Degenerative Disc Disease: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 17: | Line 17: | ||
Dengenerative Disc Disease (DDD) is thought to begin with changes to the annulus fibrosis, intervertebral disc, and subchondral bone. The process of degeneration is divided into three classifications including: early dysfunction, intermediate instability, and final stabilization. | Dengenerative Disc Disease (DDD) is thought to begin with changes to the annulus fibrosis, intervertebral disc, and subchondral bone. The process of degeneration is divided into three classifications including: early dysfunction, intermediate instability, and final stabilization. | ||
Early dysfunction is the classifed as the beginning of degenerative changes which can occur as early as 20 years. Intermediate instability is classified by a loosening of the annulus fibrosis, which can cause back pain. Fibrosis to the posterior structure and formation of osteophytes denotes the final stabilization classification. Pain decreases, and motion descreases. <ref name=" | Early dysfunction is the classifed as the beginning of degenerative changes which can occur as early as 20 years. Intermediate instability is classified by a loosening of the annulus fibrosis, which can cause back pain. Fibrosis to the posterior structure and formation of osteophytes denotes the final stabilization classification. Pain decreases, and motion descreases. <ref name="1">Dutton M. Orthopaedic Examination, Evaluation, and Intervention. 2nd ed. New York, NY: McGraw-Hll; 2008.</ref> | ||
| | ||
Revision as of 11:05, 26 June 2013
Original Editor - Amanda E Davidson and Colby Boers, Lisa Pernet
Top Contributors - Lisa Pernet, Gaëlle Vertriest, Admin, Vanbeylen Antoine, Amanda E Davidson, Garima Gedamkar, Candace Goh, Uchechukwu Chukwuemeka, Laura Ritchie, Scott Cornish, Kim Jackson, WikiSysop, 127.0.0.1, De Maeght Kim, Lucinda hampton, Aya Alhindi and Eric Robertson
Definition/Description[edit | edit source]
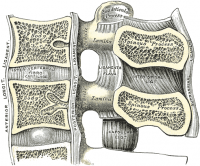
Degenerative disc disease or discopathy occurs when the discs (shock absorbers) cartilage between the bones of the spine, subjected to a process of degeneration that causes the disc to lose height and hydratation. The disc can’t fulfill his function anymore and it usually causes pain. It occurs naturally in most people over the years and is a part of the aging process.
The discopathy may develop at any level of the spine, but is most common in the cervical and lower lumbal segments. These are the transitions between mobile (cervical, lumbal) and fixed (thoracal, sacral) sections of the spine.[1][2]
Clinically Relevant Anatomy[edit | edit source]
Dengenerative Disc Disease (DDD) is thought to begin with changes to the annulus fibrosis, intervertebral disc, and subchondral bone. The process of degeneration is divided into three classifications including: early dysfunction, intermediate instability, and final stabilization.
Early dysfunction is the classifed as the beginning of degenerative changes which can occur as early as 20 years. Intermediate instability is classified by a loosening of the annulus fibrosis, which can cause back pain. Fibrosis to the posterior structure and formation of osteophytes denotes the final stabilization classification. Pain decreases, and motion descreases. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Epidemiology /Etiology[edit | edit source]
Degenerative disc disease refers to a condition in which the involved disc causes LBP. Lumbar degenerative disc disease is usually the result of a twisting injury to the lower back, such as when a person swings a golf club or rotates to put an object on a surface to the side of or behind them.[3]
The pain is also frequently caused by simple wear and tear on the spine and comes with the general aging process.
Degenerative disc disease is fairly common, and it is estimated that at least 30% of people aged 30-50 years old will have some degree of disc space degeneration, although not all will have pain or ever receive a formal diagnosis.[3]
The process that leads to DDD begins with structural changes. The annulus fibrosis (outer portion of the disc) loses water content over time which will make it increasingly unyielding toward everyday stress and strain on the spine. The loss of compliance in the discs contributes to forces being redirected from the anterior and middle portions of the facets to the posterior aspect, thus causing facet arthritis. Another result is hypertrophy of the vertebral bodies adjacent to the degenerating disc. The overgrowths are known as bony spurs (or osteophytes.)
Characteristics/Clinical Presentation[edit | edit source]
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
|
DDD commonly occurs with other diagnoses such as:
- idiopathic low-back pain
- lumbar radiculopathy
- myelopathy
- lumbar stenosis
- spondylosis
- osteoarthritis
- zygapophydeal joint degeneration [4]
Activities that typically increase pain include:
- Sitting for extended periods of time
- Rotating, bending, or lifting
- Activities that typically decrease pain include:
- Changing positions often
- Lying down
- Staying active Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Differential Diagnosis[edit | edit source]
People with DDD will have low back painCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title; however there are varying levels of severity. Pain is often chronic, but one with DDD can experience varying episodes of exacerbation where pain levels are elevatedCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
There are different degrees of annular disruption[1]. We can classify them into 4 grades, at which grade 0 is added. We differentiate these grades by means of a contrast medium injection.
- Grade 0: no disruption
- Grade 1: the contrast medium passes into the cartilage endplate through tear
- Grade 2: the contrast medium flows into the bony endplate
- Grade 3: the contrast medium is going into the cancellous bone of vertebra under endplate
- Grade 4: the contrast medium leaks completely in the cancellous bone.
Diagnostic Procedures[edit | edit source]
Provocation discography is a diagnostic test to identify a painful disc. To evaluate the degree of disruption, a combination of discogram and CTscan afther discography is used.[1]
Xray findings are used to diagnose DDD. Anterior-Posterior and lateral views are taken; presence of osteophytes, narrowing of the disc joint space, or a “vacuum sign” is noted. [5]
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
add text here related to physical examination and assessment
Patients may present with a history of Chronic LBP, and can experience symptoms into the buttock. They may also state a history of spine stiffness that gets worse with activity and tenderness with palpation over involved area. [5]
Medical management
[edit | edit source]
The preferential treatment for patients with chronic low back pain, caused by disc degeneration, is a conservative method consisting of physical therapy and medications (O'Halloran, 2007 (D)). [6]
Conservative treatment (home or hospital) includes rest, adequate program for motoractivity, regime of physical activity, strengthening of musculature, analgetic medication, physiotherapy, rehabilitation programs and lifestyle adjustments such as weight loss. [7]
Medications such as non-steroidal anti-inflammatories (e.g., ibuprofen, naproxen, COX-2 inhibitors) and pain relievers like acetaminophen (such as Tylenol) help many patients feel good enough to engage in regular activities. Stronger prescription medications such as oral steroids, muscle relaxants or narcotic pain medications may also be used to manage intense pain episodes on a short-term basis, and some patients may benefit from an epidural steroid injection. Not all medications are right for all patients, and patients will need to discuss side effects and possible factors that would preclude taking them with their physician. Epidural steroid injections can provide low back pain relief by delivering medication directly to the painful area to decrease inflammation.
Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Lately, successful outcomes were demonstrated by animal experiments with mesenchymal stem cells.[7][1]
Surgical intervention includes disc arthroplasty and lumbar spinei[1][7] fusion to reduce chronic low back pain due to degenerative disc disease.[8]
Physical management[edit | edit source]
A part of the physical therapy treatment is aimed at reducing pain. For this purpose, different physical modalities are used, including heat and cold application, traction, spinal manipulations (Beattie P, 2008 (D); Zhang Y (C), 2008; Mirza SK, 2007 (A1)), exercise programs and electrical stimulation such as ‘TENS’ and ‘pulsed radiofrequency (PRF)’ treatment.[9] With this PRF treatment, 56% of 76 patients with discogenic pain had more than 50% pain reduction one year after the first treatment.
Other objectives are to enhance the core stability by strengthening and improving the coordination between the abdominal and back muscles through a spinal stabilization program (Brox JI, 2003 (A2)). These stabilization exercises can increase the patient’s capacity to resist higher loads in the degenerative discs(Beattie P, 2008 (D)). A posterior dynamic stabilization program proved a significant improvement in pain and disability.[10][11]
In patients with degenerative disc disease it is also advised to add behavioral therapy to the usual treatment since it has been shown that the addition of behavioral therapy gives better results (Brox JI, 2003 (A2)). This is related to the fact that the diagnosis of degenerative disc disease also entails many psychological effects. Many patients assume that degeneration means that their spine is becoming weaker, associated with constant pain. These erroneous thoughts often cause fear of movement (kinesiophobia) and lead to the avoidance of movements of the spine (Beattie P, 2008 (D)).
The task of the physical therapists includes giving information and advice to improve the compliance rate.(Mirza SK, 2007 (A1)). Good communication with patients is of great importance, they have to realize that degeneration of the intervertebral disc is a normal aging process. The physiotherapist must help the patients to identify and overcome their fears and to adapt their coping strategies (Mirza SK, 2007 (A1)). It is important that patients understand that they must stay active and that activities of daily life and other moderate physical activity will not cause additional damage or have adverse effects (Brox JI, 2003 (A2)). Patients must be encouraged to perform low impact aerobic exercises, such as walking and water aerobics. Low impact aerobic conditioning ensures adequate flow of nutrients and blood to spine structures, and decreases pressure on the discs. They should avoid prolonged static postures as much as possible (Beattie P, 2008 (D); Brox JI, 2003 (A2)).
Extension exercises are given to displace the pressure on the discus intevertebralis anteriorly. Some exercises are:
- Hollow the back
- Make a sphinx posture
- Lie with the upper body prone on a table, the legs hang off. Lift the legs against the force of gravity. This is a back strengthening exercise.
- The last exercise can also be carried out on a ball.[12][13][11]
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10 </div>
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 Peng B., Pathophysiology, diagnosis, and treatment of discogenic low back pain, World J Orthop 2013 April 18; 4(2): 42-52fckLRLEVEL OF EVIDENCE=1
- ↑ Dr Vanaclocha V., et al, Degeneratieve ziekte van het disc, Clinica Neuros Neurochirurgie, 2010fckLR(http://neuros.net/nl/algemene_degenerative_ziekte_van_disc.php)fckLRLEVEL OF EVIDENCE=5
- ↑ 3.0 3.1 Ullrich, P. F. (2006 11 6). Lumbar Degenerative Disc Disease. Retrieved 06 02, 2009, from Degenerative Disc Disease: http://www.spine-health.com/conditions/degenerative-disc-disease/lumbar-degenerative-disc-disease
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedDutton - ↑ 5.0 5.1 Thompson, J.C. MD. Netter's Concise Atlas of Orthopaedic Anatomy. (2002) Saunders Elsevier. p.36-7
- ↑ O'Halloran DM, Pandit AS. Tissue-engineering approach to regenerating the intervertebral disc. Tissue Eng 2007; 13(8):1927-1954.
- ↑ 7.0 7.1 7.2 Drazin D., Rosner J., Avalos P., Acosta F., Stem cell therapy for degenerative disc disease, Advances in orthopedics, volume 2012, 8pg LEVEL OF EVIDENCE = 1
- ↑ Phillips F.M., Slosar P.J., Youssef J.A., Andersson G., Papatheofanis F., Lumbar spine fusion for chronic low back pain due to degenerative disc disease, SPINE Volume 38, Nr 7, Pp. E409-E422, 2013 LEVEL OF EVIDENCE = 1
- ↑ Rohof O., Intradiscal pulsed radiofrequency application following provocative discography for the management of degenerative disc disease and concordant pain: a pilot study, Pain practice, 2012, Volume 12, Issue 5, Pg 342-349 LEVEL OF EVIDENCE 2
- ↑ Zagra A., et al; Prospective study of a new dynamic stabilisation system in the treatment of degenerative discopathy and instability of the lumbar spine, Eur Spine J, 2012, 21, suppl 1: S83-S89 LEVEL OF EVIDENCE 2
- ↑ 11.0 11.1 Canbay S., et al, Posterior dynamic stabilization for the treatment of patients with lumbar degenerative disc disease: long-term clinical and radiological results, Turkish Neurosurgery 2013, vol. 23, No. 2, 188-197 LEVEL OF EVIDENCE 2
- ↑ Extremiteiten, www.fysio.net, Extensieoefening voor de lumbale wervelkolom in buikligging, 29-10-2009 (http://www.youtube.com/watch?v=SNamjanZttM&feature=youtube_gdata) LEVEL OF EVIDENCE = 5
- ↑ Kielbaso J., Hardcore abs training, Fit4Less4Info, 19oktober2012 (http://fit4lessamsterdam.wordpress.com/2012/10/) (http://fit4lessamsterdam.files.wordpress.com/2012/10/crunchleg-raise.jpg) LEVEL OF EVIDENCE = 5