Ependymoma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
== Definition == | == Definition == | ||
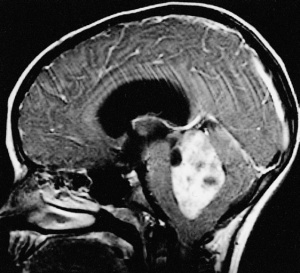
[[File:Ependymoma1.jpg|thumb|Ependymomas of the fourth ventricle.]] | [[File:Ependymoma1.jpg|thumb|Ependymomas of the fourth ventricle.]] | ||
Ependymomas are tumors of the central nervous system (CNS), which means that they originate in either the brain or spine. Tumors of glial cells are the most common and are | Ependymomas are tumors of the central nervous system (CNS), which means that they originate in either the brain or spine. Tumors of glial cells are the most common and are called gliomas. They occur in both adults and children but are most common in children. Tumors are classified by the World Health Organization (WHO) Classification of Tumors of the Nervous System as grades I, II, and III based on their grade of anaplasia (cell disorganisation)<ref name=":0">Cern-foundation.org. (2017). ''Ependymoma Basics | CERN Foundation''. [online] Available at: <nowiki>http://www.cern-foundation.org/education/ependymoma-basics</nowiki> [Accessed 24 Aug. 2017]. | ||
</ref> | </ref> | ||
| Line 33: | Line 33: | ||
==== Myxopapillary ependymoma (WHO grade I) ==== | ==== Myxopapillary ependymoma (WHO grade I) ==== | ||
This entity is characterised by cuboidal tumour cells, with GFAP expression and lack of cytokeratin expression, surrounding blood vessels in a mucoid matrix. Mitotic activity is very low or absent | This entity is characterised by cuboidal tumour cells, with GFAP expression and lack of cytokeratin expression, surrounding blood vessels in a mucoid matrix. Mitotic activity is very low or absent. | ||
==== Subependymoma (WHO grade I) ==== | ==== Subependymoma (WHO grade I) ==== | ||
Subependymoma has isomorphic nuclei in an abundant and dense fibrillary matrix with frequent microcysts; mitoses are very rare or absent | Subependymoma has isomorphic nuclei in an abundant and dense fibrillary matrix with frequent microcysts; mitoses are very rare or absent. | ||
==== Ependymoma (WHO grade II) ==== | ==== Ependymoma (WHO grade II) ==== | ||
This neoplasm has moderate cellularity; mitoses are rare or absent and nuclear morphology is monomorphic. Key histological features are perivascular pseudorosettes and ependymal rosettes | This neoplasm has moderate cellularity; mitoses are rare or absent and nuclear morphology is monomorphic. Key histological features are perivascular pseudorosettes and ependymal rosettes. Four histological variants have been described: cellular ependymoma, which has hypercellularity and increased mitotic rate, papillary ependymoma, clear cell ependymoma and tanycytic ependymoma. | ||
==== Anaplastic ependymoma (WHO grade III) ==== | ==== Anaplastic ependymoma (WHO grade III) ==== | ||
This tumour is characterised by hypercellularity, cellular and nuclear pleomorphism, frequent mitosis, pseudopalisading necrosis and endothelial proliferation. The latter two criteria do not appear to be independently related to prognosis | This tumour is characterised by hypercellularity, cellular and nuclear pleomorphism, frequent mitosis, pseudopalisading necrosis and endothelial proliferation. The latter two criteria do not appear to be independently related to prognosis. Perivascular rosettes are a histological hallmark.<ref>Reni, M., Gatta, G., Mazza, E. and Vecht, C. (2007). Ependymoma. ''Critical Reviews in Oncology/Hematology'', 63(1), pp.81-89. | ||
</ref> | </ref> | ||
== Management == | == Management == | ||
Many factors impact decisions about the treatment of ependymoma including the tumor location and grade, and the age of the person. Children and adults tolerate treatments differently, for that reason treatment for adults and treatment for pediatric patients may be very different.<ref name=":0" /> | |||
== | === Surgery === | ||
When possible, removing the tumour from the brain or spinal cord is a priority. A secondary goal of surgery is obtaining a biopsy of cancerous cells for diagnosis. | |||
=== Radiation Treatment === | |||
External beam radiation treatment is commonly used to treat ependymoma. Beams of X-rays, gamma rays or protons are aimed at the area of head or spine where the tumour is located. The treatment aims to kill cancer cell and shrink tumours. The treatments last several weeks. | |||
There are several methods of delivering radiation treatment: | |||
* Conformal radiotherapy | |||
* Intensity-modulated radiotherapy (IMRT) | |||
* Proton beam radiotherapy | |||
* Stereotactic radiosurgery (SRS) | |||
=== Chemotherapy === | |||
Chemotherapy is drug treatment for cancers or tumors. There are many types of drugs used to treat cancer. Traditionally cytotoxic agents designed to kill growing tumor cells are used. | |||
These agents often have side effects such as hair loss, nausea and vomiting and can cause a decrease in blood counts. | |||
add | == Differential Diagnosis == | ||
add text here relating to the differential diagnosis of this condition<br> | |||
== | == Key Evidence == | ||
* <br> | |||
== Resources == | |||
{| class="wikitable" | |||
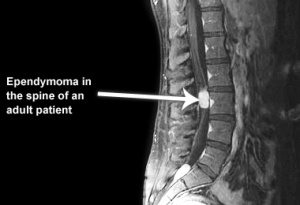
![[File:Ependymoma2.jpg|none|thumb]] | |||
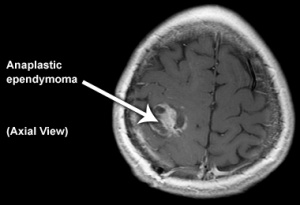
![[File:Ependymoma3.jpg|none|thumb]] | |||
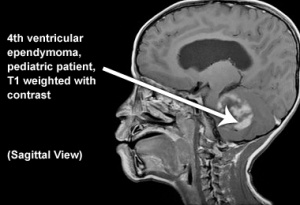
![[File:Ependymoma4.jpg|none|thumb]] | |||
|} | |||
== | == Case Studies == | ||
If you have a case study to report and you would like to contribute to Physiopedia, [[Contribute|please join]] and share your experiences.<br> | |||
== References == | |||
<references /> | <references /> | ||
Revision as of 21:13, 30 August 2017
Original Editor - George Prudden Lead Editors
Definition[edit | edit source]
Ependymomas are tumors of the central nervous system (CNS), which means that they originate in either the brain or spine. Tumors of glial cells are the most common and are called gliomas. They occur in both adults and children but are most common in children. Tumors are classified by the World Health Organization (WHO) Classification of Tumors of the Nervous System as grades I, II, and III based on their grade of anaplasia (cell disorganisation)[1]
Clinically Relevant Anatomy[edit | edit source]
Glial cells[edit | edit source]
Glial cells are a cell type that are found between nerve cells that share a general function of holding the CNS together. There are more glial cells than nerve cells and thereby constitute half of the total volume of the CNS. The four types of glial cells are: oligodenrocytes, microglia, epndymal cells and astrocytes.[2]
Ventricals[edit | edit source]
Ventricals and the central canal of the spinal cord are fluid-filled spaces within the CNS that contain cerebrospinal fluid. Both are common locations for tumours.[1]
Tentorium Cerebelli[edit | edit source]
Tentorium Cerebelli is an extension of the dura matter that separates the cerebellum from the inferior aspect of the occipital lobes. Tumour below the tentorium are called infratentorial and those above are called supratentorial.[1]
Pathological Process[edit | edit source]
Clinical Presentation[edit | edit source]
add text here relating to the clinical presentation of the condition
Diagnostic Procedures[edit | edit source]
Tumors are classified and graded according to their appearance when viewed through the microscope with the most severe tumour associated with a higher grade.
World Health Organization (WHO) Classification of Tumors of the Nervous System[edit | edit source]
Myxopapillary ependymoma (WHO grade I)[edit | edit source]
This entity is characterised by cuboidal tumour cells, with GFAP expression and lack of cytokeratin expression, surrounding blood vessels in a mucoid matrix. Mitotic activity is very low or absent.
Subependymoma (WHO grade I)[edit | edit source]
Subependymoma has isomorphic nuclei in an abundant and dense fibrillary matrix with frequent microcysts; mitoses are very rare or absent.
Ependymoma (WHO grade II)[edit | edit source]
This neoplasm has moderate cellularity; mitoses are rare or absent and nuclear morphology is monomorphic. Key histological features are perivascular pseudorosettes and ependymal rosettes. Four histological variants have been described: cellular ependymoma, which has hypercellularity and increased mitotic rate, papillary ependymoma, clear cell ependymoma and tanycytic ependymoma.
Anaplastic ependymoma (WHO grade III)[edit | edit source]
This tumour is characterised by hypercellularity, cellular and nuclear pleomorphism, frequent mitosis, pseudopalisading necrosis and endothelial proliferation. The latter two criteria do not appear to be independently related to prognosis. Perivascular rosettes are a histological hallmark.[3]
Management[edit | edit source]
Many factors impact decisions about the treatment of ependymoma including the tumor location and grade, and the age of the person. Children and adults tolerate treatments differently, for that reason treatment for adults and treatment for pediatric patients may be very different.[1]
Surgery[edit | edit source]
When possible, removing the tumour from the brain or spinal cord is a priority. A secondary goal of surgery is obtaining a biopsy of cancerous cells for diagnosis.
Radiation Treatment[edit | edit source]
External beam radiation treatment is commonly used to treat ependymoma. Beams of X-rays, gamma rays or protons are aimed at the area of head or spine where the tumour is located. The treatment aims to kill cancer cell and shrink tumours. The treatments last several weeks.
There are several methods of delivering radiation treatment:
- Conformal radiotherapy
- Intensity-modulated radiotherapy (IMRT)
- Proton beam radiotherapy
- Stereotactic radiosurgery (SRS)
Chemotherapy[edit | edit source]
Chemotherapy is drug treatment for cancers or tumors. There are many types of drugs used to treat cancer. Traditionally cytotoxic agents designed to kill growing tumor cells are used.
These agents often have side effects such as hair loss, nausea and vomiting and can cause a decrease in blood counts.
Differential Diagnosis[edit | edit source]
add text here relating to the differential diagnosis of this condition
Key Evidence[edit | edit source]
Resources[edit | edit source]
Case Studies[edit | edit source]
If you have a case study to report and you would like to contribute to Physiopedia, please join and share your experiences.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Cern-foundation.org. (2017). Ependymoma Basics | CERN Foundation. [online] Available at: http://www.cern-foundation.org/education/ependymoma-basics [Accessed 24 Aug. 2017].
- ↑ Palastanga, N., Field, D. and Soames, R. (2012). Anatomy and Human Movement: Structure and Function. 6th ed. Burlington: Elsevier Science.
- ↑ Reni, M., Gatta, G., Mazza, E. and Vecht, C. (2007). Ependymoma. Critical Reviews in Oncology/Hematology, 63(1), pp.81-89.