 3 cycles of 60-second mobilisation which have shown to have immediate effects of local and widespread analgeia<ref name="Krouwel et al, 2012">Krouwel, O., Hebron, C. and Willett, E., 2010, "An investigation into the potential hypoalgesic effects of PA mobilisations on the lumbar spine as measured by pressure pain thresholds (PPT)",Manual Therapy, Vol. 15, Pp. 7-12</ref> <ref name="Goodsell, Lee & Latimer, 2000">Goodsell, M., Lee, M and Latimer, J., 2000, "Short-Term Effects of Lumbar Posteroanterior Mobilization in Individuals With Low-Back Pain",Journal of Manipulative and Physiological Theraputics, Vol. 23, No. 5.</ref><ref name="Willet, Hebron & Krouwel, 2009">Willett, E., Hebron,C. and Krouwel, O., 2009, "The initial effects of different rates of mobilisations on pressure pain thresholds in asymptomatic subjects", Manual Therapy, Vol.15, Pp.173-178</ref>. However, the duration, rate and frequency of mobilisations should be tailored to the patient's irritability and the preference of both patient and therapist<ref name="Maitland, 2005">Maitland, G.D., Hengeveld. E., Banks, K. and English, K.eds., 2005,Vertebral Manipulation, Edition 7, London, Butterworth Heinsmann.</ref>. Current guidelines suggest that non-specific LBP patients should receive a 12-week course of manual therapy<ref name="N.I.C.E, 2009">N.I.C.E guidelines, 2009, Low back pain: Early management of persistent non-specific low back pain, National Institute for Health and Clinical Excellence, Manchester.</ref> | ||
= References = | <br>Moreover, it is generally agreed that the oscillation depth and amplitude of movement are dependent on the patient's symptoms.<br>If the patient's main symptom is pain then oscillation depth should remain shallow (<55%) and should be maintained within a pain-free range (e.g. Grade I and II). However, if the patient's main complaint is of stiffness then the depth of oscillation can progress to end of range providing pain is tolerable (e.g. Grade III and IIII). Refer to section 2 for Maitland scale. | ||
== References == | |||
<references /> | <references /> | ||
[[Category:Nottingham University Spinal Rehabilitation Project]] | |||
[[Category:Interventions]] | |||
[[Category:Lumbar Spine - Interventions]] | |||
Latest revision as of 14:17, 17 April 2023
Original Editors - Jenny Arnatt, Tabitha Eddleston, Victoria Jovcic, Lizzie Wakeham as part of the Nottingham University Spinal Rehabilitation Project
Top Contributors - Tabitha Eddleston, Victoria Jovcic, Lizzie Wakeham, Jenny Arnatt, Kim Jackson, Admin, Rachael Lowe, Samuel Winter, 127.0.0.1, Tony Lowe, Johnathan Fahrner, Kai A. Sigel and Angeliki Chorti
Introduction[edit | edit source]
In principle, any of the structures within the lumbar spine that receive innervation from the nervous system can be a source of back pain. Thus back pain can arise from any of the ligaments, muscles, fascia, joints or discs of the Lumbar Spine. Read more information on low back pain.
Mobilisations[edit | edit source]
Mobilisations primarily consist of passive movements which can be classified as physiological or accessory [1]. The purpose is to provide short term pain relief and to restore pain-free, functional movements by achieving full range at the joint [2].
Joint mobilisation is a treatment technique which can be used to manage musculoskeletal dysfunction [3], by restoring the motion in the respective joint [4]. The techniques are performed by physiotherapists and fall under the category of manual therapy. Spinal mobilisation is described in terms of improving mobility in areas of the spine that are restricted [5]. Such restriction may be found in joints, connective tissues or muscles. By removing the restriction by mobilisation the source of pain is reduced and the patient experiences symptomatic relief. This results in gentle mobilisations being used for pain relief while more forceful, deeper mobilisations are effective for decreasing joint stiffness. [6].
Effects and Mechanisms[edit | edit source]
Research has shown that mobilisation used as therapy can produce significant mechanical and neurophysiological effects [7] [8] [9] [10]. The explanations of these effects - the mechanism of mobilisation - is still relatively unknown, especially in regards to the spine, and is subject to further research [11].
However, several theories have been established in accordance with the effects seen, including the effects of pain relief, increasing range of motion and the influence on the autonomic nervous system.
Pain Relief[edit | edit source]
Mobilisations offer pain relief through hypoalgesia - decreasing the nervous system's sensitivity to painful stimuli. There are various potential mechanisms of this neurophysiological effect:
- Pain gating
Pain gating refers to the theory that stimulation of the mechano-receptive peripheral afferent nerves in the muscles produce sensory input that interferes with nociceptive impulses at the spinal cord [12]. The input from the larger sensory nerves inhibits the transmission of pain through the smaller nociceptive nerves to the brain, leading to a pain-relieving result [13]. Therefore, the processes of stimulating mechanoreceptors via mobilisation produce short term pain relief through the mechanism of pain gating [14]. However, the pain gate theory only explains the pain-relieving effect during the mobilisation, not any long term effects post-treatment. Therefore it is hypothesised that any longer-term pain-relieving effects are mediated by higher brain mechanisms [15] - Descending mechanisms and supraspinal regions
Research has shown that mobilisation leads to activation of pain inhibitory pathways that originate in the midbrain and travel down the spinal cord - the descending pathways [16] [17] [18]. The pathway stimulation works to provide pain relief by suppression of pain through this inhibitory mechanism.
In addition to this these descending pathways, research has shown a trend where regions of the brain responsible for central pain processing are suppressed during mobilisation [19]. - Adaptation
It has been hypothesised that mobilisation promotes adaptations of the nervous system [20] with a decrease in the level of neural input from the painful site. Research also suggests that mobilisations increase the pain threshold levels - relative hypoalgesia [21]. It has been suggested that this could be due to electrochemical changes in the regulation of threshold potential [22].
Increasing Range of Motion[edit | edit source]
Mobilisations are often used with the objective to increase the range of motion of the joint through stretching of fibrous tissue [23]. This stretching may cause the tissue to 'creep'. The phenomenon of creep relates to the ability of tissues to change shape over time as a constant load is applied. The creep deformation is not permanent and, once the load is removed, the tissue will slowly resume its original length [24]. However, in the short term, this mechanical effect of mobilisation enables an increase in range of motion at the joint.
Influence on Autonomic Nervous System[edit | edit source]
Mobilisation has been found to influence sympathetic activity, affecting heart rate, blood pressure [25] and respiratory rate [26]. These sympathetic responses could possibly be linked to another evidenced effect of mobilisation - changes in blood component levels. Teodorczyk-Injeyan et al (2006) found that mobilisation effected the levels of blood components, with a reduction in inflammatory proteins. Therefore it was suggested that mobilisation could be a potential therapeutic modality to reduce inflammatory response - working as an anti-inflammatory mechanism, though the exact explanation for this process is unknown [27].
Bialosky et al (2009)[28] suggested that the mechanical and neurophysiological effects explored here are interlinked. They proposed that a mechanical force initiates a chain of neurological responses, which would then produce the outcomes associated with manual therapy.
This proposal was illustrated in their model of the mechanisms of manual therapy[29].
The effects of mobilisation and the mechanisms responsible are not fully understood and more research is needed to provide evidence for the theories discussed. It is also important to note that variables such as the placebo effect and psychological factors may also pertain to the effects seen [30].
Effects of Mobilisation on Stiffness and Pain[edit | edit source]
Mobilisations involving pressure onto the vertebra can be used to increase joint range of motion, and also to produce and analgesic effect.
Manual therapy and mobilisations can be used to treat 5 symptom groups:[31][32]
- Pain
- Stiffness
- Pain associated with stiffness
- Momentary jabs of pain
- Disorders directly related to a specific diagnosis
Stiffness[edit | edit source]
For patients whose joint stiffness is limiting normal function.[33] First, assess the patient's movement using physiological movements, select the movement that has limited ROM and needs to be stretched. Then accessory movements can be used. Pressure applied through the thumb or pisiform against the vertebrae in the direction of the movement that is stiff.
Staccato techniques are used to move a stiff joint through its maximum range before the bordering joints have time to start moving as well. If there are no symptoms from the joint, then the speed of the staccato can be quicker, however, if symptoms are moderate, then the movements need to be more fluid.
There is evidence to suggest that different segments of the lumbar spine will react slightly differently, for example; when a PA is performed on L3, 4 and 5, they tend to move into extension, and all three segments will move in response to a PA on one vertebra. However, with L1 and L2, the lower L3, 4 and 5 segments move relatively into flexion. The physiotherapist needs to be aware of the effect of a PA mobilisation on neighbouring vertebra segments [34]
Pain[edit | edit source]
For patients who have severe pain that is limiting movement[33]. The joint being treated should be positioned in a symptom-free way. To decide between accessory movements and physiological movements, the one, which can be performed with the larges amplitude of movement, most comfortable for the patient, is used. If a joint is painful, oscillations in mobilisations should be smoothly and even, so that changes between the on and off pressure cannot be detected.
Types of Mobilisations[edit | edit source]
Mobilisations can significantly decrease localised pain in the short term, about 24 hours, and can potentially lead to a greater decrease of pain long term compared to no treatment [35]. To most effectively treat the pain, the symptomatic level of vertebra should be selected rather than a randomly selected level [36]
Accessory Movements[edit | edit source]
- Pressure is applied through the thumb or pisiform to produce large amplitude of movement, with very little pressure and without any degree of stiffness felt.
- The amplitude of the movement should be as large as possible without causing any pain. As symptoms improve, then the amplitude of the movements can increase gradually, although mobilisations have been shown to have a beneficial hypoalgesic regardless of amplitude. [37]
Physiological Movements[edit | edit source]
When these are used they should not cause any discomfort
- Any movements should be in the painless direction, in a large, slow, smooth manner, stopping before the onset of any discomfort. As the patient’s symptoms and ROM improve, the technique can be taken into a known and controlled degree of discomfort.
Grading Mobilisations[edit | edit source]
Mobilisation techniques can be performed in different positions of the range, using small or large amplitudes of movements, which are divided into four grades[33].
Grade of Movement[edit | edit source]
I A small-amplitude movement near the starting position of the range
II A large-amplitude of movement that carries well into the range. It can occupy any part of the range that is free of any stiffness or muscle spasm that does move into stiffness or muscle spasm
III Also a large-amplitude movement, but one that does move into stiffness or muscle spasm
IV A small-amplitude movement stretching into stiffness or muscle spasm
Contraindications/Precautions to Vertebral Mobilisations[38][39][edit | edit source]
- Neurological:
- Patient with arm pain and neurological signs, from two nerve routes
Disturbance of bladder and bowel function, or perineal anaesthesia
Spinal cord symptoms
- Patient with arm pain and neurological signs, from two nerve routes
- Radiological changes:
- Patients with rheumatoid arthritis and osteoporosis are contraindications to forceful mobilizations.
Any pathology leading to significant bone-weakening such as tumours, infections, long-term corticosteroid medication, fracture - Patients with vertigo need close supervision
- Patients with rheumatoid arthritis and osteoporosis are contraindications to forceful mobilizations.
- Hypermobility:
- If a vertebra in the spine was hypermobile compared to the other vertebra, care must be taken to avoid putting excessive strain on the hypermobile joint
- Vascular
- Aortic aneurysm, bleeding into joints, e.g. severe Haemophilia
- Pregnancy
- Musculoskeletal deformity
- Spondylolysis, spondylolisthesis
Mobilisations of the Lumbar Spine[edit | edit source]
Passive Physiological Intervertebral Movements (PPIVMs)[edit | edit source]
Passive Physiological Intervertebral Movements (PPIVMs) are most often used in an assessment capacity rather than as a treatment therapy. PPIVMs are used to determine a range of properties of spinal movement that will guide the use of manual therapy techniques [40]. PPIVMs test the movement available at the spinal level identified by application of a passive physiological motion [41] and palpating between adjacent spinous process or articular facets [42]. While the therapist passively moves the spine they can note the range of motion, any muscle spasm or provocation of pain [43]. They can confirm any restriction of motion seen in active movement and can also identify hypermobility [44]. Additionally the spine can be taken to the end of range and there the therapist can apply over pressure to assess the end-feel of the movement [45]. In this way PPIVMs can help the therapist to identify location, nature, severity and irritability of symptoms.
Reliability[edit | edit source]
Research has shown that PPIVMs have a good intra-tester reliability [46]. However, the inter-tester reliability has often been questioned and some research has reported it to be poor [47] [48]. Research has shown that PIVMs testing in flexion has high specificity (99%) but low sensitivity (5%) [49].
Method [edit | edit source]
(see Fig. 1) [50]
- The patient lies on their side with hips and knees flexed . The therapists positions themselves in front of the patient.
- The therapist reaches under the patients knees, lifting them up and resting the patients lower legs against the therapists upper thighs.
- Leaning over the patient the therapist places one arm over the patients scapular to prevent backward rotation of thorax.
- The therapist places their fingers on the spinous process of the segment to be assessed for movement
- To produce passive flexion the therapist rocks from side to side with their pelvis, carrying the patients legs along with them.
- Opening and closing of the interspinous gaps can be felt as the patient is passively flexed.
From this position passive extension can also be assessed.
When palpating/assessing the lower lumbar spine the movement will need to be performed in relatively more flexion when assessing the upper lumbar spine movement [51].
Fig 1. Physiological flexion positioning
PPIVMs in Alternate Planes[edit | edit source]
- Beyond Flexion Extension, Lumbar PPIVMs and PAIVMs can be performed in Extension, Side-flexion, Rotation and in a combination of planes
Side-flexion[edit | edit source]
- The pt is positioned in side lying facing the PT. They are asked to slide close to the edge of the table.
- PT’s cranial arm hooks under the pt’s top arm & the PT’s hand palpates for segmental motion.
- PT’s caudal hand holds the pt’s legs above the ankles with the pt’s legs against the PT’s thighs.
- Side bending motion is introduced by the PT’s arms & body by raising or lowering the patients distal legs. Can do ipsi- & contralateral SB.
- Overpressure (PAIVM) can be done with cranial hand while stabilizing the bottom segments through the pelvis.
Rotation[edit | edit source]
- The pt is positioned in side lying facing the PT. They are asked to slide close to the edge of the table.
- PT’s cranial arm hooks under the pt’s top arm & the PT’s hand palpates for segmental motion.
- PT’s caudal arm stabilizes the pt’s pelvis against the PT’s body & the caudal hand palpates for motion of the inferior segment.
- Rotation motion is introduced by the PT’s cranial arm & body.
- Overpressure (PAIVM) can be done with cranial hand while stabilizing the bottom segment with the caudal hand.
Central Posteroanterior (PA) Mobilisation Technique[edit | edit source]
A Passive accessory intervertebral movement (PAIVM) is a mobilisation technique that produces movement of a mobile vertebral segment without the active participation of muscles related to the movement[31]. Posteroanterior (PA) mobilisations of the lumbar spine are achieved by applying a force on to a vertebral segment in a posteroanterior direction (Back to front).
- PA mobilisations are a commonly used manual therapy technique that has shown to be effective at reducing pain in patients with low back pain (LBP) [52]. So far, evidence suggests immediate pain relief following treatment, and also some evidence suggests an increased range of movement (ROM) of lumbar extension [53] [54] [55]. However, literature is still variable on the overall effects of ROM and pain.
- During flexion, the superior vertebral body and its inferior facet joints move relatively anteriorly and superiorly on the inferior vertebral body and its superior facet joints. Therefore, to aid flexion the mobilisation needs to be applied to the vertebra above the stiff/painful vertebra to facilitate the anterior-superior translation of the facet joints.
Technique[edit | edit source]
Starting Position (see Fig. 2):
- Patient lying in prone
- Therapist stands to side of patient placing their pisiform/ulnar surface of hand over the selected spinous process (SP) with their wrist in full extention. Other hand placed ontop of hand to reinforce. (See Fig. 3).
- Therapist's shoulders should be directly above the SP with elbows slightly bent.
Method[edit | edit source]
- Therapist uses their body weight to apply a PA force to the selected SP by leaning their body over their arms and performing rocking movements to provide oscillatory movements of the vertebra.
On initial assessment and treatment, if the patient has very limited movement, a pillow can be placed underneath their abdomen, or the head end of plinth can be raised to position the Lumbar spine in relative extension. Similarly, if the patient cannot tollerate pressure directly through the spinous process, the therapist can apply pressure either side of the SP with either thumb on the transverse processes (bilateral PA).
Equally, as the patient’s pain and stiffness reduces the position of the patient can be altered to increase flexion nearer to end of range. This can be done by either lowering the foot section of the plinth (see Fig. 4) or kneeling the patient on the floor by the foot of the plinth with his trunk flexed over the plinth ( approx. 20 degrees flexion) [31]
Fig. 2. Central posteroanterior mobilisation technique with lumbar spine in neutral
Fig. 3. Hand positioning for central PA
Fig. 4. PA mobilisation technique with lumbar flexion
Mobilisations with Movement (MWMs)[edit | edit source]
Mobilisations with Movement is a manual therapy technique which was developed by Brian Mulligan, for the treatment of musculoskeletal dysfunction [56]. It involves performing a sustained force (accessory glide) while a previously painful (problematic) movement is performed[57].
Usually, the technique is indicated if, during its application, the technique enables the impaired joint to move more freely without pain or impediment[58]. Mulligan does not prescribe grades of movement or oscillatory movements. He prescribes taking the joint through its full range of movement and this entails taking it into resistance. When performing MWMs, the direction of the applied force is typically perpendicular to the plane of movement or impaired action and in some instances, it is parallel to the treatment plane [59][60].
There have been reports of clinical cases and case series which have described the success of MWMs in the management of various musculoskeletal conditions[61][62][63][64][65][66][67]. See Exelby[68] for success in MWMs in the lumbar spine
MWMs to increase Flexion of the Lumbar Spine[edit | edit source]
Key MWMs:
- Side-lying flexion-extension
- Central and unilateral SNAG in standing
- Standing belt lumbar traction
- Snag in four-point kneeling
Technique One[edit | edit source]
Starting position
- Patient is in side-lying facing therapist.
- The patient's knees should be bent towards their chest in mid lumbar flexion and rested on the therapist's hips.
- The therapist places their forearms along the patients back to palpate between adjacent spinous processes.
Method[edit | edit source]
- The therapist produces flexion and extension of the lumbar spine by swaying hips left to right (and vice versa)
- To isolate flexion, the problematic level is palpated and when passively moving the spine into flexion a sustained PA force is applied to the spinous process throughout the movement of flexion and then released.
N.B *Correct plinth height is essential for this technique.
** It may take multiple attempts of the MWMs to find the correct level of the lumbar spine to decrease pain and/or stiffness.
Technique Two[edit | edit source]
Starting Position (See Fig. 5):
- Patient in standing perpendicular to the therapist.
- Therapist's need to stabilise pelvis via placing the cup of hand other the ASIS.
- Therapist to palpate between adjacent spinous processes.
Method[edit | edit source]
- The patient actively flexes the lumbar spine and then extends to return to the neutral position.
- To isolate flexion, again, the problematic level is palpated and when the patient actively moves into flexion, a sustained PA force is applied to the spinous process throughout the movement.
Fig. 5 Flexion in standing technique
Technique Three[edit | edit source]
Starting Position (See Fig. 6):
- Patient in sitting, facing away from therapist.
- The pelvis is stabilised via a belt being placed around the patients ASIS's and around the therapist's ischial tuberosity.
- Therapist to palpate between adjacent spinous processes.
Method[edit | edit source]
(See Fig. 7)
- The patient actively flexes the lumbar spine and extends to a neutral position.
- The therapist maintains the tension on the belt throughout all movement.
- The problematic level is palpated and when the patient actively moves into flexion, a sustained PA force is applied throughout the whole movement of flexion to the spinous process.
N.B * The therapist should have bent knees and be able to lean onto the belt to increase the tension of the belt. [69]
Fig. 6. Flexion with belt in sitting upright
Fig. 7. Flexion with belt in sitting with forward flexion
Technique 4: Snag in four-point kneeling[edit | edit source]
Patient starts in four-point, therapist places hand under stomach and over sacrum
We gently guide the patients buttock towards their feet
We apply a snag as the patient moves between flexion and tension
Recording[edit | edit source]
Prescription of Mobilisations[edit | edit source]
Thus far, there is no definitive evidence for the optimum duration, frequency or amplitude for mobilisation techniques. Most researchers have investigated subject responses' to 3 cycles of 60-second mobilisation which have shown to have immediate effects of local and widespread analgeia[70] [71][72]. However, the duration, rate and frequency of mobilisations should be tailored to the patient's irritability and the preference of both patient and therapist[73]. Current guidelines suggest that non-specific LBP patients should receive a 12-week course of manual therapy[74]
Moreover, it is generally agreed that the oscillation depth and amplitude of movement are dependent on the patient's symptoms.
If the patient's main symptom is pain then oscillation depth should remain shallow (<55%) and should be maintained within a pain-free range (e.g. Grade I and II). However, if the patient's main complaint is of stiffness then the depth of oscillation can progress to end of range providing pain is tolerable (e.g. Grade III and IIII). Refer to section 2 for Maitland scale.
References[edit | edit source]
- ↑ Porter, S., (2005). Dictionary of Physiotherapy. London. Elsevier.
- ↑ Maitland, G., Hengeveld. E., Banks, K. and English, K., (2005). Maitland's Vertebral Manipulation. 7th Edition. London. Elsevier.
- ↑ Hertling D., and Kessler, R., (1996) Management of Common Musculoskeletal Disorders. Baltimore: Lippincott, Williams & Wilkins.
- ↑ Randall, T., Portney, L., and Harris, BA., (1992). Effects of Joint Mobilization on Joint Stiffness and Active Motion of the Metacarpal-Phalangeal Joint. Journal of Orthopaedic & Sports Physical Therapy. Vol 16, (1) 30-36.
- ↑ Korr, IM., (1977). The neurobiologic mechanisms in manipulative therapy. New York, Plenum Press.
- ↑ Maitland, GD., (1986). Vertebral manipulation. 5th edition. Sydney, Butterworths.
- ↑ Wright, A., (1995). Hypoalgesia post-manipulative therapy: a review of a potential neurophysiological mechanism. Manual Therapy, Vol 1, 11-16
- ↑ Bialosky, J., Bishop, M., Price, D., Robinson, M., and George, S., (2009). The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Therapy, Vol 14, 531-538.
- ↑ Gross, A., Miller, J.,D'Sylva, J., Burnie, S., Goldsmith, C., Graham, N., Haines, T., Bronfort, G., and Hoving J., (2010). Manipulation or Mobilisation for Neck Pain. Cochrane Database of Systematic Reviews, Issue 1, 1-90
- ↑ Zusman, M., (2011). Mechanism of mobilization. Physical Therapy Reviews, Vol 16, (4) 233-236.
- ↑ Krouwel, O., Hebron, C., and Willet, E., (2010). An investigation into the potential hypoalgesic effects of different amplitudes of PA mobilisation on the lumbar spine as measured by pressure pain thresholds (PPT). Manual Therapy, Vol 15, 7-12
- ↑ Pickar, JG., and Wheeler, JD., (2001). Response of muscle proprioceptors to spinal manipulative like loads in the anesthetized cat. Journal of Manipulative and Physiological Therapeutics, Vol 24, 2–11.
- ↑ BJA., (2002). Editorial I - Gate Control Theory of pain stands the test of time. British Journal of Anaesthesia, Vol 88 (6) 755-757.
- ↑ Zusman, M., (1986). Spinal Manipulative Therapy: Review of Some Proposed Mechanisms, and a New Hypothesis. The Australian Journal of Physiotherapy, Vol 32 (2) 89-99
- ↑ Krouwel, O., Hebron, C., and Willet, E., (2010). An investigation into the potential hypoalgesic effects of different amplitudes of PA mobilisation on the lumbar spine as measured by pressure pain thresholds (PPT). Manual Therapy, Vol 15, 7-12
- ↑ Krouwel, O., Hebron, C., and Willet, E., (2010). An investigation into the potential hypoalgesic effects of different amplitudes of PA mobilisation on the lumbar spine as measured by pressure pain thresholds (PPT). Manual Therapy, Vol 15, 7-12
- ↑ Zusman, M., (2011). Mechanism of mobilization. Physical Therapy Reviews, Vol 16 (4) 233-236.
- ↑ Grayson, J., Barton, T., Cabot, P., and Souvlis, T., (2012), Spinal manual therapy produces rapid onset analgesia in a rodent model. Manual Therapy, Vol 17, 292-297.
- ↑ Bialosky, J., Bishop, M., Price, D., Robinson, M., and George, S., (2009). The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Therapy, Vol 14, 531-538.
- ↑ Refshauge, K., and Gass, E., (2004). Musculoskeletal Physiotherapy: clinical science and evidence-based practice. 2nd Edition. Oxford. Butterworth Heinemann.
- ↑ Wright, A., (1995). Hypoalgesia post-manipulative therapy: a review of a potential neurophysiological mechanism. Manual Therapy, Vol 1, 11-16
- ↑ Zusman, M., (1986). Spinal Manipulative Therapy: Review of Some Proposed Mechanisms, and a New Hypothesis. The Australian Journal of Physiotherapy, Vol 32 (2) 89-99
- ↑ Refshauge, K., and Gass, E., (2004). Musculoskeletal Physiotherapy: clinical science and evidence-based practice. 2nd Edition. Oxford. Butterworth Heinemann.
- ↑ Threlkeld, A., (1992). The Effects of Manual Therapy on Connective Tissue. Physical Therapy, Vol 72 (12) 893-902.
- ↑ Zusman, M., (2011). Mechanism of mobilization. Physical Therapy Reviews, Vol 16 (4) 233-236.
- ↑ Wright, A., (1995). Hypoalgesia post-manipulative therapy: a review of a potential neurophysiological mechanism. Manual Therapy, Vol 1, 11-16
- ↑ Teodorczyk-Injeyan, J., Injeyan, H., and Ruegg, R,. (2006). Spinal manipulative therapy reduces inflammatory cytokines but not substance P production in normal subjects. Journal of Manipulative and Physiological Therapeutics, Vol 29, 14–21
- ↑ Bialosky, J., Bishop, M., Price, D., Robinson, M., and George, S., (2009). The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Therapy, Vol 14, 531-538.
- ↑ Bialosky, J., Bishop, M., Price, D., Robinson, M., and George, S., (2009). The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Therapy, Vol 14, 531-538.
- ↑ Ernst, E., (2000). Does spinal manipulation have specific treatment effects? Family Practice, Vol 17, 554–556.
- ↑ 31.0 31.1 31.2 Maitland, G.D., Hengeveld. E., Banks, K. and English, K.eds., 2005,Vertebral Manipulation, Edition 7, London, Butterworth Heinsmann.
- ↑ Fabio R. (1992) Efficacy of manual therapy. Physical Therapy Vol 72, Issue 12
- ↑ 33.0 33.1 33.2 Maitland, G.D., Hengeveld. E., Banks, K. and English, K.eds., 2005,Vertebral Manipulation, Edition 7, London, Butterworth Heinsmann.
- ↑ Powers CM, Kulig K, Harrison J, Bergman G (2003). Segmental mobility of the lumbar spine during a posterior to anterior mobilization: assessment using dynamic MRI. Clinical Biomechanics 18:80-83
- ↑ Hanrahan S, Bonnie L, et al (2005) The short-term effects of joint mobilizations on acute mechanical low back dysfunction in collegiate athletes. Journal of athletic training 40(2)
- ↑ • Chiradejnant A, Latimer J, Maher CG, Stepkovitch N, (2002) Does the choice of spinal level treated during posterioanterior (PA) mobilisation affect the treatment outcome? Physiotherapy Theory and Practice 18, 165-174
- ↑ Krouwel O, Hebron C, Wilet E, (2009) An investigation into the potential hypoalgesic effects of different amplitudes of PA mobilisations on the lumbar spine as measured by pressure pain thresholds (PPT). Manual Therapy 15:7-12
- ↑ Gibbons P, Tehan P, (2001) Patient positioning and spinal locking for lumbar spine rotation manipulation. Manual Therapy, 6(3), 130-138
- ↑ Maitland, G.D., Hengeveld. E., Banks, K. and English, K.eds., 2005,Vertebral Manipulation, Edition 7, London, Butterworth Heinsmann.
- ↑ Magee, D., Zachazewski, J., Quillen, W., (2008). Pathology and Intervention in Musculoskeletal Rehabilitation. Missouri. Elsevier.
- ↑ Binkley, J., Stratford, P., and Gill, C., (1995). Interrater Reliability of Lumbar Accessory Motion Mobility Testing. Physical Therapy, Vol 75 (9) 786-795.
- ↑ Hertling, D., and Kessler, R., (2006). Management Of Common Musculoskeletal Disorders: Physical Therapy Principles And Methods. 4th edition. Philadelphia. Lippincott Williams & Wilkins.
- ↑ Hertling, D., and Kessler, R., (2006). Management Of Common Musculoskeletal Disorders: Physical Therapy Principles And Methods. 4th edition. Philadelphia. Lippincott Williams & Wilkins.
- ↑ Porter, S., and Tidy, N., 2008. Tidy's Physiotherapy. 14th Edition. London. Elsevier.
- ↑ Maitland, G., Hengeveld. E., Banks, K. and English, K., (2005). Maitland's Vertebral Manipulation. 7th Edition. London. Elsevier.
- ↑ Binkley, J., Stratford, P., and Gill, C., (1995). Interrater Reliability of Lumbar Accessory Motion Mobility Testing. Physical Therapy, Vol 75 (9) 786-795.
- ↑ Binkley, J., Stratford, P., and Gill, C., (1995). Interrater Reliability of Lumbar Accessory Motion Mobility Testing. Physical Therapy, Vol 75 (9) 786-795.
- ↑ Phillips, D., Twomey, L., (1996). A comparison of manual diagnosis with a diagnosis established by a uni-level lumbar spinal block procedure. Manual therapy, Vol 2, 82-87.
- ↑ Abbott, J., (2007). Passive intervertebral motion tests for diagnosis of lumbar segmental instability. Australian Journal of Physiotherapy, Vol 53, 66.
- ↑ Maitland, G., Hengeveld. E., Banks, K. and English, K., (2005). Maitland's Vertebral Manipulation. 7th Edition. London. Elsevier.
- ↑ Maitland, G., Hengeveld. E., Banks, K. and English, K., (2005). Maitland's Vertebral Manipulation. 7th Edition. London. Elsevier.
- ↑ Shum, G.L., Tsung, B.Y. and Lee, R.L., 2012, 'The immediate effect of posteroanterior Mobilisation on reducing back pain and the stiffness of the lumbar spine', Archive of Physical Medicine and Rehabilitation, doi: 10.1016/j.apmr.2012.11.020
- ↑ McCollam, R.L. Cindy, B.J., 1993, 'Effects of Postero-anterior Mobilization on lumbar extension and flexion', Journal of Manual & Manipulative Therapy, vol 1, No.4.
- ↑ Powers, C.M., Beneck, G.J., Hulig, K., Landel, R.F. and Fredericson, M., 2008, 'Effects of a single session of posterior-to-anterior spinal mobilization and press-up exercise on pain and response with lumbar spine extension in people with nonspecific low back pain', Journal of the American Physical Therapy Association, Vol.88, Pp.485-493.
- ↑ Shum, G.L., Tsung, B.Y. and Lee, R.L., 2012, 'The immediate effect of posteroanterior Mobilisation on reducing back pain and the stiffness of the lumbar spine', Archive of Physical Medicine and Rehabilitation, doi: 10.1016/j.apmr.2012.11.020
- ↑ Jonas. (2005). Mosby's Dictionary of Complementary and Alternative Medicine, Elsevier.. Available: http://medical-dictionary.thefreedictionary.com/mobilization+with+movement. Last accessed 11th Jan 2013.
- ↑ Vicenzino. (2009). Mulligans: Mobilisations with movement. Available: http://www.bmulligan.com/conference/downloads/vicenzino_keynote1_MUllConf09.pdf. Last accessed 11th Jan 2013.
- ↑ Mulligan B. Mobilisation with movement (MWM’s). Journal offckLRManual and Manipulative Therapy 1993;1:154–6.
- ↑ Mulligan B. (1992). Extremity joint mobilisations combined with movements. New Zealand Journal of Physiotherapy, 20:28–9.
- ↑ Mulligan B. (1996). Mobilisations with movement (MWM’S) for the hip jointfckLRto restore internal rotation and flexion. Journal of Manual and Manipulative Therapy, 4:35–6.
- ↑ Stephens G. Lateral epicondylitis. Journal of Manual and ManioulativefckLRTherapy 1995;3:50–8.
- ↑ Vicenzino B, Wright A. Effects of a novel manipulative physiotherapyfckLRtechnique on tennis elbow: a single case study. Manual TherapyfckLR1995;1(1):30–5.
- ↑ Hetherington B. Lateral ligament strains of the ankle: do they exist?fckLRManual Therapy 1996;1(5):274–5.
- ↑ O’Brien T, Vicenzino B. A study of the effects of Mulligan’sfckLRmobilization with movement treatment of lateral ankle pain usingfckLRa case study design. Manual Therapy 1998;3(2):78–84.
- ↑ Miller J. Case study: Mulligan concept management of ‘‘tennis elbow’’.fckLROrthopaedic Division Review 2000;3:45–7.
- ↑ Exelby L. The locked lumbar facet joint: intervention using mobilizationsfckLRwith movement. Manual Therapy 2001;6(2):116–21.
- ↑ Folk B. Traumatic thumb injury management using mobilization withfckLRmovement. Manual Therapy 2001;6(3):178–82.
- ↑ Exelby L. The locked lumbar facet joint: intervention using mobilizationsfckLRwith movement. Manual Therapy 2001;6(2):116–21
- ↑ Mulligan. (1995). Spinal Mobilisations with Leg Movement (Further Mobilisations with Movement). Journal of Manipulative Therapy. 3 (1), pg25-7.
- ↑ Krouwel, O., Hebron, C. and Willett, E., 2010, "An investigation into the potential hypoalgesic effects of PA mobilisations on the lumbar spine as measured by pressure pain thresholds (PPT)",Manual Therapy, Vol. 15, Pp. 7-12
- ↑ Goodsell, M., Lee, M and Latimer, J., 2000, "Short-Term Effects of Lumbar Posteroanterior Mobilization in Individuals With Low-Back Pain",Journal of Manipulative and Physiological Theraputics, Vol. 23, No. 5.
- ↑ Willett, E., Hebron,C. and Krouwel, O., 2009, "The initial effects of different rates of mobilisations on pressure pain thresholds in asymptomatic subjects", Manual Therapy, Vol.15, Pp.173-178
- ↑ Maitland, G.D., Hengeveld. E., Banks, K. and English, K.eds., 2005,Vertebral Manipulation, Edition 7, London, Butterworth Heinsmann.
- ↑ N.I.C.E guidelines, 2009, Low back pain: Early management of persistent non-specific low back pain, National Institute for Health and Clinical Excellence, Manchester.