Femoral stress fracture
Original Editors - Matthias Verstraelen as part of the Vrije Universiteit Brussel's Evidence-based Practice project
Top Contributors - Matthias Verstraelen, Lucinda hampton, Kim Jackson, Redisha Jakibanjar, Admin, Daniele Barilla, Adam Vallely Farrell, Wanda van Niekerk, Daphne Jackson, Laura Ritchie, Evan Thomas, Naomi O'Reilly, WikiSysop, Elise Audiens and Claire Knott
Definition/Description[edit | edit source]
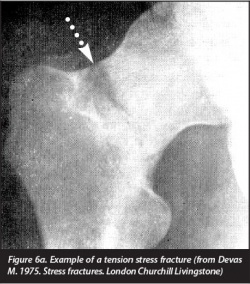
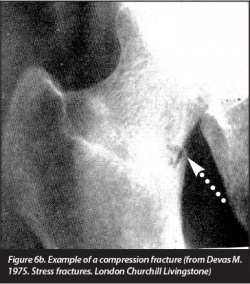
Stress fractures were first described in Prussian soldiers by Breithaupt in 1855. They were named “march fractures” and their characteristics were confirmed 40 years later with the advent of radiography.In 1958, Devas made the first report on stress fractures in athletes.[1]
Stress fractures are injuries that occur when repetitive and excessive stress on a bone is combined with limited rest. This leads to muscle weakness and a lower shock absorbing capacity of the leg[2][3][4][5][6].
Clinically Relevant Anatomy[edit | edit source]
Stress fractures of the femur can occur in the whole bone like the neck, shaft and the condyles.Femoral stress fractures mainly develop on the medial compression side of the femoral shaft, within the proximal and middle thirds of the bone. [8]The highest incidence is seen at the femoral neck. When the patient doesn’t adapt his or her training, certain stress fractures could lead to complications, even to the point of complete femoral fractures of the head or shaft [9][10].
Epidemiology/Etiology[edit | edit source]
Stress fractures are presented in athletes with the main focus on running or in military trainees[4]. The femoral ones are at a level 6% to 7% of all the stress injuries. Femoral stress fractures are seen in overtrainers but also in undertrainers [11]. With the decreased physical level of the population, it is possible that the incidence of femoral stress fractures will increase in the future [12].
Characteristics/Clinical Presentation[edit | edit source]
The risk factors are as follows: [13][2][3][14]
- High-intensity training
- Recreational runners
- Track and field, basketball, soccer, dance
- Women
- Poor nutrition and lifestyle activities
- Lower 25-hydroxyvitamin D
- Female athlete triad
- (history of) smoking
- < 3 times exercising/week
- > 10 alcoholic drinks/week
- Genetic factors [15] (CTR C allele, VDR C-A haplotype, LRP5 A-G-G-C, VDR C-A haplotype)
- Change of surfaces (indoor track, frozen field)
- Biomechanical imbalance (leg length, foot arch, forefoot varus, stance of foot and ankle)
There is a trend to significance for energy expenditure (kcal/day) with lower limb stress fractures (p=0.06). This effect could be explained as a sequence that more active people have also a higher expenditure level [16].
No significant effect is found of the ground reaction force on the incidence of lower-limb stress fractures (p>0.05) [3].
The incidence of femoral stress fractures is reduced with 14% (p=0.013) when a semi rigid insole is used [17].
Alana et al. concluded that there’s no effect on lower limb stress fractures and calcium intake (p=0.55) or bone density [16].
There is a trend to significance for energy expenditure (kcal/day) with lower limb stress fractures (p=0.06). This effect could be explained as a sequence that more active people have also a higher expenditure level [16].
Diagnostic Procedures[edit | edit source]
First of all we describe the possible symptoms: [14][4][18][5]
- Local pain and edema
- Point tenderness on palpation
- Local swelling
- Antalgic gait
- Painful and limited passive and active ROM of hip and/or knee (flexion, internal rotation, extension)
- Pain increases during activity
- Groin pain
- Bone marrow edema
Therapists have to pay attention to misdiagnose a femoral stress fracture as muscle strain of the quadriceps or illiopsoas tendinopathy because of the similar symptoms [19].
To present femoral stress fractures on images. We can use 4 modalities: plain radiography, bone scintigrapy, MRI and ultrasonography with the highest sensitivity and specificity for MRI [13]. These techniques can be used in different phases of diagnosis and treatment [13][15].
Classification of lower limb stress fracture [1][20][edit | edit source]
| Arendt scale (MRI based) | Federicson scale (MRI based) | Saxen classification | Torg classification (radiographic based) | |
|---|---|---|---|---|
| Location of use | Generic | Generic | Navicular | 5th Metatarsal base |
| Grade 1 | STIR signal change | Periosteal edema - bone marrow normal | Dorsal cortex involved | Acute fracture line, no intramedullary sclerosis or periosteal reaction |
| Grade 2 | STIR and T2 change | Periosteal and bone marrowedema - T2 change only | Dorsal cortex and body involved | Widened fracture line with intramedullary sclerosis and periosteal reaction |
| Grade 3 | STIR, T1 and T2 change - no fracture line present | Periosteal and bone marrow edema - T1 and t2 change - no fracture line | Dorsal and volar cortices uninvolved | Widened fracture line with complete intramedullary sclerosis and periosteal reaction |
| Grade 4 | STIR, T1 and T2 change - fracture line present | Periosteal and bone marrow edema - STIR, T1 and T2 change - fracture line | - | - |
*MRI: Magnetic resonance imaging; CT: Computed tomography; STIR: Short tau inversion recovery.
Examination[21]
The hop test and tuning fork test could be used as diagnostic test but there is a lack of recent evidence for their validity. Another test is the “fist” test, the therapist create a bilateral pressure on the anterior side of the femur starting at the distal part and moving to the proximal one. The most valid test for the diagnosis is the fulcrum-test, while the therapist pushes to the dorsum of the knee [18].
Physical Therapy Management[edit | edit source]
Initial treatment is based on the reduction of activities to a pain-free level. During this “relative rest”-period of 4 to 12 weeks, the patient can use pneumatic compression walking boots to reduce his pain level. Also, physical therapy and cross-training which contains of flexibility, strength and cardiovascular training is permitted for example swimming and biking. After that restriction period, the activities can be increased in a slow, graduated way [17].
Ivkovic et al. designed a new treatment algorithm for femoral shaft stress injuries. Four phases have to be fulfilled to start normal training and each phase is evaluated by a hop or fulcrum test. The first phase is called symptomatic, where the patient has to walk with crutches. The second phase is the asymptomatic one where patient are allowed to walk normally and to start swimming and exercises the upper extremity. During the third ‘basic’ phase the patient can perform exercises of lower and upper extremities. During the last ‘resuming phase’, the athlete is allowed to gradually start normal training [18]. No recurrence of injury after treatment and follow-up for 48-96 months [18].The treatment algorithm is free available in the article from Ivkovic et al.: "Stress fractures of the femoral shaft in athletes: a new treatment algorithm."
A triple-phase bone scan is recommended for an early diagnosis. It is very important to perform an adequate evaluation, patient history, and have a high index of suspicion. This will enable the practitioner to justify having a bone scan performed and thereby decrease the incidence of undiagnosed asymptomatic femoral shaft stress fractures. [23]
An early diagnosis is needed. Often, x-rays are not going to detect these injuries. Therefore, we must go through the appropriate referral channels to have a triple-phase bone scan ordered. One needs to maintain a high level of suspicion, especially if the athlete is experiencing persistent pain that shows no improvement with treatment.[23]
To prevent femoral stress fractures, people could modify their training schedules and wear shock-absorbing shoe inserts. Insoles lowers the incidence because the improves biomechanics, less fatigue and limit the impact on the ground. The size of these insoles can range in different types to support the forefoot and/or the toes [3][17]. Also calcium and vitamin D supplementation could play a role in the prevention but their data are controversial [17]. Leg muscle stretching during warm-up has no significant effect on prevention for femoral stress fractures[13].
Resources[edit | edit source]
- Pubmed, Web of Knowledge, Pedro
- Third edition, Examination of musculoskeletal injuries
- Second edition, Therapeutic exercise for musculoskeletal injuries
References[edit | edit source]
- ↑ 1.0 1.1 Astur DC, Zanatta F, Arliani GG, Moraes ER, Pochini AD, Ejnisman B. Stress fractures: definition, diagnosis and treatment. Revista brasileira de ortopedia. 2016 Feb;51(1):3-10.
- ↑ 2.0 2.1 Stress Fractures, information from your family doctor. Americain Family Physician Jan. 2011. Level of evidence: 5
- ↑ 3.0 3.1 3.2 3.3 Zadpoor A, Nikooyan A. The relationship between lower-extremity stress fractures and the ground reaction force: a systematic review. Clinical Biomechanics 2011; 26: 23 -28. (level of evidence 3A)
- ↑ 4.0 4.1 4.2 Niva M, Mattila V, Kiuru M, Pihlajamäki H. Bone stress Injuries are common in female military trainees. Clin Orthop Relat Res (2009) 467: 2962-2969. Level of evidence: 3A
- ↑ 5.0 5.1 Schultz, Houglum, Perrin. Third edition, examination of musculoskeletal injuries p.401. Human Kinetics. Level of evidence: 5
- ↑ Houglum P. Second edition, therapeutic exercise for musculoskeletal injuries p.80-81, p. 811-812. Human Kinetics. Level of evidence: 5
- ↑ 7.0 7.1 Devas, Michael. Stress fractures. Churchill Livingstone, 1975.
- ↑ Robertson GA, Wood AM. Lower limb stress fractures in sport: Optimising their management and outcome. World journal of orthopedics. 2017 Mar 18;8(3):242.
- ↑ Patel D, Roth M, Kapil N. Stress fractures: diagnosis, treatment and prevention. American Family Physician Jan. 2011; 83: 39-46. Level of evidence: 1A
- ↑ Zadpoor A, Nikooyan A. The relationship between lower-extremity stress fractures and the ground reaction force: a systematic review. Clinical Biomechanics 2011; 26: 23 -28. Level of evidence: 1B
- ↑ Kang L, Belcher D, Hulstyn M. Stress fractures of the femoral shaft in women’s college lacrosse: a report of seven cases and a review of the literature. Br J Sports Med 2005; 39: 902-906. Level of evidence: 2B
- ↑ Fredericson M, Jang K, Bergman G, Gold G. Femoral diaphyseal stress fractures: results of a systematic bone scan and magnetic resonance evaluation in 25 runners. Physical Therapy in Sport 5 (2004): 188-193. Level of evidence: 2B
- ↑ 13.0 13.1 13.2 13.3 Patel D, Roth M, Kapil N. Stress fractures: diagnosis, treatment and prevention. American Family Physician Jan. 2011; 83: 39-46. (Level of evidence 1A)
- ↑ 14.0 14.1 Anand A, Raviraj A, Kodikal G. Subchondral stress fractures of femoral head in healthy adult. Indian J Orthop. 2010 Oct-Dec; 44(4): 458-460. Level of evidence: 3B
- ↑ 15.0 15.1 Korvala J, Hartikka H, Pihlajamäki H, Solovieva S, Ruohola J-P, Sahi T, Barral S, Ott J, Ala-Kokko L, Männikkö M. Genetic predisposition for femoral neck stress fractures in military conscripts. BMC Genetics 2010, 11: 95. Level of evidence: 2B
- ↑ 16.0 16.1 16.2 Cline A, Jansen R, Melby C. Stress fractures in female army recruits: implications of bone density, calcium intake and exercise. Journal of the American College of Nutrition, Vol. 17; No. 2: 128-135 (1998). Level of evidence: 3A
- ↑ 17.0 17.1 17.2 17.3 Snyder R, De Angelis J, Koester M., Spindler K, Dunn W. Does shoe insole modification prevent stress fractures? A systematic review. HSSJ (2009) 5: 92-98. (Level of evidence 2B)
- ↑ 18.0 18.1 18.2 18.3 Ivkovic A, Bojanic I, Pecina M. Stress fractures of the femoral shaft in athletes: a new treatment algorithm. Br J Sports Med 2006; 40: 518-520. (Level of evidence 2A)
- ↑ Nguyen J, Peterson J, Biswal S, Beaulieu C, Fredericson M. Stress-related injuries around the lesser trochanter in long-distance runners. AJR 2008; 190: 1616-1620. Level of evidence: 3B
- ↑ Robertson GA, Wood AM. Lower limb stress fractures in sport: Optimising their management and outcome. World journal of orthopedics. 2017 Mar 18;8(3):242.
- ↑ Casterline M, Osowski S, Ulrich G. Femoral stress fracture. Journal of Athletic Training March 1996; 31: 53-56. Level of evidence: 4
- ↑ BJSM Videos. Stress fracture (fulcrum) test, with Mike Reiman. Available from: http://www.youtube.com/watch?v=8Dw3fNd5Szc [last accessed 25/01/14]
- ↑ 23.0 23.1 Mark Casterline, M. A. (March 1996). Femoral Stress Fracture. Journal Of Athletic Training, 55-56 (level of evidence 4).