Foot and Ankle Assessment-Investigations and Tests: Difference between revisions
Kim Jackson (talk | contribs) m (Text replacement - "Category:Course Pages" to "Category:Course Pages Category:Physioplus Content") |
Rucha Gadgil (talk | contribs) No edit summary |
||
| Line 185: | Line 185: | ||
== References == | == References == | ||
<references /><br> | <references /><br> | ||
[[Category:Assessment]] | [[Category:Assessment]] | ||
[[Category:Foot]] | [[Category:Foot]] | ||
[[Category:Ankle]] | [[Category:Ankle]] | ||
[[Category:Ankle - Assessment and Examination]] | [[Category:Ankle - Assessment and Examination]] | ||
[[Category:Foot - Assessment and Examination]] | [[Category:Foot - Assessment and Examination]] | ||
[[Category:Musculoskeletal/Orthopaedics]] | [[Category:Musculoskeletal/Orthopaedics]] | ||
[[Category:Athlete Assessment]] | [[Category:Athlete Assessment]] | ||
[[Category:Sports Medicine]] | [[Category:Sports Medicine]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
Revision as of 09:22, 26 June 2021
Original Editor - Rachael Lowe
Top Contributors - Ewa Jaraczewska, Admin, Kim Jackson, Lucinda hampton, Samuel Adedigba, Nikhil Benhur Abburi, Jess Bell, Shejza Mino, Khloud Shreif, Rachael Lowe, Kai A. Sigel, Simisola Ajeyalemi, Rucha Gadgil, Wanda van Niekerk, Pinar Kisacik and Evan Thomas
Subjective (Patient Intake)[edit | edit source]
Patients may present to the clinic with foot and ankle problems for a variety of reasons which may include pain, swelling, deformity, stiffness, instability and/or abnormal gait.[1]
Patient Intake[edit | edit source]
- History of presenting complaint:
- Acute trauma? Insidious onset? Specific mechanism of Injury (if applicable)?
Special Questions (Region‐specific historical examination)[edit | edit source]
- Presence of back or leg pain? Is pain in a dermatomal region (i.e., pain in the foot and ankle can be referred from the back)
- Presence of hip or knee pain? (i.e., ankle pain can be referred from the hip or biomechanically affected by the ankle)
- Type of shoes, including wear pattern, age and proper design?[2]
Additional Information[edit | edit source]
- Medical history (PMH): pre-existing medical conditions?
- Drug history (DH): any relevant medications?
- Social history (SH): work/sports/hobbies affected?
Investigations[edit | edit source]
- Radiological Considerations: any previous radiographs or other medical imagingscans?
- Other investigations: recent blood tests?
Red Flags[edit | edit source]
Red flags are signs and symptoms found in the patient history and clinical examination that may be suggestive of serious pathology. If serious pathology is suspected, immediate referral to a medical doctor is indicated and your concerns should be noted.
Red flags specific to evaluation of the foot and/or ankle include:
- Bilateral pins and needles or numbness in the lower limb (LL)
- Bowel and bladder dysfunction (i.e., patient is unable to feel themselves while going to the toilet)
- Incontinence
- Paraesthesia in the groin region
- Loss of pulses in the LL (vascular compromise)
- Obvious deformity
- Positive Babinski sign
If serious pathology is not evident, but patient symptoms are more severe than anticipated, advice from an experienced therapist on whether an A&E referral is appropriate may be useful. It should be noted that the mechanism of Injury is a significant consideration. For example, if there was a force exerted through the leg, what was it and was it enough to result in a fracture of the tibia or femur? Loss of pulses in the foot may be indicative of vascular compromise.
Clinical Reasoning - What does the History tell you?[edit | edit source]
Gathering valuable information during the history provides the clinician with clues as to what structure is likely affected, further guiding the physical examination. Mechanism of injury is extremely important as it provides information on what forces went through what structure, and in what direction. This will further provide valuable information on what tissues/structures are likely stretched or damaged (I.e., a valgus force may indicate a deltoid ligament sprain, whereas a varus force may be suggestive of injury to the anterior tala-fibular ligament (ATFL) and/or calcaneofibular ligament (CFL).
The low back, as a source of ankle pain, should be ruled out (unless there is a clear mechanism of injury to the ankle), as the ankle can be a referred site of pain for both these areas. Immediate swelling and bruising usually indicates significant trauma and may require radiographs to rule out fractures or an MRI to investigate integrity of the ligaments.
The information gathered during the history should provide the clinician with a working hypothesis to take into the objective examination. The physical examination will be used to prove or disprove the working hypothesis.
Objective[edit | edit source]
The objective examination provides quantifiable measures to rule out what structures are involved as well as to reassess after treatment to track progress/deterioration.
General Observation (in standing)[edit | edit source]
- Posture - foot posture, arch posture
- Movement Patterns - calf flexibility (without subtalar joint/midfoot collapsing), see functional tests for others
- Gait Analysis - normal, walking on insides and outsides of feet, heel and toe-walk, tandem, running (particularly if running is an aggravating factor)
Functional Tests[edit | edit source]
- Small knee bend
- Sit to stand
- Squat
- Double heel raise
- Jump
- Single leg stand
- Single knee bend
- Single heel raise
- Hop
- Running
- Star Excursion Balance Test
Inspection & Palpation[edit | edit source]
Inspection
- Deformities: bunions, hammer toes, claw toes, calluses etc.
- Effusion
- Muscle Wasting
Palpation
- Joint lines
- Medial and lateral ligaments
- Achilles tendon, peronei and other extrinsic muscles
Neurologic Assessment[edit | edit source]
If neurological pathology or referral from lumbar spine is suspected, a neurological assessment should be performed.
Reflexes
- Patella Ligament (L3/L4)
- Achilles Tendon (S1/S2)
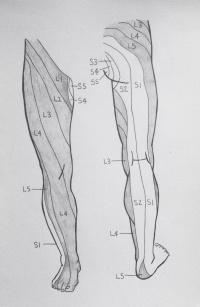
Dermatomes
- L1 to S4
Myotomes
- L2 - Hip flexion
- L3 - Knee extension
- L4 - Dorsiflexion
- L5 - Big toe extension OR 4 lesser toes extension
- L5/S1 - Knee flexion
- S1 - Plantar flexion OR foot eversion
- S2 - Toe flexion
Other neurological testing:
- Plantar response (also known as the Babinski response)
- Clonus
Vascular Assessment[edit | edit source]
If compromised circulation is suspected, the clinician should palpate to assess pulses of the dorsalis pedis artery. The state of the vascular system can also be assessed by the response of symptoms to positions of dependence and elevation of the lower limbs.
Movement Testing[edit | edit source]
- Full AROM + overpressure to clear the lumbar spine, hip and knee
- AROM + overpressure & PROM: ankle, subtalar joint, midfoot, forefoot and toes
- Specific joint mobility: test each individual joint with a glide and compare to contralateral side and to normal values
- Lower limb muscle strength and length: Specifically muscles of the calf, gluteal muscles, TFL and other hip flexors proximally
- If involvement of the lumbar spine is suspected, perform passive intervertebral mobilizations (PA spinous processes & PA transverse processes)
Special Tests[edit | edit source]
Special tests are utilized to prove or disprove the working hypothesis, as well as to identify dysfunctional structures/tissues. They include the following:
- Ottawa ankle rules (to determine if radiographs are indicated to rule out fracture)
- Ankle ligament stress tests
- Talar tilt test
- Anterior drawer of the ankle
- Eversion stress test
- Muscle tests (to assess functioning of the intrinsic & extrinsic muscles)
- Silfverskiöld test
- Squeeze test
- Windlass test
- Impingement sign ankle
- Navicular drop test
Biomechanical Evaluation[edit | edit source]
A foot assessment can be used to classify foot type as well as to identify possible etiological factors relating to injury in order to properly prescribe therapeutic interventions.
Details can be found on the Biomechanical Assessment of the Foot and Ankle page.