International Framework for Examination of the Cervical Region
Original Editor - Lucy Aird
Top Contributors - Tarina van der Stockt, Aya Alhindi, Lucy Aird, Ewa Jaraczewska, Admin, Jess Bell, Kim Jackson, Rachael Lowe, Simisola Ajeyalemi and Claire Knott
Background[edit | edit source]
This page is based on:
Rushton A, Rivett D, Carlesso L, Flynn T, Hing W, Kerry R. International Framework for Examination of the Cervical Region for potential of vascular pathologies of the neck prior to Orthopaedic Manual Therapy (OMT) Intervention: International IFOMPT Cervical Framework. International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT). 2020[1]
This document presents a clinical reasoning framework for best practice developed by an international collaboration of the standards committee of the International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT) and international subject matter experts. The original framework was informed by the consensus forum at the IFOMPT International Conference in Rotterdam (June 2008) where nominated experts from each Member Organisation of IFOMPT were invited to participate. Prior to this forum, the issues central to this document were explored through oral presentations and discussion at the World Confederation for Physical Therapy (WCPT) International Congress (June 2007, Vancouver) and in Rotterdam. Drafts of the document have been developed since 2008 through an iterative consultative process with experts and Member Organisations.
The IFOMPT Cervical Framework Document was published in 2012, as a resource for clinicians. It was scheduled for a revision in 2017 and the final revision was published in September 2020. The revised 2020 framework is available for free on the IFOMPT website. As a consensus document, the Framework was developed through rigorous methods and pivots around clinical reasoning and evidence-based practice.
IFOMPT[edit | edit source]
Please see www.ifompt.org for all information.
The vision statement of IFOMPT is:
"World-wide promotion of excellence and unity in clinical and academic standards for manual/musculoskeletal physiotherapists."
The vision statement summarises the mission of IFOMPT that as an organisation it aims to:
- Promote and maintain the high standards of specialist education and clinical practice in manual/musculoskeletal physiotherapists.
- Promote and facilitate evidence-based practice and research amongst its members.
- Communicate widely the purpose and level of the specialisation of manual/musculoskeletal physiotherapists amongst physiotherapists, other healthcare disciplines and the general public.
- Work towards international unity/conformity of educational standards of practice amongst manual/musculoskeletal physiotherapists.
- Communicate and collaborate effectively with individuals within the organisation and with other organisations.
The Standards Committee of IFOMPT is a sub-committee of the Executive Committee and responsible for advising the Executive on educational issues and maintaining standards. The Standards Document is the guideline document that IFOMPT provides for groups of Manual Therapists who wish to seek membership of IFOMPT through the creation of postgraduate educational programmes in Orthopaedic Manual Therapy (OMT). Part A of the Standards Document[2] details the educational standards.
Reason for the Development of the Framework[edit | edit source]
There is an array of potential vascular pathologies of the neck which is related to the arterial system supplying blood to the brain. There are two implications for physiotherapists/physical therapists who treat musculoskeletal conditions.
- Neurovascular incidents have been associated with therapeutic interventions
- There exist multiple arterial pathologies (vascular masqueraders) which could present as musculoskeletal pain and dysfunction of the neck, like neck pain and headache
The goal of the International IFOMPT Cervical Framework is to increase the physiotherapists understanding of risk and pathology, in order to promote patient safety.
The mission of the Framework is to make sure that educators and physiotherapists have an understanding of the risk in both its epidemiological and individual contexts. Epidemiologically, the risk of an incident due to therapeutic intervention is small but physiotherapists should still give utmost attention to limit the risk to the individual.
The aim of the Framework is "to provide the necessary information to allow both educators and physical therapists to teach and practice with the sound reasoning and knowledge required to make the best clinical decisions, with the result that they are capable of minimising this risk."
Executive summary[edit | edit source]
Key principles of the 2020 International Framework:
- In previous versions, the terminology Cervical Artery Dysfunction (CAD) was used. CAD has been replaced with vascular pathologies of the neck.
- Provocative positional testing, like the Vertebral Artery Test, is no longer recommended due to a lack of evidence of its predictive ability to identify risk.[3] [4]
- The framework is based on best available evidence and is intended to be informative and not prescriptive
- The framework enhances the physical therapist’s clinical reasoning as part of the process of patient assessment and treatment
- An important underlying principle of the framework is that physical therapists cannot rely on the results of only one test to draw conclusions, and therefore development of an understanding of the patient’s presentation following an informed, planned and individualised assessment is essential
- The framework is designed to be an aid to patient-centred clinical reasoning
- The framework requires effective clinical reasoning to enable effective, efficient and safe assessment and management of the cervical region
- The physical therapist’s aim during the patient history is to make the best judgment on the probability of serious pathology and contraindications to treatment based on available information
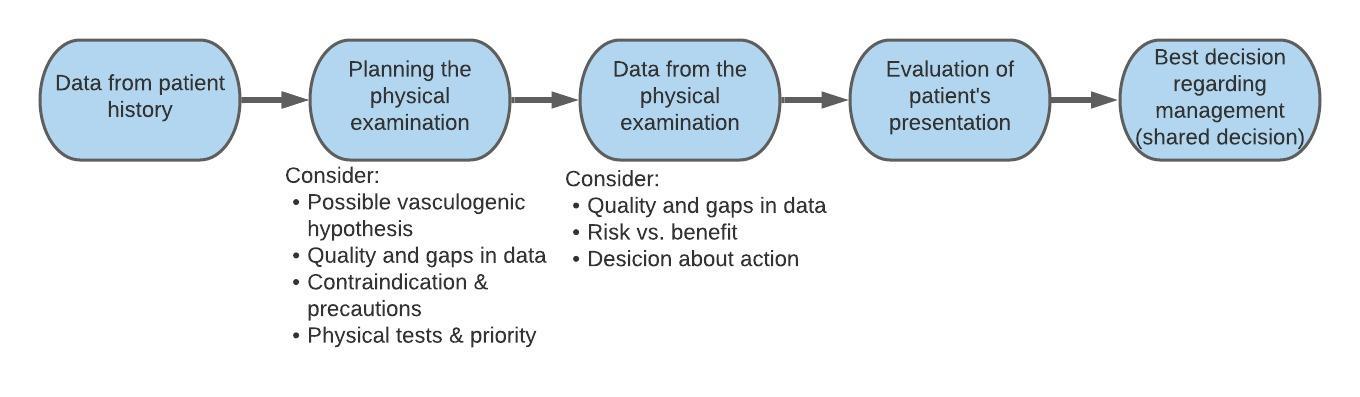
- A process of planning the physical examination to interpret the data from the patient history and define the main hypotheses is essential to an effective physical examination
- It is important that the tests within the physical examination provide reliable and valid data to enable evaluation of the main hypotheses
- Risk versus benefit model is advocated to provide a simple framework for decision-making through consideration of risk factors, predicted benefit of OMT intervention, and analysis of possible action
- A flowchart of clinical reasoning is provided
- Patient-centred decision making following informed consent must be obtained prior to treatment interventions
- Key considerations are provided for the physical therapist during the selection and application of cervical manipulation as a treatment intervention
- Guidance is provided for those teaching cervical assessment and management to students
Aim of the framework[edit | edit source]
The framework is designed to provide guidance for the assessment of the cervical spine region for potential of vascular pathologies in the neck in advance of planned OMT interventions. The IFOMPT definition of Orthopaedic Manual Therapy (OMT), voted in at the General Meeting in Cape Town, March 2004 is:
OMT is a specialised area of physiotherapy / physical therapy for the management of neuro-musculo-skeletal conditions, based on clinical reasoning, using highly specific treatment approaches including manual techniques and therapeutic exercises.
OMT also encompasses, and is driven by, the available scientific and clinical evidence and the biopsychosocial framework of each individual patient.
OMT interventions for the cervical spine addressed through this framework include: manipulation, mobilisation and exercise. Attention is focused to techniques occurring in end range positions of the cervical spine, during mobilisation, manipulation and exercise interventions.
The framework is based on best available evidence at the time of writing. It is designed to be used in conjunction with the IFOMPT Standards[2] that define postgraduate best practice in OMT internationally. Central to this framework are sound clinical reasoning and evidence based practice.
Within the cervical spine, events and presentations of vascular pathologies of the neck are rare, but are an important consideration as part of an OMT assessment. Arterial dissection (a tear in the lining of an artery) and other vascular presentations are fairly recognisable if the appropriate questions are asked during the patient history, if interpretation of elicited data enables recognition of this potential, and if the physical examination can be adapted to explore any potential vasculogenic hypothesis further. The framework is therefore reflective of best practice and aims to place risk in an appropriate context that is informed by the evidence. In this context, the framework considers ischaemic and non-ischaemic presentations to identify risk, prior to overt symptoms in a patient presenting for cervical management.
An important underlying principle of the framework is that physical therapists cannot rely on the results of only one test to draw conclusions, and therefore development of an understanding of the patient’s presentation following an informed, planned and individualised assessment is essential. There are multiple sources of information available from the process of patient assessment to improve the confidence of estimating the probability of vascular pathologies of the neck. Data available to inform clinical reasoning will improve and change with ongoing research. This framework therefore encourages physical therapists to critically read the current literature to enable support for their clinical decisions, rather than provide specific data prescriptive guidance, as the evidence base for this is not available.
The framework is intended to be informative and not prescriptive, and aims to enhance the physical therapist’s clinical reasoning as part of the process of patient assessment and treatment. The framework is intended as simple and flexible. The physical therapist should be able to apply it to their individual patients thereby facilitating patient centred-practice.
IFOMPT Cervical Framework[edit | edit source]
The framework is divided into different sections, and is designed to be used in conjunction with key literature sources identified in the context section.
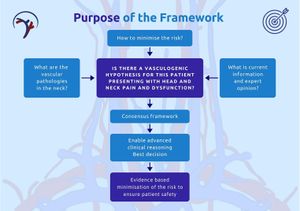
Section 1: Summary infographic[edit | edit source]
- This infographic on page 4 of the framework is a summary of all the different sections within the framework as described below.
Section 2: Aim and scope of the Framework[edit | edit source]
- Provides guidance for the assessment of the cervical spine region for the potential of vascular pathologies of the neck prior to OMT interventions (mobilisation, manipulation and exercise).
- The intention is to inform, not prescribe, and to enhance the physiotherapist's clinical reasoning
- Events and presentations of vascular pathologies of the neck are rare[5] but important to consider in an OMT assessment
- To recognise vascular pathologies appropriate subjective assessment questions should be asked as part of an informed, planned and individualised assessment
- Ischaemic and non-ischaemic presentations should be considered to identify risk in a patient presenting for cervical examination and management
- Physiotherapists should not rely on the results of only one test to draw conclusions
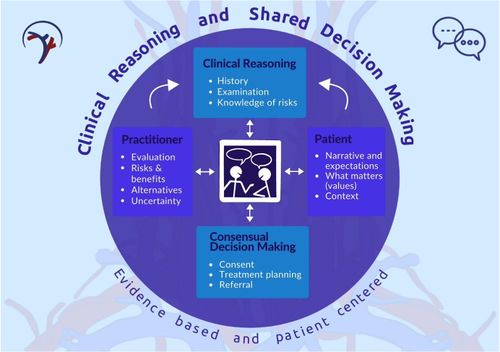
Section 3: Framework underpinned by clinical reasoning[edit | edit source]
"The Framework requires effectiveness in clinical reasoning to enable effective, efficient, and safe assessment and management of the cervical spine region. It is clear that some recorded safety incidents (e.g. following cervical manipulation) could have been avoided if more thorough clinical reasoning had been exercised by the clinician[6]. The Framework is therefore designed to be an aid to patient-centred clinical reasoning."[1]
The IFOMPT Standards Document[7] states that:
“Advanced clinical reasoning skills are central to the practice of OMT Physical Therapists, ultimately leading to decisions formulated to provide the best patient care. Clinical decisions are established following consideration of the patient’s clinical and physical circumstances to establish a clinical physical diagnosis and treatment options. The decisions are informed by research evidence concerning the efficacy, risks, effectiveness, and efficiency of the options[8]. Given the likely consequences associated with each option, decisions are made using a model that views the patient’s role within decision making as central to practice[9], thus describing a patient centred model of practice. Therefore, practice in OMT is informed by a complex integration of research evidence, the patient’s preferences and the patient’s individual clinical presentation.”
“The application of OMT is based on a comprehensive assessment of the patient’s neuromusculoskeletal system and of the patient’s functional abilities. This examination serves to define the presenting dysfunction(s) in the articular, muscular, nervous and other relevant systems; and how these relate to any disability or functional limitation as described by the World Health Organisation’s International Classification of Functioning, Disability and Health. Equally, the examination aims to distinguish those conditions that are indications or contraindications to OMT Physical Therapy and / or demand special precautions, as well as those where anatomical anomalies or pathological processes limit or direct the use of OMT procedures. OMT includes a large range of therapeutic procedures such as passive movements (mobilisation and/or manipulation), rehabilitative exercises, patient information/education as well as other interventions and modalities. The main aims of OMT are to relieve pain and to optimise the patient’s functional ability.”
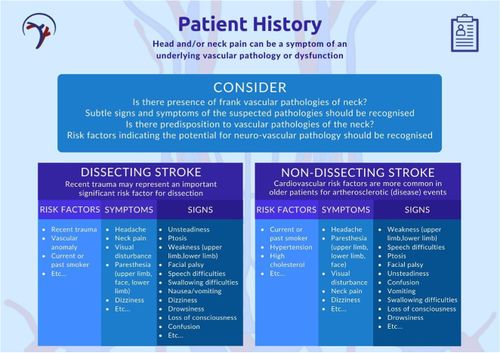
Section 4: Patient history[edit | edit source]
Clinical reasoning process[edit | edit source]
The physiotherapist’s aim is to use the patient history to make the best judgment on the probability of either contraindications to treatment or serious pathology that is present. Please note that the physical examinations proposed in the Framework has very limited diagnostic utility data.
General considerations and specific vascular pathology of the neck considerations[edit | edit source]
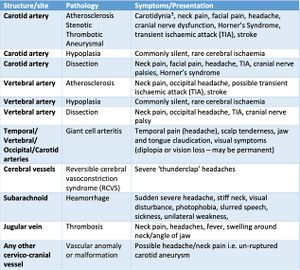
A patient experiencing a vascular pathology of the neck may seek OMT for the relief of this associated pain, these vascular pathologies might mimic musculoskeletal dysfunction i.e. head/neck pain. The physiotherapist should recognise subtle signs and symptoms of the suspected pathologies and risk factors from the patient history
See the table on the right with information to highlight the key components of the patient history in this context.
Typical case histories of vascular dysfunction from the Framework[edit | edit source]
Case: Typical vertebral artery dissection with ischaemic changes
A 46-year-old female supermarket worker presented for physical therapy with left-sided head (occipital) and neck pain described as “unusual”. She reported a 6-day history of the symptoms following a road traffic accident. The symptoms were progressively worsening. The pain was eased by rest. She reported a history of previous road traffic accidents. Past medical history included hypertension, high cholesterol, and a maternal family history of heart disease and stroke. Cranial nerve tests for VIII, IX, and X were positive and resting blood pressure was 170/110. Two days after assessment, the patient reported an onset of new symptoms including “feels like might be sick”, “throaty” and “feels faint” – especially after performing prescribed neck exercises. Two days after this, she reported a stronger feeling of nausea, loss of balance, swallowing difficulties, speech difficulties and acute loss of memory. Magnetic resonance arteriography revealed an acute vertebrobasilar stroke related to a left vertebral (extra-cranial) artery dissection.
Synopsis:
A typical background of vascular risk factors and trauma, together with a classic pain distribution for vertebral arterial somatic pain which was worsening. Positive signs (blood pressure and cranial nerve dysfunction) were suggestive of cervical vascular pathology. Signs of vertebrobasilar ischaemia developed in a typical time period post-trauma.
Case: Vertebral artery with pain as the only clinical feature (non-ischaemic)
A friend presents to a physical therapist with a sore neck and unremitting headache. The individual complains that they “think” their “neck is out”. They ask if they can have their neck manipulated to “put it back in”. The headache has been present for 3-4 days and is getting worse. They note that the pain has been unrelieved by medication (paracetamol) and it appears to be of a mechanical presentation. Without taking a full history and carrying out a physical examination, the physical therapist goes ahead and manipulates the neck. The result was the individual experiencing numbness and paralysis to their left arm and hand.
Synopsis:
Investigation post-incident identified an intimal tear of the vertebral artery. The key issue, in this case, is that the presentation was not fully assessed through a detailed history and physical examination. The warning feature from the history of worsening pain, unrelieved by medication, combined with an inadequate physical examination and limited clinical reasoning, all contributed to an unfortunate and potentially avoidable outcome.
Case: Internal carotid artery dissection
A 42-year-old accountant presents to physical therapy with a 5-day history of unilateral neck and jaw pain, as well as temporal headache, following a rear-end motor vehicle collision. There is a movement restriction of the neck and the physical therapist begins to treat with gentle passive joint mobilisations and advises range of movement exercises. The following day, the patient’s pain is worse, and he has developed an ipsilateral ptosis. The patient’s blood pressure is unusually high.
Synopsis:
On medical investigation, an extra-cranial dissection of the internal carotid artery was found. The patient had underlying risk factors for arterial disease, and the presentation was typical of internal carotid artery dissection, with a key differentiator being the ptosis. A dramatic systemic blood pressure response was a result of this vascular insult.
Section 5: Planning the physical examination[edit | edit source]
Necessity for planning[edit | edit source]
A process of interpreting the data from the patient history and defining the main hypotheses is essential to an effective physical examination[10][11]. Hypothesis generation from the history and refining, re-ranking and rejecting of these hypotheses in the physical examination is necessary to facilitate optimal clinical reasoning in OMT[12]. Therefore careful planning of the physical examination is required. In particular, for this framework, the possible vasculogenic (cervical arterial) contribution to the patient’s presentation needs to be clearly evaluated from the patient history data.
Are any further patient history data required?[edit | edit source]
An important component of planning is the identification of any further patient history data that may be required. That is, are there any gaps in the information obtained? Is the quality of the information obtained sufficient?
Decision-making regarding the physical examination[edit | edit source]
Based upon the evaluation and interpretation of the data from the patient history, the physical therapist needs to decide:
- Are there any precautions to OMT?
- Are there any contraindications to OMT?
- What physical tests need to be included in the physical examination?
- What is the priority for these physical tests for this specific patient? This is to inform decisions regarding the order of testing and to determine which tests should be completed at the first visit.
- Do the physical tests need to be adapted for this specific patient?
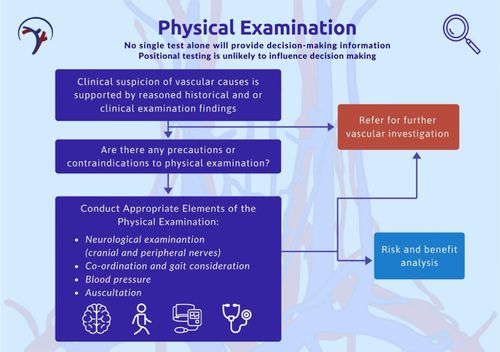
Section 6: Physical examination[edit | edit source]
The purpose of the physical examination is to continue to test the vascular hypothesis generated during the history.
Hypertension is a strong predictor of cardiovascular disease[13], but it should be interpreted in the context of other findings, with sound clinical reasoning. Hypertension and neck pain are only two of the many factors which influence the decision on the probability of vascular pathology.
Neurological examination
Examination of the peripheral nerves and cranial nerves in assessing for an upper motor neuron lesion will assist in evaluating the potential for neurovascular conditions. Follow this link to learn more about testing. There is an increasing body of literature that details clinical cases of arterial pathology with cranial nerve involvement to inform pattern recognition. The absence of findings does not rule out underlying pathology.
Examination of the carotid artery
The physiotherapist should aim to understand and experience both normal and pathological pulse quality. Auscultation is advised as palpation of the internal carotid artery may induce vagal reactions (especially when palpating bilaterally). In most cases, the sensitivity or specificity of pulse examination is unknown, but in the correct clinical context, it may offer important evidence leading to specific diagnoses and treatment[14].
- An alteration of the internal carotid artery pulse has been identified as a feature of the internal carotid disease [15]
- Asymmetry between left and right vessels is considered significant
- A pulsatile, expandable mass is indicative of an arterial aneurysm[16]
- A bruit on auscultation (controlling for normal turbulence) is indicative of a significant finding and should be considered in the context of other clinical findings.
Differentiation during the physical examination
Differentiation of a patient’s symptoms originating from a vasculogenic cause with complete certainty is not currently possible from the physical examination. Thus, it is important for the physical therapist to understand that headache / neck pain may be the early presentation of an underlying vascular pathology[17][18]. The task for the therapist is to differentiate the symptoms by:
- Having a high index of suspicion
- Testing the vascular hypothesis.
This process of differentiation should take place from an early point in the assessment process i.e. early in the patient history. The symptomology and history of a patient experiencing vascular pathology are what may alert the physical therapist to such an underlying problem[17][18]. A high index of suspicion of cervical vascular involvement is required in cases of acute onset neck/head pain described as “unlike any other”[18]. Physical therapists may be exposed to patients presenting with the early signs of stroke (for example, neck pain / headache) and as such need both knowledge and awareness of the mechanisms involved. A basic understanding of vascular anatomy, haemodynamics and the pathogenesis of arterial dysfunction may help the physical therapist differentiate vascular head and neck pain from a musculoskeletal cause[17][18] through interpretation of the patient history data and tests in the physical examination.
Refer on for further investigation
- There exist no clinical guidelines for medical diagnostic work-up in respect of vascular pathology.
- The physiotherapist should follow local policy in referring for further investigation. Immediate referral for medical investigation should take place with clinical suspicion of vascular pathology.
- Conventionally, duplex ultrasound, magnetic resonance imaging/arteriography, and computed tomography are used in the work-up.
Additional training
Physiotherapists should receive additional training if their current OMT practice does not include the tests mentioned in this Framework.
Section 7: Risk and benefit[edit | edit source]
Framework for evaluating risk
This section relates to those patients NOT presenting with a discrete vascular pathology, but rather with neuromusculoskeletal cranio-cervical dysfunction suitable for OMT mobilisation, manipulation and exercise intervention. This assessment of risk and benefit relates to the risk associated with treatment, not misdiagnosis.
In the context of this Framework, there are two substantive, but related, risks:
- The risk of misdiagnosis of an existing vascular pathology
- The risk of serious adverse event following OMT
For instance, a patient presents with neck pain / headace but develop a serious adverse event, such as a dissection due to underlying pathology aggravated by treatment)
Risk
See the Risk and Benefit diagram to the right
Benefit
The benefits of OMT are reported in high-quality systematic reviews and meta-analyses by different authors[19][20][21][22]. OMT and exercise interventions are also included in the most recent Clinical Practice Guidelines linked to the International Classification of Functioning, Disability and Health[23]. The combination of OMT and exercise for neck pain and associated disorders like headache and radiculopathy have been proven to be effective[24][25].
Person-centred decision-making
From an individual level, based on the background literature which highlights various risk factors for specific pathologies in specific people, the epidemiological data must be contextualised in the specific patient encounter. This is also the case for decision-making regarding the choice of intervention and its predicted benefit. Accurate data to inform a precise level of risk at an individual level is lacking, so it is not possible to develop valid clinical prediction rules for risk nor benefit. Absolute risk judgement cannot be made by the physiotherapist and the therapist must accept that the clinical decision is made in the absence of certainty and a decision based on a balance of probabilities. When in doubt, consider not intervening, and assess the chance of recovery of pain and dysfunction (assuming a musculoskeletal dysfunction).
See page 25 of the Framework for a clinical reasoning flowchart for risk assessment prior to cervical manual therapy.
[edit | edit source]
Shared decision-making covers the professional and ethical obligations of informed consent but it surpasses informed consent by recognising the patients’ rights to make decisions about their care, ensuring they are adequately informed about treatment options and their consequences, providing patients with sufficient opportunity to discuss them and by jointly agreeing on a course of action for each individual (Moulton et al, 2013)[26]. The specific requirements of informed consent will vary from country to country according to local laws, regulatory expectations, customs and norms.
The Agency for Healthcare Research and Quality has proposed 5 steps based on the SHARE approach that will help facilitate the process of shared decision making with your patients. Follow this link if you want to learn more about this.
Further information on consent is provided in pages 27 and 28 of the Framework
Section 9: Safe OMT practice[edit | edit source]
You will find more information on this section on the related page: Section 9: Safe OMT practice, including emergency management of an adverse situation
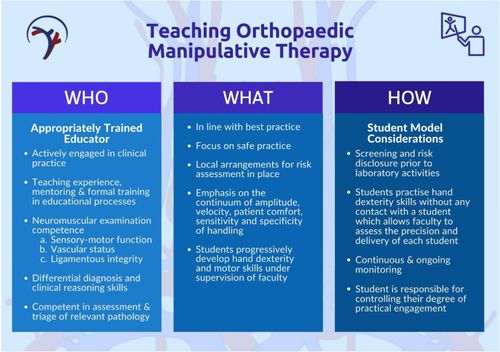
Section 10: Teaching OMT for the cervical region[edit | edit source]
You will find more information on this section on the related page: Section 10: Teaching OMT for the Cervical Region
References[edit | edit source]
- ↑ 1.0 1.1 Rushton A, Rivett D, Carlesso L, Flynn T, Hing W, Kerry R. International Framework for Examination of the Cervical Region for potential of vascular pathologies of the neck prior to Orthopaedic Manual Therapy (OMT) Intervention: International IFOMPT Cervical Framework. International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT). 2020
- ↑ 2.0 2.1 IFOMPT (2008). IFOMT Educational Standards Document. Available at: http://www.ifompt.com/Standards/Standards+Document.html Accessed December 2012
- ↑ Hutting, N., Kerry, R., Coppieters, M.W., Scholten-Peeters, G.G.M. (2018). Considerations to improve the safety of cervical spine manual therapy. Musculoskeletal Science and Practice, 33, 41-45.
- ↑ Hutting, N., Antonius, H., & Kerry, R. (2020). Yes, we should abandon pre-treatment positional testing of the cervical spine. Musculoskeletal Science and Practice, 49, 102181.
- ↑ Kranenburg, H.A., Schmitt, M.A., Puentedura, E.J., Luijcks, G.J., van der Schans, C.P. (2017). Adverse events associated with the use of cervical spine manipulation or mobilization and patient characteristics: A systematic review. Musculoskeletal Science and Practice, 28, 32-38.
- ↑ Rivett, D.A. (2004). Adverse effects of cervical manipulative therapy. In J.D. Boyling and G.A. Jull (Eds.), Grieve’s Modern Manual Therapy of the Vertebral Column (3rd ed) (pp 533-549). Churchill Livingstone: Edinburgh.
- ↑ IFOMPT (2016). Educational Standards In Orthopaedic Manipulative Therapy Document.
- ↑ Haynes RB, Devereaux PJ, Guyatt GH (2002). Physicians’ and patients’ choices in evidence based practice. British Medical Journal 324:1350-1351.
- ↑ Higgs J, Jones M (2000). Clinical Reasoning in the Health Professions, 2nd edn, Oxford, Butterworth Heinemann.
- ↑ Maitland G, Hengeveld E, Banks K, et al (Eds)(2005). Maitland's Vertebral Manipulation, 7th Edn, Elsevier Butterworth Heinneman, Edinburgh.
- ↑ Petty NJ (2011). Neuromusculoskeletal Examination and Assessment: A Handbook for Therapists (Physiotherapy Essentials), 4th edn, Churchill Livingstone, Elsevier, Edinburgh.
- ↑ Jones MA, Rivett DA (2004). Introduction to clinical reasoning. In M.A. Jones and D.A. Rivett (eds.), Clinical Reasoning for Manual Therapists. Butterworth-Heinemann: Edinburgh 3-24.
- ↑ Saiz, L.C., Gorricho, J., Garjón, J. (2017). Blood pressure targets for the treatment of people with hypertension and cardiovascular disease. Cochrane Database of Systematic Reviews, 10, CD010315.
- ↑ Pickett, C.A., Jackson, J.L., Hemann, B.A., Atwood, J.E. (2011). Carotid artery examination, an important tool in patient evaluation. Southern Medical Journal, 104(7), 526-532.
- ↑ Patel, R.R., Adam, R., Maldjian, C., Lincoln, C.M., Yuen, A., Arneja, A. (2012). Cervical carotid artery dissection: current review of diagnosis and treatment. Cardiology in Review, 20(3), 145-152. 38 |
- ↑ Elder, A., Japp, A., Verghese, A. (2016). How valuable is physical examination of the cardiovascular system? British Medical Journal, 354, i3309.
- ↑ 17.0 17.1 17.2 Rivett DA (2004). Adverse effects of cervical manipulative therapy. In J.D. Boyling and G.A. Jull (eds.), Grieve’s Modern Manual Therapy of the Vertebral Column (3rd ed). Churchill Livingstone: Edinburgh 533-549.
- ↑ 18.0 18.1 18.2 18.3 Taylor AJ, Kerry R (2010). A ‘system based’ approach to risk assessment of the cervical spine prior to manual therapy. International Journal of Osteopathic Medicine 13:85-93
- ↑ Gross, A., Langevin, P., Burnie, S.J. et al (2015). Manipulation and mobilisation for neck pain contrasted against an inactive control or another active treatment. Cochrane Database of Systematic Reviews, 23(9), CD004249.
- ↑ Lozano López, C., Mesa Jiménez, J., de la Hoz Aizpurúa, J.L. (2016). Efficacy of manual therapy in the treatment of tension-type headache: A systematic review from 2000-2013. Neurologia, 31(6), 357-69.
- ↑ Zhu, L., Wei, X., Wang, S. (2016). Does cervical spine manipulation reduce pain in people with degenerative cervical radiculopathy? A systematic review of the evidence, and a meta-analysis. Clinical Rehabilitation, 30(2), 145-155.
- ↑ Varatharajan, S., Ferguson, B., Chrobak, K., et al. (2016). Are non-invasive interventions effective for the management of headaches associated with neck pain? An update of the Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. European Spine Journal, 25(7), 1971-1999.
- ↑ Blanpied, P.R., Gross, A.R., Elliott, J.M., Devaney, L.L., Clewley, D., Walton, D.M., Sparks, C., Robertson, E.K. (2017). Neck pain: Revision 2017. Journal of Orthopaedic & Sports Physical Therapy, 47(7), A1-A83.
- ↑ Hidalgo, B., Hall, T., Bossert, J., Dugeny, A., Cagnie, B., Pitance, L. (2017). The efficacy of manual therapy and exercise for treating non-specific neck pain: A systematic review. Journal of Back and Musculoskeletal Rehabilitation, 30(6), 1149-1169.
- ↑ Fredin, K., Lorås, H. (2017). Manual therapy, exercise therapy or combined treatment in the management of adult neck pain - A systematic review and meta-analysis. Musculoskeletal Science and Practice, 31, 62-71
- ↑ Moulton, B., Collins, P.A., Burns-Cox, N., Coulter, A. (2013). From informed consent to informed request: do we need a new gold standard? Journal of the Royal Society of Medicine, 106(10), 391-394.