Femoral Fractures: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editors ''' - [[User:Vanderpooten Willem|Willem Vanderpooten]] | <div class="editorbox">'''Original Editors ''' - [[User:Vanderpooten Willem|Willem Vanderpooten]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Search strategy == | == Search strategy == | ||
Keywords:<br>femur fracture, femoralis fracture, femoral fracture, Thomas traction, Hare traction, … | |||
Keywords:<br>femur fracture, femoralis fracture, femoral fracture, Thomas traction, Hare traction, … | |||
Databases searched:<br>PubMeb, Web of Science, Pedro, Emedicine, …<br> | Databases searched:<br>PubMeb, Web of Science, Pedro, Emedicine, …<br> | ||
== Definition/Description<br> == | |||
A femoral fracture is a fracture of the thigh bone. A femoral shaft fracture is defined as a fracture of the diaphysis occurring between 5 cm distal to the lesser trochanter and 5 cm proximal to the adductor tubercle. The femur is the largest ad strongest bone in the body and has a good blood supply, so it requires a large or high impact force to break this bone. There are 4 types of fracture: | |||
Type 1: stress fracture<br>Type 2: severe impaction fractures<br>Type 3: partial fracture<br>Type 4: completed displaced fracture | |||
[[Image: | This classification is for the severity of the fracture. | ||
Type 1: stress fracture <br>A stress fracture is a small crack in the bone. Stress fractures often develop from overuse, such as from high-impact sports. Most stress fractures occur in the weight-bearing bones. A stress fracture is an overuse injury. When muscles are overtired, they are no longer able to lessen the shock of repeated impacts. When this happens, the muscles transfer the stress to the bones. This can create small cracks or fractures. <ref name="AAOS">AAOS. Stress Fractures of the Foot and Ankle. 2009. (Available at http://orthoinfo.aaos.org/topic.cfm?topic=a00379, accessed 19 December 2014) fckLR(Level of evidence: 5)</ref><br> | |||
[[Image:Figuur 1.jpg]] | |||
Type 2: severe impaction fractures<br>An impacted fracture is a fracture in which the bone breaks into multiple fragments, which are driven into each other. It is a closed fracture that occurs when pressure is applied to both ends of the bone, causing it to split into two fragments that jam into each other. <ref name="WebMD">WebMD. Understanding Bone Fractures - the Basics. 2014. (Available at http://www.webmd.com/a-to-z-guides/understanding-fractures-basic-information, accessed 19 December 2014) fckLR(Level of evidence: 5)</ref> <br> | |||
[[Image:Figuur 2.jpg]] | |||
<br> | |||
Type 3: partial fracture<br>A partial fracture is an incomplete break of a bone. This type of fracture refers to the way the bone breaks. In an incomplete fracture the bone cracks but doesn’t break all the way through. In contrast there is the complete fracture, where the bone snaps into two or more parts.<ref name="Cleveland Clinic">Cleveland Clinic. Fractures. 2013. (Available at http://my.clevelandclinic.org/services/orthopaedics-rheumatology/diseases-conditions/hic-fractures, assessed 21 December 2014)fckLR(Level of Evidence: 5)</ref> <ref name="WebMD et al.">WebMD. Broken bone: types of fractures, symptoms and prevention. 2014. (Available at http://www.webmd.boots.com/a-to-z-guides/bone-fractures-types-symptoms-prevention, accessed on 21 december 2014)fckLR(Level of Evidence: 5)</ref> <br> | |||
[[Image:Figuur 3.jpg]] | |||
Type 4: completed displaced fracture<br>A bone has a displaced fracture when it breaks in two or more pieces and is no longer correctly aligned. Displacement of fractures is defined in terms of the abnormal position of the distal fracture fragment in relation to the proximal bone. <ref name="WebMD" /> <br>[[Image:Figuur 4.jpg]] | |||
Femor fractures can be located at three different places: | |||
<br>-Femoral head fracture<br>[[Image:Figuur 5.jpg]] | |||
<br> | |||
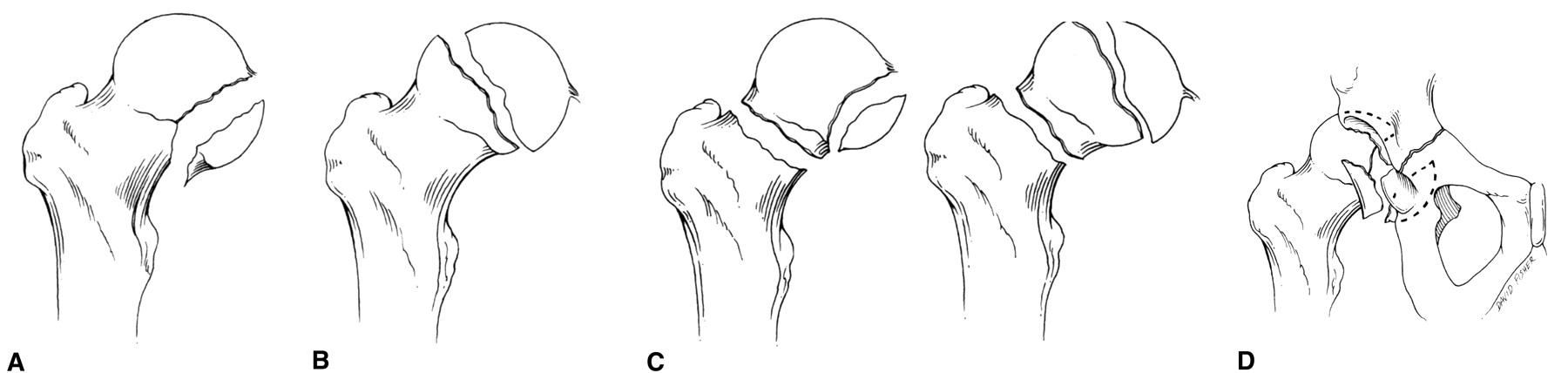
Head fractures: The Pipkin classification. <br>A: Type I, femoral head fracture inferior to the fovea centralis <br>B: Type II, fracture extended superior to the fovea centralis <br>C: Type III, any femoral head fracture with an associated femoral neck fracture<br>D: Type IV, any femoral head fracture with an associated acetabular fracture <br>[[Image:Figuur 6.jpg]]<br> | |||
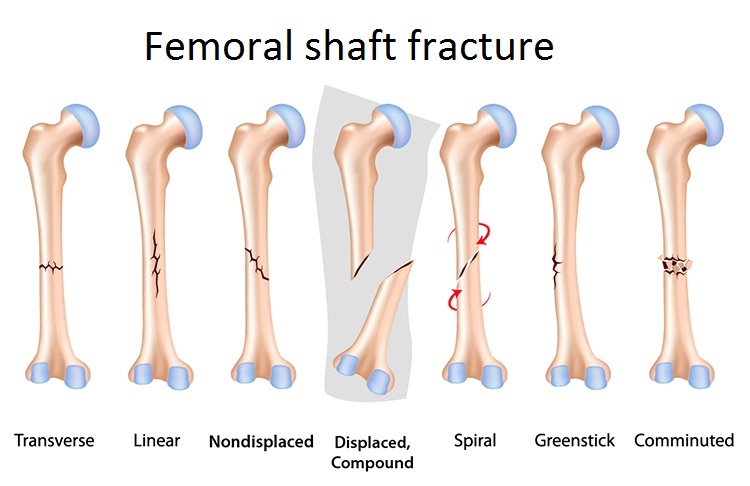
Femoral shaft fracture: <br> Keany (2013) describes 3 types of femoral shaft fractures as follows:<br> Type I - Spiral or transverse (most common)<br> Type II – Comminuted<br> Type III - Open <ref name="Keany et al.">Keany, J. et al. Femur fracture. 2013. (Available at http://emedicine.medscape.com/article/824856-overview, accessed 6 November 2014)</ref><br> | |||
[[Image:Enkel titel aangepast.jpg]]<br> | |||
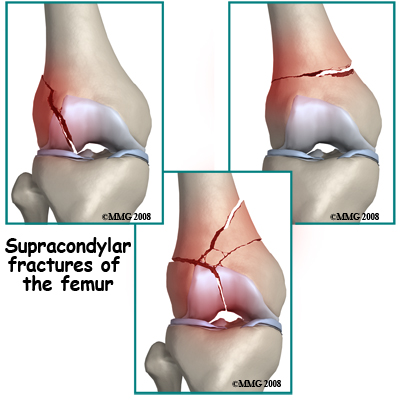
-Femoral condyle fracture | |||
[[Image:Figuur 7.jpg]] | |||
<br> | |||
== Clinically relevant anatomy == | == Clinically relevant anatomy == | ||
| Line 33: | Line 63: | ||
#Adductors: M adductor longus, M adductor brevis, M adductor longus, M pectineus, M gracilis | #Adductors: M adductor longus, M adductor brevis, M adductor longus, M pectineus, M gracilis | ||
#Abductors: M tensor fasciae latae | #Abductors: M tensor fasciae latae | ||
#Hamstrings: M biceps femoris, M semimembranosus, M semitendinosus | #Hamstrings: M biceps femoris, M semimembranosus, M semitendinosus | ||
#[[Image:Figuur 8.jpg]] | |||
<br> | |||
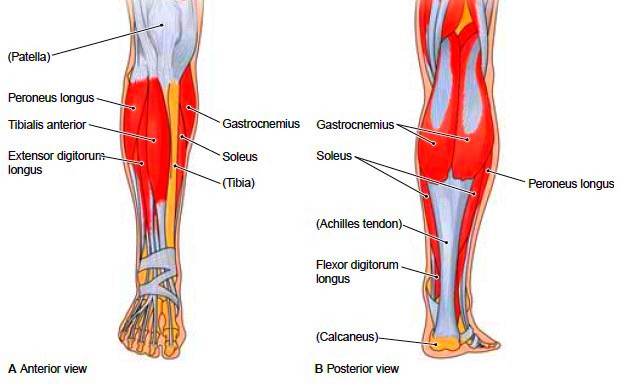
Several large muscles attach to the femur. Proximally, the gluteus medius and minimus attach to the greater trochanter, resulting in abduction of the femur with fracture. The iliopsoas attaches to the lesser trochanter, resulting in internal rotation and external rotation with fractures. The linea aspera (rough line on the posterior shaft of the femur) reinforces the strength and is an attachment for the gluteus maximus, adductor magnus, adductor brevis, vastus lateralis, vastus medialis, vastus intermedius, and short head of the biceps. Distally, the large adductor muscle mass attaches medially, resulting in an apex lateral deformity with fractures. The medial and lateral heads of the gastrocnemius attach over the posterior femoral condyles, resulting in [[Flexion deformity]] in distal-third fractures<ref name="Aukerman">Aukerman DF. Femur injuries and fractures. http://emedicine.medscape.com/article/90779-overview (accessed 30 October 2008)</ref>. | Following a femoral fracture, according to Keller et al., most of these muscles are much weaker than before, so physiotherapy is very important for muscle strengthening.<ref name="Keller et al.">Keller K. et al. Muscle atrophy caused by limited mobilisation. 2013.</ref> | ||
Several large muscles attach to the femur. Proximally, the gluteus medius and minimus attach to the greater trochanter, resulting in abduction of the femur with fracture. The iliopsoas attaches to the lesser trochanter, resulting in internal rotation and external rotation with fractures. The linea aspera (rough line on the posterior shaft of the femur) reinforces the strength and is an attachment for the gluteus maximus, adductor magnus, adductor brevis, vastus lateralis, vastus medialis, vastus intermedius, and short head of the biceps. Distally, the large adductor muscle mass attaches medially, resulting in an apex lateral deformity with fractures. The medial and lateral heads of the gastrocnemius attach over the posterior femoral condyles, resulting in [[Flexion deformity]] in distal-third fractures<ref name="Aukerman">Aukerman DF. Femur injuries and fractures. http://emedicine.medscape.com/article/90779-overview (accessed 30 October 2008)</ref>. Also the dysfunction or atrophy of the muscles such as abductors, iliopsoas, adductors, gastrocnemius and tensor fascia lata can be a initiating point leading to femoral shaft fracture. | |||
[[Image:Figuur 9.jpg]] | |||
<br> | |||
== Epidemiology/Etiology == | == Epidemiology/Etiology == | ||
Most femur fractures are the result of a high energy trauma, such as a motor accident, gunshot wound, or jump/fall from a height. A femoral fracture is a very serious injury and needs 3-6 months to heal. | |||
Several factors are related to increased risk of femoral fracture. Older persons (over 70) have a higher incidence of femoral fracture. Persons with [[Osteoporosis]] are also more likely to break their femur<ref name="Keany">Keany JE. Femur Fracture. http://emedicine.medscape.com/article/824856-overview (accessed 22 April 2009).</ref>.<br> | The incidence of femoral fractures is reported as 1-1.33 fractures per 10,000 population per year in the USA. In the United States and Europe the incidence of femoral fractures in children comprise 20 per 100,000 yearly.<ref name="Poolman et al.">Poolman, RW. et al. Pediatric femoral fractures: A systematic review of 2422 cases. 2006.</ref> In individuals younger than 25 years and those older than 65 years, the rate of femoral fractures is 3 fractures per 10,000 population annually<ref name="Aukerman" />. | ||
Several factors are related to increased risk of femoral fracture. Older persons (over 70) have a higher incidence of femoral fracture. A fracture of the proximal femoral is common in the elderly, with special emphasis on intracapsular (of the femoral neck) and extracapsular (trantrochanteric and subtrochanteric). Persons with [[Osteoporosis]] are also more likely to break their femur<ref name="Keany">Keany JE. Femur Fracture. http://emedicine.medscape.com/article/824856-overview (accessed 22 April 2009).</ref>.<br> | |||
Morbidity and mortality rates have been reduced in femoral shaft fractures, mainly as the result of changes in methods of fracture immobilization. Current therapies allow for early mobilization, thus reducing the risk of complications associated with prolonged bed rest. | Morbidity and mortality rates have been reduced in femoral shaft fractures, mainly as the result of changes in methods of fracture immobilization. Current therapies allow for early mobilization, thus reducing the risk of complications associated with prolonged bed rest. | ||
| Line 49: | Line 88: | ||
== Characteristics/Clinical presentation<br> == | == Characteristics/Clinical presentation<br> == | ||
A broken thigh bone is almost always very obvious. Signs of a fracture include severe pain, inability to move the leg or stand on it, and swelling. There individual may also be unable to bear weight, and apparent shortening of the affected leg may occur when the fracture is displaced. There may also be a resultant loss of blood in the femur, and a haematoma may be present in the surrounding soft tissue. | A broken thigh bone is almost always very obvious. Signs of a fracture include severe pain, inability to move the leg or stand on it, and swelling. There individual may also be unable to bear weight, and apparent shortening of the affected leg may occur when the fracture is displaced. There may also be a resultant loss of blood in the femur, and a haematoma may be present in the surrounding soft tissue. In case of an open fracture: open fractures have added potential for infection.<ref name="Keany et al." /> Also knee ligament injuries are common, such as lateral collateral ligament injuries or anterior cruciate ligament injury and must be assessed after fracture fixation.<ref name="Koval et al.">Koval, K., &amp; Zuckerman, J. et al. Handbook of Fractures. 2002; second edition. Levels of Evidence : 5</ref> | ||
== Complications<ref name="OrthoInfo">OrthoInfo. Femur Shaft Fractures. http://orthoinfo.aaos.org/topic.cfm?topic=A00521 (accessed 24 Jan 2015).</ref><br> == | == Complications<ref name="OrthoInfo">OrthoInfo. Femur Shaft Fractures. http://orthoinfo.aaos.org/topic.cfm?topic=A00521 (accessed 24 Jan 2015).</ref><br> == | ||
| Line 88: | Line 127: | ||
*Subtrochanteric fracture<ref name="Kisner">Kisner C, Colby LA. Therapeutic exercises: foundations and techniques. Philadelphia: F.A. Davis, 2012.</ref> | *Subtrochanteric fracture<ref name="Kisner">Kisner C, Colby LA. Therapeutic exercises: foundations and techniques. Philadelphia: F.A. Davis, 2012.</ref> | ||
Alternatively, patients who are not medically stable or nonambulatory may be treated with traction. | Alternatively, patients who are not medically stable or nonambulatory may be treated with traction. Applying a traction splint results in the reduction of hemorrhage. This is also one of the primary indications for applying these splints. The most common types of splints are the Thomas and Hare splint. Of which the Hare splint is more preferable because of the small application time. Femoral fractures need to be splinted during the initial phase. Those splints are needed to minimise pain and additional tissue damage.<br>These splints also have complications resulting from the use of traction splints including iatrogenic peroneal nerve injury, pressure sore development, ligamentous injury and pain. Even thought these complications research had advised to apply significant forces because they are necessary to obtain fracture reduction. <ref name="Daugherty et al.">Daugherty, M. et al. Significant Rate of Misuse of the Hare Traction Splint for Children with Femoral Shaft Fractures. Journal of Emergency Nursing. 2013.fckLR(Levels of Evidence : 2B)</ref><br>Surgical reduction and fixation should be performed within 24-48 of the injury. <br> | ||
{{#ev:youtube|-5hE0Ambr5A|300}} <br>Video Animation of Intramedullary Nail Fixation | |||
<br> | |||
Complications: | |||
Most common complications can occur during and after surgery, which are:<br>• Nerve injury <br>• Vascular injury <br>• Infection <br>• Refracture <br>• Non-union<br>• Malunion <br>• Fixation device failure <ref name="Koval et al." /><br> | |||
== Physical Therapy Management <br> == | == Physical Therapy Management <br> == | ||
| Line 98: | Line 141: | ||
Whilst in hospital, a therapist will teach the patient how to use a walking aid to allow them to mobilise, depending on their weight bearing status. The patient should be taught basic range of movement and strengthening exercises to maintain a degree of strength and reduce the risk of blood clots. | Whilst in hospital, a therapist will teach the patient how to use a walking aid to allow them to mobilise, depending on their weight bearing status. The patient should be taught basic range of movement and strengthening exercises to maintain a degree of strength and reduce the risk of blood clots. | ||
Surgical fixation and immobilization are followed by extensive physical therapy. After a femoral fracture, most of the muscles are much weaker than before so physiotherapy is very important. <br> | Surgical fixation and immobilization are followed by extensive physical therapy. Under extensive therapy can be understood that the patients who underwent a femur fracture should receive a treatment by a physiotherapist who will invest time in gait training. Gait training results in an increased bone formation. Even if gait training is completed using 30-50% of body weight support, an increase in bone formation could be found. <ref name="Carvalho et al.">Carvalho, D.C.L et al. Effect of treadmill gait on bone markers and bone mineral density of quadriplegic subjectshttp. 2006.</ref> After a femoral fracture, most of the muscles are much weaker than before so physiotherapy is very important. <br> | ||
The physiotherapist will begin with range of motion exercises for the hip, knee and ankle because mobility is decreased following immobilization. Mobilization is a very important treatment in the recovery process. The patient can also begin strengthening exercises based on the surgeon's orders (typically six weeks post-op). Patients should also undergo balance and proprioceptive rehab and these abilities are quickly lost with inactivity. <br> | The physiotherapist will begin with range of motion exercises for the hip, knee and ankle because mobility is decreased following immobilization. Mobilization is a very important treatment in the recovery process. The patient can also begin strengthening exercises based on the surgeon's orders (typically six weeks post-op). Patients should also undergo balance and proprioceptive rehab and these abilities are quickly lost with inactivity. <br> | ||
| Line 105: | Line 148: | ||
Knee: flexion and extension, abduction and adduction<br> Hip: flexion and extension, abduction and adduction, rotation <br> Functional quadriceps exercises should be initiated as soon as possible after the surgery because the quadriceps help provide stability in the knee. Flexion exercises also need to start as soon as possible, provided the fracture is adequated supported (i.e. the selected fixation approach allows for weight bearing). Physiotherapy should be continued until an acceptable functional range has been achieved or until a static position has been reached. It is necessary to record the range of movements in the knee with accuracy; first this should be done at weekly and then at monthly intervals. <br> | Knee: flexion and extension, abduction and adduction<br> Hip: flexion and extension, abduction and adduction, rotation <br> Functional quadriceps exercises should be initiated as soon as possible after the surgery because the quadriceps help provide stability in the knee. Flexion exercises also need to start as soon as possible, provided the fracture is adequated supported (i.e. the selected fixation approach allows for weight bearing). Physiotherapy should be continued until an acceptable functional range has been achieved or until a static position has been reached. It is necessary to record the range of movements in the knee with accuracy; first this should be done at weekly and then at monthly intervals. <br> | ||
During the postoperative treatment of patients with a proximal femoral fracture, physical therapy should focus on increasing the muscle strength, to improve walking safety and efficiency. Allowing the elderly patient to become more independent. | |||
Research indicates that strengthening the abductor and adductor muscles of the hip increase the laterolateral stability during walks. Resulting in an influence in the improvement of the patient’s dynamic balance.<ref name="Carneiro et al.">Carneiro, M. et al. Physical therapy in the postoperative of proximal femur fracture in elderly. Literature review. 2013. fckLR(Levels of evidence: 1A)</ref> | |||
Orthopaedic therapy:<br>During the immobilisation period of the therapists need to actively mobilise the foot, with or without weight. Another important aspect is the mobilisation through a hole in the plaster of the patellar bone. The use of isometric exercises are also important to train the muscles (quadriceps, hamstring & glutei) of the upper leg. After the immobilisation period it is necessary to fixate the leg manually or by using a brace. The fixation is needed for the re-education of hip and knee and to secure a progressively verticalisation of the leg and to make the patient independent while walking or during other activities. Also stabilisation exercises with unilateral support are recommended, but also balneotherapy. After the consolidation therapists need to focus on progressively increased pressure, the revalidation of the gait cycle, more intense mobilisation, strength-training therapy to reverse the muscle atrophy that occurred during the immobilisation period and condition training to increase the loss of endurance during the immobilisation period. | |||
Osteosynthesis:<br>Before going to bed, it is advised to massage the pre-articular structures and mobilisation of the hip. All mobilisation techniques can be used except rotations! It is also advised to use passive mobilisation techniques for retrieving the mobility of the patellar bone. The osteosynthesis is positively influenced by using isometric exercises of the hamstrings, quadriceps and glutei and the use of active exercises with low resistance to train the muscles of the hip and knee. The use of massage techniques of the quadriceps is advised straight after the verticalisation without support. The synthesis of the bone is also positively influenced by unilateral stabilisation exercises. After the consolidation period, orthopaedic therapy is recommended.<ref name="Xhardez et al.">Xhardez Y et al. Vade-mecum kinésithérapie et de reeducation fonctionnelle. 2002. fckLR(Levels of evidence: 5)</ref> | |||
As non-operative treatment there are 3 alternatives:<br>1. Skin traction: used in adults only for emergency fracture immobilisation in the field for patient comfort and to facilitate patient transport. Main disadvantage is the causing of slippage or skin necrosis when applying sufficient forces to the limb.<br>2. Skeletal traction: used for early fracture care before a definitive operative procedure can be performed. The goal is to restore the femoral length and to limit rotational and angular deformities. Skeletal traction may be applied through the distal femur or proximal tibia. Problems with skeletal traction include knee stiffness, limb shortening, prolonged hospitalisation, respiratory and skin aliments, and malunion. <br>3. Cast Brace: an external support device that permits progressive weight bearing by partially unloading the fracture through circumferential support of the soft tissues. Indications for cast bracing include open fracture, distal third fractures, and comminuted midshaft fractures of the femur. Proximal, simple transverse, or oblique fractures are less amendable to cast bracing due to high stress concentration and a propensity to angulate. The cast brace is best used after an initial period of skeletal traction. Consistently high rates of union, superior to 90%, usually by 13 to 14 weeks, have been reported in numerous studies. Problems with cast bracing include loss of reduction and subsequent malunion, shortening and angulation.<ref name="Keany et al." /><br> | |||
== Key Search == | |||
Carneiro, M. et al.Physical therapy in the postoperative of proximal femur fracture in elderly. Literature review. 2013. <br>Levels of evidence: 1A | |||
Koval, K., & Zuckerman, J. et al. Handbook of Fractures. 2002; second edition. <br>Levels of evidence: 5 | |||
Xhardez Y. et al. Vade-mecum kinésithérapie et de reeducation fonctionnelle. 2002. <br>Levels of evidence: 5<br>Daugherty, M. et al. Significant Rate of Misuse of the Hare Traction Splint for Children with Femoral Shaft Fractures. Journal of Emergency Nursing. 2013.<br>Levels of evidence: 2B<br>AAOS. Stress Fractures of the Foot and Ankle. 2009.<br>Level of evidence: 5 | |||
WebMD. Understanding Bone Fractures - the Basics. 2014. <br>Level of evidence: 5 | |||
Texas Orthopedic Spine Institute. Types of bone fractures. <br>Level of evidence: 5 | |||
WebMD. Broken bone: types of fractures, symptoms and prevention. 2014. <br>Level of evidence: 5 | |||
Cleveland Clinic. Fractures. 2013. <br>Level of Evidence: 5<br> | |||
== Resources == | |||
http://emedicine.medscape.com/article/90779-overview | |||
http://emedicine.medscape.com/article/824856-overview | |||
http://emedicine.medscape.com/article/824856-overview | |||
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3861999/ | |||
http://ac.els-cdn.com/S1878764914706291/1-s2.0-S1878764914706291-main.pdf?_tid=65bdb594-5516-11e4-8d24-00000aab0f01&acdnat=1413451721_842b7d8bdef872019e2b5a7408aca409/ | |||
http://www.sciencedirect.com/science/article/pii/S0099176712005454 | |||
http://apps.webofknowledge.com.ezproxy.vub.ac.be:2048/full_record.do?product=WOS&search_mode=Refine&qid=4&SID=S2zn1kgocpk8Xkj2bxO&page=1&doc=1 | |||
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0100-879X2006001000012&lng=en&nrm=iso&tlng=en | |||
http://orthoinfo.aaos.org/topic.cfm?topic=a00379 | |||
http://www.webmd.com/a-to-z-guides/understanding-fractures-basic-information | |||
http://www.houstonspineandjoint.com/bone-fracture-types.html | |||
http://www.webmd.boots.com/a-to-z-guides/bone-fractures-types-symptoms-prevention | |||
http://my.clevelandclinic.org/services/orthopaedics-rheumatology/diseases-conditions/hic-fractures | |||
http://www.ncbi.nlm.nih.gov/pubmed/23519955<br> | |||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
<div class="researchbox"> | <div class="researchbox"> | ||
<rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1TEH1tG6NHxr9l1EWHjKGcVEwYMfFCvp13XhEx4mxZBo8N4kW5|charset=UTF-8|short|max=10</rss> | <rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1TEH1tG6NHxr9l1EWHjKGcVEwYMfFCvp13XhEx4mxZBo8N4kW5|charset=UTF-8|short|max=10</rss> | ||
• femoral fractures; +16 new citations<br>• http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3861999/<br>• http://www.ncbi.nlm.nih.gov/pubmed/23519955<br> | |||
</div> | </div> | ||
== References == | == References == | ||
<references /> | <references /> | ||
<br> | <br> | ||
[[Category:Injury]] [[Category:Hip]] [[Category:Thigh]] [[Category:Bones]] [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | [[Category:Injury]] [[Category:Hip]] [[Category:Thigh]] [[Category:Bones]] [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | ||
Revision as of 21:28, 2 June 2016
Top Contributors - Kim Jackson, Vanderpooten Willem, Lucinda hampton, Admin, Vidya Acharya, Nupur Smit Shah, Jentel Van De Gucht, Rachael Lowe, Alex Palmer, Daphne Jackson, Margaux Jacobs, Aminat Abolade, Jason Coldwell, Lauren Lopez, 127.0.0.1, Evan Thomas and WikiSysop
Search strategy[edit | edit source]
Keywords:
femur fracture, femoralis fracture, femoral fracture, Thomas traction, Hare traction, …
Databases searched:
PubMeb, Web of Science, Pedro, Emedicine, …
Definition/Description
[edit | edit source]
A femoral fracture is a fracture of the thigh bone. A femoral shaft fracture is defined as a fracture of the diaphysis occurring between 5 cm distal to the lesser trochanter and 5 cm proximal to the adductor tubercle. The femur is the largest ad strongest bone in the body and has a good blood supply, so it requires a large or high impact force to break this bone. There are 4 types of fracture:
Type 1: stress fracture
Type 2: severe impaction fractures
Type 3: partial fracture
Type 4: completed displaced fracture
This classification is for the severity of the fracture.
Type 1: stress fracture
A stress fracture is a small crack in the bone. Stress fractures often develop from overuse, such as from high-impact sports. Most stress fractures occur in the weight-bearing bones. A stress fracture is an overuse injury. When muscles are overtired, they are no longer able to lessen the shock of repeated impacts. When this happens, the muscles transfer the stress to the bones. This can create small cracks or fractures. [1]
Type 2: severe impaction fractures
An impacted fracture is a fracture in which the bone breaks into multiple fragments, which are driven into each other. It is a closed fracture that occurs when pressure is applied to both ends of the bone, causing it to split into two fragments that jam into each other. [2]
Type 3: partial fracture
A partial fracture is an incomplete break of a bone. This type of fracture refers to the way the bone breaks. In an incomplete fracture the bone cracks but doesn’t break all the way through. In contrast there is the complete fracture, where the bone snaps into two or more parts.[3] [4]
Type 4: completed displaced fracture
A bone has a displaced fracture when it breaks in two or more pieces and is no longer correctly aligned. Displacement of fractures is defined in terms of the abnormal position of the distal fracture fragment in relation to the proximal bone. [2] 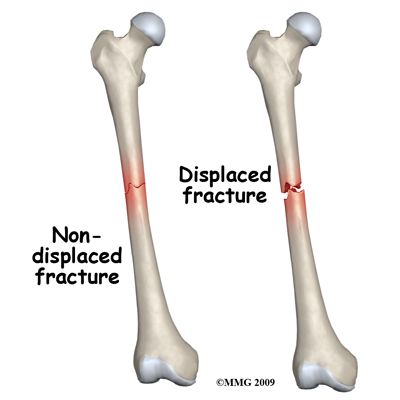
Femor fractures can be located at three different places:
Head fractures: The Pipkin classification.
A: Type I, femoral head fracture inferior to the fovea centralis
B: Type II, fracture extended superior to the fovea centralis
C: Type III, any femoral head fracture with an associated femoral neck fracture
D: Type IV, any femoral head fracture with an associated acetabular fracture 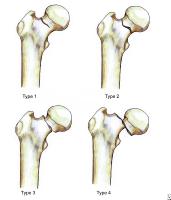
Femoral shaft fracture:
Keany (2013) describes 3 types of femoral shaft fractures as follows:
Type I - Spiral or transverse (most common)
Type II – Comminuted
Type III - Open [5]
-Femoral condyle fracture
Clinically relevant anatomy[edit | edit source]
Osteology
[edit | edit source]
The femur consists of a head, greater and lesser trochantor, shaft, and lateral and medial condyles with the patellar surface in between.
Musculature
[edit | edit source]
The femur is surrounded by different muscles: the quadriceps, the adductors, abductors and the hamstrings.
- Quadriceps: M rectus femoris, M vastus lateralis, M vastus medialis, M vastus intermedius
- Adductors: M adductor longus, M adductor brevis, M adductor longus, M pectineus, M gracilis
- Abductors: M tensor fasciae latae
- Hamstrings: M biceps femoris, M semimembranosus, M semitendinosus
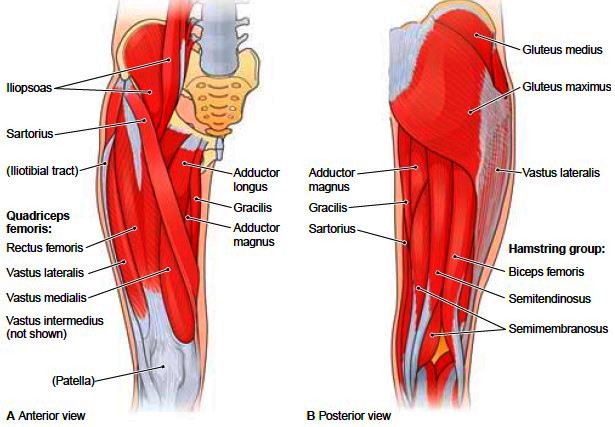
Following a femoral fracture, according to Keller et al., most of these muscles are much weaker than before, so physiotherapy is very important for muscle strengthening.[6]
Several large muscles attach to the femur. Proximally, the gluteus medius and minimus attach to the greater trochanter, resulting in abduction of the femur with fracture. The iliopsoas attaches to the lesser trochanter, resulting in internal rotation and external rotation with fractures. The linea aspera (rough line on the posterior shaft of the femur) reinforces the strength and is an attachment for the gluteus maximus, adductor magnus, adductor brevis, vastus lateralis, vastus medialis, vastus intermedius, and short head of the biceps. Distally, the large adductor muscle mass attaches medially, resulting in an apex lateral deformity with fractures. The medial and lateral heads of the gastrocnemius attach over the posterior femoral condyles, resulting in Flexion deformity in distal-third fractures[7]. Also the dysfunction or atrophy of the muscles such as abductors, iliopsoas, adductors, gastrocnemius and tensor fascia lata can be a initiating point leading to femoral shaft fracture.
Epidemiology/Etiology[edit | edit source]
Most femur fractures are the result of a high energy trauma, such as a motor accident, gunshot wound, or jump/fall from a height. A femoral fracture is a very serious injury and needs 3-6 months to heal.
The incidence of femoral fractures is reported as 1-1.33 fractures per 10,000 population per year in the USA. In the United States and Europe the incidence of femoral fractures in children comprise 20 per 100,000 yearly.[8] In individuals younger than 25 years and those older than 65 years, the rate of femoral fractures is 3 fractures per 10,000 population annually[7].
Several factors are related to increased risk of femoral fracture. Older persons (over 70) have a higher incidence of femoral fracture. A fracture of the proximal femoral is common in the elderly, with special emphasis on intracapsular (of the femoral neck) and extracapsular (trantrochanteric and subtrochanteric). Persons with Osteoporosis are also more likely to break their femur[9].
Morbidity and mortality rates have been reduced in femoral shaft fractures, mainly as the result of changes in methods of fracture immobilization. Current therapies allow for early mobilization, thus reducing the risk of complications associated with prolonged bed rest.
Characteristics/Clinical presentation
[edit | edit source]
A broken thigh bone is almost always very obvious. Signs of a fracture include severe pain, inability to move the leg or stand on it, and swelling. There individual may also be unable to bear weight, and apparent shortening of the affected leg may occur when the fracture is displaced. There may also be a resultant loss of blood in the femur, and a haematoma may be present in the surrounding soft tissue. In case of an open fracture: open fractures have added potential for infection.[5] Also knee ligament injuries are common, such as lateral collateral ligament injuries or anterior cruciate ligament injury and must be assessed after fracture fixation.[10]
Complications[11]
[edit | edit source]
Complications from the fracture:
- The sharp ends of the broken bone may lacerate blood vessels or nerves.
- Acute Compartment Syndrome may develop
- Increased risk of infection with open fractures as they expose the bone to the outside environment.
Complications from surgery:
- Infection
- Blood Clots (Deep Vein Thrombosis or Pulmonary Embolism)
- Damage to nerves or blood vessels
- Fat Embolism (Bone marrow enters the blood stream and can travel to the lungs)
- Malalignment of the bony fragments
- Delayed union or non-union
- Hardware Irritation (e.g. end of the nail or the screw can irritate the overlying muscles and tendons)
Examination[edit | edit source]
The Ottawa Knee Rules are a clinical tool that can be used to determine the need for radiography following knee injury based on the patient's presentation. Ante posterior and lateral x-rays (used to look for a break in the bone) views of the femur are typically obtained to confirm the fracture. X-ray views of the hip, the lower leg and the knee are also commonly reviewed to detect any associated injuries, because a femur fracture is almost associated with other traumatic injuries. For that reason a general physical examination should be included. Pain, swelling, deformity, abrasion, and protrusions should be noted.
Outcome Measures[edit | edit source]
Dynamic Gait Index
International Hip Outcome Tool (iHOT)
Lower Extremity Functional Scale (LEFS)
Timed Up and Go Test (TUG)
Medical Management
[edit | edit source]
Surgical reduction and fixation is indicated for the following types of proximal femur fractures:
- Intracapsular femoral neck fracture
- Dislocated femoral head
- Intertrochanteric fracture
- Subtrochanteric fracture[12]
Alternatively, patients who are not medically stable or nonambulatory may be treated with traction. Applying a traction splint results in the reduction of hemorrhage. This is also one of the primary indications for applying these splints. The most common types of splints are the Thomas and Hare splint. Of which the Hare splint is more preferable because of the small application time. Femoral fractures need to be splinted during the initial phase. Those splints are needed to minimise pain and additional tissue damage.
These splints also have complications resulting from the use of traction splints including iatrogenic peroneal nerve injury, pressure sore development, ligamentous injury and pain. Even thought these complications research had advised to apply significant forces because they are necessary to obtain fracture reduction. [13]
Surgical reduction and fixation should be performed within 24-48 of the injury.
Video Animation of Intramedullary Nail Fixation
Complications:
Most common complications can occur during and after surgery, which are:
• Nerve injury
• Vascular injury
• Infection
• Refracture
• Non-union
• Malunion
• Fixation device failure [10]
Physical Therapy Management
[edit | edit source]
Whilst in hospital, a therapist will teach the patient how to use a walking aid to allow them to mobilise, depending on their weight bearing status. The patient should be taught basic range of movement and strengthening exercises to maintain a degree of strength and reduce the risk of blood clots.
Surgical fixation and immobilization are followed by extensive physical therapy. Under extensive therapy can be understood that the patients who underwent a femur fracture should receive a treatment by a physiotherapist who will invest time in gait training. Gait training results in an increased bone formation. Even if gait training is completed using 30-50% of body weight support, an increase in bone formation could be found. [14] After a femoral fracture, most of the muscles are much weaker than before so physiotherapy is very important.
The physiotherapist will begin with range of motion exercises for the hip, knee and ankle because mobility is decreased following immobilization. Mobilization is a very important treatment in the recovery process. The patient can also begin strengthening exercises based on the surgeon's orders (typically six weeks post-op). Patients should also undergo balance and proprioceptive rehab and these abilities are quickly lost with inactivity.
Mobility exercises[edit | edit source]
Knee: flexion and extension, abduction and adduction
Hip: flexion and extension, abduction and adduction, rotation
Functional quadriceps exercises should be initiated as soon as possible after the surgery because the quadriceps help provide stability in the knee. Flexion exercises also need to start as soon as possible, provided the fracture is adequated supported (i.e. the selected fixation approach allows for weight bearing). Physiotherapy should be continued until an acceptable functional range has been achieved or until a static position has been reached. It is necessary to record the range of movements in the knee with accuracy; first this should be done at weekly and then at monthly intervals.
During the postoperative treatment of patients with a proximal femoral fracture, physical therapy should focus on increasing the muscle strength, to improve walking safety and efficiency. Allowing the elderly patient to become more independent.
Research indicates that strengthening the abductor and adductor muscles of the hip increase the laterolateral stability during walks. Resulting in an influence in the improvement of the patient’s dynamic balance.[15]
Orthopaedic therapy:
During the immobilisation period of the therapists need to actively mobilise the foot, with or without weight. Another important aspect is the mobilisation through a hole in the plaster of the patellar bone. The use of isometric exercises are also important to train the muscles (quadriceps, hamstring & glutei) of the upper leg. After the immobilisation period it is necessary to fixate the leg manually or by using a brace. The fixation is needed for the re-education of hip and knee and to secure a progressively verticalisation of the leg and to make the patient independent while walking or during other activities. Also stabilisation exercises with unilateral support are recommended, but also balneotherapy. After the consolidation therapists need to focus on progressively increased pressure, the revalidation of the gait cycle, more intense mobilisation, strength-training therapy to reverse the muscle atrophy that occurred during the immobilisation period and condition training to increase the loss of endurance during the immobilisation period.
Osteosynthesis:
Before going to bed, it is advised to massage the pre-articular structures and mobilisation of the hip. All mobilisation techniques can be used except rotations! It is also advised to use passive mobilisation techniques for retrieving the mobility of the patellar bone. The osteosynthesis is positively influenced by using isometric exercises of the hamstrings, quadriceps and glutei and the use of active exercises with low resistance to train the muscles of the hip and knee. The use of massage techniques of the quadriceps is advised straight after the verticalisation without support. The synthesis of the bone is also positively influenced by unilateral stabilisation exercises. After the consolidation period, orthopaedic therapy is recommended.[16]
As non-operative treatment there are 3 alternatives:
1. Skin traction: used in adults only for emergency fracture immobilisation in the field for patient comfort and to facilitate patient transport. Main disadvantage is the causing of slippage or skin necrosis when applying sufficient forces to the limb.
2. Skeletal traction: used for early fracture care before a definitive operative procedure can be performed. The goal is to restore the femoral length and to limit rotational and angular deformities. Skeletal traction may be applied through the distal femur or proximal tibia. Problems with skeletal traction include knee stiffness, limb shortening, prolonged hospitalisation, respiratory and skin aliments, and malunion.
3. Cast Brace: an external support device that permits progressive weight bearing by partially unloading the fracture through circumferential support of the soft tissues. Indications for cast bracing include open fracture, distal third fractures, and comminuted midshaft fractures of the femur. Proximal, simple transverse, or oblique fractures are less amendable to cast bracing due to high stress concentration and a propensity to angulate. The cast brace is best used after an initial period of skeletal traction. Consistently high rates of union, superior to 90%, usually by 13 to 14 weeks, have been reported in numerous studies. Problems with cast bracing include loss of reduction and subsequent malunion, shortening and angulation.[5]
Key Search[edit | edit source]
Carneiro, M. et al.Physical therapy in the postoperative of proximal femur fracture in elderly. Literature review. 2013.
Levels of evidence: 1A
Koval, K., & Zuckerman, J. et al. Handbook of Fractures. 2002; second edition.
Levels of evidence: 5
Xhardez Y. et al. Vade-mecum kinésithérapie et de reeducation fonctionnelle. 2002.
Levels of evidence: 5
Daugherty, M. et al. Significant Rate of Misuse of the Hare Traction Splint for Children with Femoral Shaft Fractures. Journal of Emergency Nursing. 2013.
Levels of evidence: 2B
AAOS. Stress Fractures of the Foot and Ankle. 2009.
Level of evidence: 5
WebMD. Understanding Bone Fractures - the Basics. 2014.
Level of evidence: 5
Texas Orthopedic Spine Institute. Types of bone fractures.
Level of evidence: 5
WebMD. Broken bone: types of fractures, symptoms and prevention. 2014.
Level of evidence: 5
Cleveland Clinic. Fractures. 2013.
Level of Evidence: 5
Resources[edit | edit source]
http://emedicine.medscape.com/article/90779-overview
http://emedicine.medscape.com/article/824856-overview
http://emedicine.medscape.com/article/824856-overview
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3861999/
http://www.sciencedirect.com/science/article/pii/S0099176712005454
http://orthoinfo.aaos.org/topic.cfm?topic=a00379
http://www.webmd.com/a-to-z-guides/understanding-fractures-basic-information
http://www.houstonspineandjoint.com/bone-fracture-types.html
http://www.webmd.boots.com/a-to-z-guides/bone-fractures-types-symptoms-prevention
http://my.clevelandclinic.org/services/orthopaedics-rheumatology/diseases-conditions/hic-fractures
http://www.ncbi.nlm.nih.gov/pubmed/23519955
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1TEH1tG6NHxr9l1EWHjKGcVEwYMfFCvp13XhEx4mxZBo8N4kW5|charset=UTF-8|short|max=10: Error parsing XML for RSS
• femoral fractures; +16 new citations
• http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3861999/
• http://www.ncbi.nlm.nih.gov/pubmed/23519955
References[edit | edit source]
- ↑ AAOS. Stress Fractures of the Foot and Ankle. 2009. (Available at http://orthoinfo.aaos.org/topic.cfm?topic=a00379, accessed 19 December 2014) fckLR(Level of evidence: 5)
- ↑ 2.0 2.1 WebMD. Understanding Bone Fractures - the Basics. 2014. (Available at http://www.webmd.com/a-to-z-guides/understanding-fractures-basic-information, accessed 19 December 2014) fckLR(Level of evidence: 5)
- ↑ Cleveland Clinic. Fractures. 2013. (Available at http://my.clevelandclinic.org/services/orthopaedics-rheumatology/diseases-conditions/hic-fractures, assessed 21 December 2014)fckLR(Level of Evidence: 5)
- ↑ WebMD. Broken bone: types of fractures, symptoms and prevention. 2014. (Available at http://www.webmd.boots.com/a-to-z-guides/bone-fractures-types-symptoms-prevention, accessed on 21 december 2014)fckLR(Level of Evidence: 5)
- ↑ 5.0 5.1 5.2 Keany, J. et al. Femur fracture. 2013. (Available at http://emedicine.medscape.com/article/824856-overview, accessed 6 November 2014)
- ↑ Keller K. et al. Muscle atrophy caused by limited mobilisation. 2013.
- ↑ 7.0 7.1 Aukerman DF. Femur injuries and fractures. http://emedicine.medscape.com/article/90779-overview (accessed 30 October 2008)
- ↑ Poolman, RW. et al. Pediatric femoral fractures: A systematic review of 2422 cases. 2006.
- ↑ Keany JE. Femur Fracture. http://emedicine.medscape.com/article/824856-overview (accessed 22 April 2009).
- ↑ 10.0 10.1 Koval, K., & Zuckerman, J. et al. Handbook of Fractures. 2002; second edition. Levels of Evidence : 5
- ↑ OrthoInfo. Femur Shaft Fractures. http://orthoinfo.aaos.org/topic.cfm?topic=A00521 (accessed 24 Jan 2015).
- ↑ Kisner C, Colby LA. Therapeutic exercises: foundations and techniques. Philadelphia: F.A. Davis, 2012.
- ↑ Daugherty, M. et al. Significant Rate of Misuse of the Hare Traction Splint for Children with Femoral Shaft Fractures. Journal of Emergency Nursing. 2013.fckLR(Levels of Evidence : 2B)
- ↑ Carvalho, D.C.L et al. Effect of treadmill gait on bone markers and bone mineral density of quadriplegic subjectshttp. 2006.
- ↑ Carneiro, M. et al. Physical therapy in the postoperative of proximal femur fracture in elderly. Literature review. 2013. fckLR(Levels of evidence: 1A)
- ↑ Xhardez Y et al. Vade-mecum kinésithérapie et de reeducation fonctionnelle. 2002. fckLR(Levels of evidence: 5)