Congenital and Acquired Neuromuscular and Genetic Disorders
Top Contributors - Clem Nihill, Sean Lewis, Shaimaa Eldib, Kim Jackson, Christine Mitchell, Kimberley Foy, James Millar, Alannah Henderson, Laura Ritchie, Mande Jooste, 127.0.0.1, Rucha Gadgil, Lucinda hampton, Tarina van der Stockt, Admin, Scott Buxton, Evelin Milev, WikiSysop, Evan Thomas and Mila Andreew
Introduction[edit | edit source]
The realisation that your child has a congenital or acquired disability can be a daunting and fearful situation[1]. There are many support networks and resources available however which aim to help and assist parents and carers in the development of that child.
Giving birth to a child with such disorders can happen to any mother regardless of age, racial or cultural heritage, socioeconomic status, health or lifestyle. According to the WHO, congenital anomalies or birth defects affect one in every 33 infants every year worldwide and result in approximately 3.2 million birth defect related disabilities every year1.
What is Congenital and Acquired?[edit | edit source]
A congenital disorder is one which exists at birth and very often before birth. It also can include those conditions which develop within the first month of birth. Congenital disorders vary widely in causation and abnormalities and can be as a result of genetic or chromosomal abnormalities, infection, birth trauma or the environment the fetus was in whilst in the uterus.
Acquired disorders on the other hand develop after birth and can develop over the course[2] of one’s life.
Resource Aims[edit | edit source]
Understanding how a disorder affects a child’s future health, abilities and lifestyle requirements is very commonly a priority for parents very soon after the birth of that child. The aim of this wiki resource is to provide guidance and information to parents of children with congenital and acquired neuromuscular and genetic disorders. This resource is not designed to provide and exhaustive list of disorders as there are very many. It will include those disorders which are most commonly found in the UK in terms of rates of incidence.
The authors aim to provide information in layman’s terms without clinical jargon. Where the use of such jargon may occur, small popups with explanations are provided when users hover over the terms.
Learning Outcomes[edit | edit source]
- Discuss the management strategies for children with congenital and acquired neurological disorders
- Describe and evaluate the current physical activity guidelines for those with congenital and acquired neurological disorders and the evidence underpinning them
- Identify support networks and relevant resources for severe and/or long term neurological conditions
Conditions[edit | edit source]
Cerebal Palsy[edit | edit source]
Overview[edit | edit source]
Cerebral Palsley is a general term for chronic NON-PROGRESSIVE neurological conditions that affect your childs ability to move and to maintain posture and balance (Geralis & Ritter 1991). This is due to damage to the areas of the brain that control movement and co-ordination. This damage to the brain can occur before, during or after birth. A child with CP will find they are not able to control some muscles in their body in the normal way.
It is estimated that 1 in 400 babies in the UK have a type of CP. (cerebralpalsy.org.uk)
Every case of cerebral palsy is unique to the individual this is due to the type and timing of injury to the developing brain
Signs & Symptoms
NHS.uk
Usually appear before a child is 3 years old.
These include:
- Muscle stiffness/ deformities
- Floppiness
- Weakness
- Exaggerated reflexes
- Epilepsy
- Uncontrolled movement
- Problems with balance & co-ordination
- Speech, visual, hearing and perceptual problems
- There may be learning difficulties
Classification of CP by limbs affected
- Monoplegic – one limb is affected
- Diplegic/paraplegic- both lower limbs are affected
- Triplegic- 3 limbs are affected
- Hemiplegic- one side of the body affected, same arm as leg
- Tetraplegic/quadriplegic – affects all 4 limbs and the torso. Likely to be some respiratory complications and difficulties eating.
Types of CP
- Spastic – abnormal control of voluntary limb muscles. Muscles are stiff and sometimes permanently contracted. Reflexes may be exaggerated. This is the most common form of CP occurring in 70-80% of people affected. (early support 2012)
- Athetoid/Dyskenetic- slow irregular writhing movements tend to occur at the end of limbs, may also be jerky and quick
- Ataxic - lack of balance or poor ability to perform smooth co-ordinated voluntary movements
- Mixed - does not fit into one category may have different types of movement disorders at the same time.
Other terms and language
There are a number of other words you may here to describe CP
These include:
Hypertonia- high muscle tone leading to stiffness
Hypotonia- low muscle tone which leads to floppiness
Dystonia – muscle tone fluctuates between floppy and stiff
Rigidity – Sustained stiffness of limbs
Spasm – involuntary contraction of a muscle
Tremor – rhythmic uncontrolled, repetitive movements
Minimal or mild CP – Little obvious physical impairment but children experience poor coordination and clumsiness. This can be associated with learning difficulties. (Early Support 2012)
Whilst CP is chronic it is manageable. Management will largely depend on the severity of problems. Many people with CP lead independent lives and not everyone will require physiotherapy. If your child is diagnosed with Cerebral Palsy they will likely have a team of people looking after them which will include: Doctors, Nurses, Pharmacists, Occupational Therapists, Dieticians and Physiotherapists.
Physiotherapists play a key role in supporting children and adults with CP (CSP 2014) website.
Management[edit | edit source]
Physiotherapy Management
Physiotherapists’ main aims are to help a child be as mobile and independent as possible. They also help encourage parents and carers to be involved and are happy to give support and advice on managing problems associated with CP.
Physiotherapy can help with stiffness or hypotonia, areas of inactivity, poor control of movement patterns, muscle shortening, contractures and prevention of musculoskeletal deformities. (kids physiotherapy.co.uk)
Physiotherapy treatment may involve stretches, strengthening exercises, facilitation of normal movement patterns, advice on postural management, and ways to clear secretions. Physiotherapists also give advice on aids and equipment which may be useful for sitting, standing, walking and getting children involved in everyday activities.
The Physiotherapist will complete a physical assessment and may also ask questions about the pregnancy and birth and any other relevant information. Treatment is designed to focus on capabilities not limitations. Physiotherapists will create a specific program and set goals with you that are tailored to your child’s needs.
Caring for anyone with CP can be overwhelming and difficult at times. Physical therapy can help the child to overcome or adapt to certain physical difficulties. This can help take some pressure of the parents/carers as the child becomes more independent.
Infant years
Goal setting with family
Feeding and carrying techniques
Symmetry limit abnormal movements, midline play
Encourage development of functional skills & play
Sensory motor development
Respiratory
Through School
Some children benefit from a programme at nursery and school. Community physiotherapists can visit your child during school or nursery. This is important because physiotherapists play an important role in training teachers for managing children with CP. (Mahon & Cusack 2002).
Orthotics
These are external devices which are often required to keep joints working properly in upper and lower limbs. They can help improve walking, decrease contracture and increase endurance. They also help to reduce trips or falls. They are made from a variety of materials with some very fashionable patterns now. They are generally slid or strapped on with Velcro.
Medical and surgical management
There are lots of different medications for CP which can help to reduce symptoms and help with any complications. Drug therapy is used to help control body movements, prevent seizures, relax muscles, and manage pain and many other associated problems.
When choosing which drugs the Consultants or Doctors will consider the benefits and side effects. Doctors will discuss the medications with you answering any questions or concerns you may have. It is often a process of trial and error for which drug will work best because everyone is different. The medications will be regularly monitored.
The most common medications used to treat CP include these categories:
Anticholinergics- For uncontrolled body movements
Anticonvulsants- seizure medication
Antidepressants- depression medication
Antispastic- muscle relaxers
Anti-inflammatories- pain management
Stool softeners
Surgery
Surgery may be used to correct problems with bones and joints or muscles and tendons. This tends to be used if there is pain on moving. This can also help to improve the child’s confidence, posture and ability to cope with everyday life. After surgery an intensive course of physiotherapy will often be required.
An example of a surgery used for children who suffer from severe stiffness in their legs is a SELECTIVE DORSAL RHIZOTOMY. This may only be used after other treatments have failed. It involves cutting some nerves in the spinal column which can help to reduce the stiffness experienced. Extensive physiotherapy will be needed after this type of operation. This will help the child to re-learn how to control their leg muscles.
What can you do?[edit | edit source]
Educate yourself so you can help prepare you and your child for the future. Part of a physiotherapists job is to educate so don’t be scared to ask questions. Develop support systems, involve family if you can and seek out other parents with children who have CP. Resources are not always easy to find but can make a massive difference. Ask healthcare professionals and other parents or guardians what support and services they use. Try to involve your child in a wide variety of programmes to support their skills and social development. (Canchild 2009).
Whilst your child is important remember to take care of yourself. (Canchild 2009). If you have a partner make time for them and work together raising your child. Be honest about how you feel, it is normal to feel angry, guilty, worried and scared. Ask for help when you need it.
How to your keep your kid active
Keeping active is vitally important for children. Studies have shown that children with various disabling diseases and conditions still benefit from being active. (Damiano 2006) Just because your child has CP doesn’t mean they can’t be active or get involved in sports and recreation programs. Encourage your child and let them try different activities until they find one they enjoy. Try to find solutions to the problems.
Physiotherapists can give you advice and information about special classes or sports specifically for children with CP. This can help your child and you, they will meet other children similar to them and you can speak to parents who are going through similar situations.
Activity can help:
- Improve muscle strength
- Improve endurance
- Improve overall health (for heart and lungs)
- Give them more confidence
- Improve social skills
- Become more independent
Muscular Dystrophy[edit | edit source]
Overview[edit | edit source]
Muscular Dystrophy (MD) is a group of inherited conditions that have a steady degenerative progression . It causes muscles to become weak over time . The muscle weakness begins in the legs most often . Some forms of this disease can affect the heart and lungs, which can create life-threatening complications. It is caused by a mutation in the genes responsible for muscle structure, which interferes with the child’s ability to function. As the disease progresses, the level of disability becomes worse. Both boys and girls can be affected by muscular dystrophy, however some affect boys predominantly, such as Duchenne’s muscular dystrophy (DMD).
There are many types of muscular dystrophy. Each is classified based on their presentation
| Type | Prevalence | Common Symptoms |
|---|---|---|
| Duchenne Muscular Dystrophy | 1 in 3,500 | • Difficulty walking, running or jumping • Difficulty standing up • Learn to speak later than usual • Unable to climb stairs without support • Can have behavioural or learning disabilities |
| Facioscapulohumeral Muscular Dystrophy | 1 in 7,500 | • Sleeping with eyes slightly open • Cannot squeeze eyes shut tightly • Cannot purse their lips |
| Myotonic Dystrophy | 1 in 8000 | • Muscle stiffness • Clouding of the lens in the eye • Excessive sleeping or tiredness • Swallowing difficulties • Behavioural and learning disabilities • Slow and irregular heartbeat |
| Becker Muscular Dystrophy | Varies; 1 in 18,000 – 1 in 31, 000 |
• Learn to walk later • Experience muscle cramps when exercising |
| Limb-Girdle Muscular Dystrophy | Estimated to be in a range of 1 in 14,500 – 1 in 123,000 | • Muscle weakness in hips, thighs and arms • Loss of muscle mass in these same areas • Back pain • Heart palpitations / irregular heartbeats |
| Oculopharyngeal Muscular Dystrophy | 1-9 in 100,000 | • Does not usually appear until age 50-60 • Dropped eyelids • Trouble swallowing • Gradual restriction of eye movement • Limb weakness, especially around shoulders and hips |
| Emery-Dreifuss Muscular Dystrophy | 1 in 100,000 | • Develop symptoms in childhood and adolescence • Muscle weakness • Trouble on stairs • Tendency to trip • Slow, irregular heartbeat |
Duchenne’s muscular dystrophy (DMD) is the most common type, and therefore will be the focus of the rest of this section.
Duchenne’s is almost exclusively seen in boys, however girls are carries of the condition. The gene which results in DMD has been found on the X chromosome that the boy receives from his mother. If the mother is a carrier of this mutated gene, the son has a 50% chance of developing DMD.
Signs & Symptoms
There are no abnormalities seen at birth and any symptoms usually begin when the child starts walking . Children with DMD generally have delayed motor milestones when compared with other children, for instance they begin walking around 18 months. These children also have difficulty sitting and standing independently . The disease becomes even more apparently between 4 and 5 years of age when the child is tripping and stumbling often and has trouble keeping up with other children.
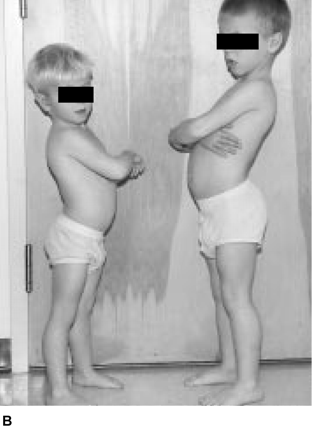
Weakness of the child’s calf muscles and the muscles back of the thigh early in the condition cause the child to stand with a more pronounced curve in their lower back. They do this in order to maintain balance as their center of gravity has shifted. This way of standing gives the child maximal support at both the hip and the knee.
The child stands with their legs further apart to give themself a broader base of support. This contributes to the child developing an altered walking pattern referred to as a waddling gait.
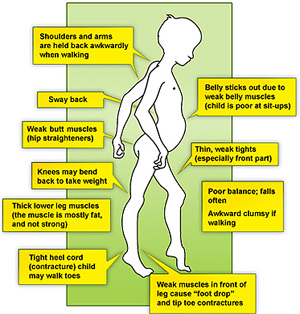
In this gait pattern, children walk on their toes with feet apart to help maintain balance, with an increased curve in the lower back. Contractures are a classic finding in DMD. It develops when tissues, such as muscle fibers, which are normally stretchy are replaced by hardened, non-stretchy tissue. They are seen as a major cause of disability . They prevent normal movement, and, for children with DMD, occur often in the legs, especially the calf and muscles around the hip.
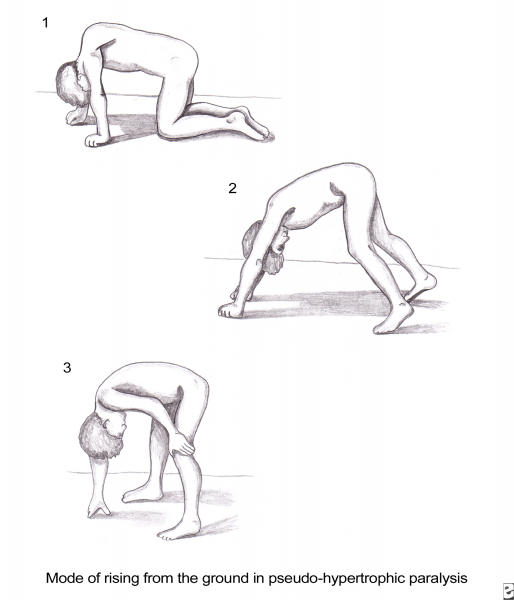
Gower’s Sign is a very common physical finding for boys with Duchenne’s . It involves using their hands to ‘climb’ up their legs in order to stand up. It is due to a weakness in the child’s hip muscles.
Boys with DMD may also suffer from behavioural or mental deficits, but this is not always the case . Any such impairments are not progressive meaning they will not get worse over time . Delayed language milestones may be an early warning sign of DMD and the child may need to work with a speech and language therapist to overcome these difficulties.
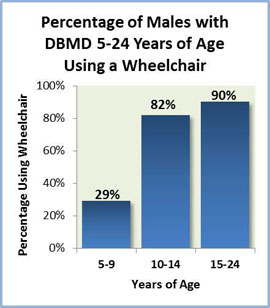
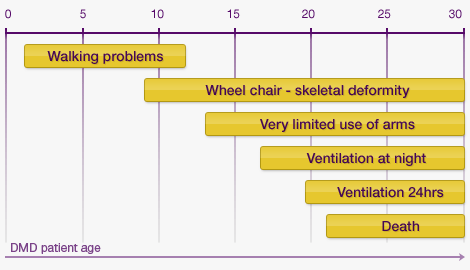
Between the ages of 6-11, there is a steady decline in muscle strength and by the age of 12 most children are wheelchair bound . There are further complications surrounding children being dependent on wheelchairs, such as scoliosis and respiratory problems .
Youtube video emedded here https://www.youtube.com/watch?v=AF4D4TyE9NM
Management[edit | edit source]
Medical Management
Sadly, there is no cure for Duchenne’s, but there are ways to help improve the individual’s quality of life and provide help for the stage they are in.
Mobility aids will be given to help the child be as independent as possible. This can include a walker in the beginning phases and can progress to a motorized wheelchair. In-home hoists are useful for the carers when they need help to transfer the child. Standing frames also become useful when the child can no longer stand on their own. This helps the child gain the benefits of standing, such as increased bone density, and stretching the muscles even if the child cannot stand on their own . Knee-ankle-foot orthosis may be used as well. They have been found to prolong the child’s independent mobility . These should be used alongside the mobility aids, such as a zimmer frame . Below, you can find more information about the various equipment options available to you.
Link to mobility aids sections
Staying as active as possible is recommended. Bedrest can make the muscle weakening worse3. Recommended physical activities and ways to help keep your child active will be discussed below.
Steroids are commonly prescribed for children with DMD, and are the only palliative treatment . Steroids have been shown to increase the child’s muscle strength and their functional ability . Steroids may help delay the child becoming wheelchair dependent28. However, there are side effects and you may wish to speak to your GP regarding steroid prescription. Another group of medications that has been shown to be helpful are Beta-Blockers . Heart and respiratory function slowly decline in these children and these drugs are used to help manage both these problems . Again, speak to your GP about these drugs and when they may need to be administered.
Some families may consider surgery for their child. Common surgeries for Duchenne’s boys include foot surgery, insertion of a feeding tube and spinal surgeries to correct a scoliosis, which may occur from being wheelchair dependent . There are many facts to consider before surgery, such as the effect general anesthesia has on the cardiac and respiratory systems, which are already compromised in children with DMD . Families need to weigh the advantages of the surgery with the risk before making a decision. For example, evidence has been found that surgery to correct scoliosis has improved respiratory function , and it also improves the cosmetic appearance and comfort of the child, however depending on the child’s cardiac and respiratory function there may be concerns about how anesthesia will affect them.
Physiotherapy Management
Physiotherapy is essential to the management of Duchenne’s. It is important to monitor the physical symptoms of the condition and physiotherapy can help keep the child active for as long as possible. Physiotherapists will work with the parents and carers and provide them with information and manual skills that will be helpful for the child.
Contractures are one of the major side effects that a physiotherapist will address. They will do these through a stretching routine, which can also be taught to the parents .
Physiotherapists will also be responsible for advising the parents on any orthoses, such as AFOs, and referring them with a paediatric orthotist . They will also help families choose what mobility aids and equipment the child might need.
In the early stages of the condition, the physiotherapist will be involved in helping keep the child active. During later stages of the condition, the physiotherapist will help more with respiratory issues as well.
Physiotherapists will monitor the child’s posture in sitting, lying and standing . They can inform the parents of ways to help the child sit, stand and lie in optimal positions using pillows or splints. A sleep system and night splints may be recommended for nighttime to help maintain the child’s posture over a long period of time.
Many physiotherapists use the NorthStar Amulatory Assessment in order to objectively monitor the child’s progression. Initiated in 2003, it is a tool designed specifically for children with DMD and has the child perform up to 17 activities, including standing, head-raising, hopping and running . This assessment is used only for children who are still able to walk. It is standardized with each child given the same instructions and their ability given a score of 0-2 . It is easy to administer and can be completed in approximately 10 minutes. These are useful when consulting with other medical practitioners and letting them know where the child is physically.
What can you do?[edit | edit source]
It is important for children with Duchenne’s to remain active . Being physically active will contribute to the child’s health and feelings of well being, as well as helping the development of their sensory motor skills . Weight bearing will help improve bone density and strength, which is important for children with DMD as their bones tend to be osteoporotic41. Inactivity is common in this population, not only due to the effects of the condition40. The increased effort needed for any activity, the fear of falling and the use of mobility aids are also factors contributing in inactivity40. It is important to encourage activity, but not to the point of fatigue37. In the early stage when the child is still walking independently, they need to be encouraged to participate in a variety of activities. Swimming and hydrotherapy are a great way for children to use and stretch their muscles without the influence of gravity . It also has a positive social aspect as it allows them to participate with other children in a way they are unable to on land . The warm water relaxes muscles, which helps when stretching37. Bike riding, so long as they have the balance to stay on, is also beneficial for children with Duchenne’s41. Like swimming, it allows the child to keep up with his friends and experience feeling like a normal child.
In later stages, physical activity may be more limited, but is still important for the child to do what they can. Again, swimming and hydrotherapy is a good way for the child to get out of the wheelchair and be able to move. It also helps improve the ability of the lungs, which these individuals struggle with in the later stage43. Biking outdoors may not be an option due to decreased balance and physical ability, but static recliner biking is still an option and allows the child to still be active within a supervised setting.
The child’s ability to be active changes again when they become fully wheelchair dependent. They are still able to be active through hydrotherapy. It is important during this time to monitor respiratory function and equipment may be used to help improve lung function, such as intermittent positive pressure breathing and inceptive spirometry . A practical way to incorporate breathing activities into a daily routine is by encourage the child to play a wind instrument or join a singing group. For younger children, encouraging them to blow bubbles aids respiratory function.
Along with all of these things, a stretching programme is very important in order to delay the development on contractures and must be done at all stages of the condition. Using weights to exercise should be avoided as this could lead to overworking the muscle and could cause further damage.
Charcot-Marie-Tooth disease
[edit | edit source]
Overview
[edit | edit source]
Charcot-Marie-Tooth disease (CMT) is known as a hereditary motor and sensory neuropathy (HMSN) and is the most common inherited neuromuscular disease with a prevalence of approximately 1 in every 2,500 (Reilly et al. 2011). CMT involves the degeneration of nerve fibres in the body that results in muscle weakness and wasting along with a decrease in sensation (Pareyson and Marchesi 2009; LaFarge et al. 2014).
Causes
CMT is caused by genetic mutations with approximately 1000 mutations in 80 genes that are related to the physical presentation of the disease. The diagnosis and classification of CMT is a very complicated process (Pareyson and Marchesi 2009).The two main types are Type I which is known as demyelinating CMT and Type II which is known as axonal CMT(Reilly et al. 2011). More information regarding the specifics about the different gene mutations can be found here (NHS choices- Causes).
Signs & Symptoms
The signs and symptoms of CMT are extremely variable between each different type due the extensive amount of different mutations possible. Symptoms most often begin in adolescence or early adulthood, but can also begin later in mid-adulthood (physio.co.uk). It is a progressive disease so the symptoms change between earlier and later stages. Some of these signs & symptoms may include (CMT United Kingdom; physio.co.uk):
- Fatigue (most common to all those affected)
- This is a direct result of having to put in additional effort with daily activities
- Early Signs:
- Difficulty walking or an awkward walking pattern
- You may notice your child having trouble lifting their feet which may result in tripping
- You may notice your child having trouble lifting their feet which may result in tripping
- Clumsiness at a young age
- Lack of agility
- Difficulty walking or an awkward walking pattern
- Common Symptoms:
- Pes Cavus, also known as highly arched feet
- This can cause foot and ankle instability issues which may result in ankle sprains
- This can cause foot and ankle instability issues which may result in ankle sprains
- Very flat feet
- Curled or hammer toes
- This can be very uncomfortable for your child and may cause pain and difficulty finding appropriate shoes
- This can be very uncomfortable for your child and may cause pain and difficulty finding appropriate shoes
- Lower legs are very thin, while the thigh muscles are a normal shape and bulk, or size.
- This characteristic is known as the inverted champagne bottle
- This characteristic is known as the inverted champagne bottle
- Some sensory loss and numbness in both the arms and legs
- This is not usually a major problem for most individuals, but can result in unknown injuries if it is very severe
- This is not usually a major problem for most individuals, but can result in unknown injuries if it is very severe
- Cold hands and feet due to poor circulation
- Pes Cavus, also known as highly arched feet
- Later Symptoms:
- Upper limbs including both the hands and forearms may be affected as the disease progresses
- Loss of fine motor control
- Loss of dexterity & overall hand strength
- Pain
- Tremors
- Upper limbs including both the hands and forearms may be affected as the disease progresses
CMT most often affects the distal limbs first, or those limbs further away from the body such as your arms and legs. However, the lower limbs are usually affected before the upper limbs. The muscles in the lower part of your leg, ankle, and foot begin to atrophy as the disease progresses. This means the amount of muscle in these areas will decrease. Atrophy in the more proximal parts of the limbs or the parts closer to the body such as your thighs and upper arms is rare and usually only occurs in those more severely affected. As noted above, this muscle weakness along with a decrease in sensation can cause a lot of problems with both walking without any aid as well as problems with balance (Muscular Dystrophy Association 2009; Thomas et al.2014).
Management[edit | edit source]
Medical Management
There is currently no cure or drug therapy for CMT. The main treatment options are rehabilitation therapy which will involve both a physiotherapist and an occupational therapist, and surgical treatment options (Pareyson and Marchesi 2009).
Surgical Treatment
Surgical treatment is used for individuals with CMT with different skeletal deformities most often in their feet. Most individuals start out with flexible deformities in which the ankle begins to turn in, known as a cavovarus deformity. However, during the later stages of this disease, the deformity can become fixed. Treatment options are therefore, soft tissue surgeries, osteotomies or removal of bone, and joint fusions. These can either be performed on their own or as a combination of a few. Research indicating who is appropriate for surgery and when this would be optimal is not yet conclusive as more in-depth long-term studies must be completed. For the upper limbs, tendon transfers may be beneficial to improve the ability to oppose the thumb and assist with wrist extension. In addition, scoliosis, also known as a curvature of the spine, is prevalent in about 15-20% of individuals with CMT and if severe enough, may need surgical intervention (Pareyson and Marchesi 2009).
Physiotherapy Management
Physiotherapy is a key factor in your child’s management. It helps to improve the symptoms of CMT as well as decrease the risk of muscle contractures also known as the shortening of muscles. Physiotherapy for your child will most likely involve more low-impact exercises which would include posture and balance work, walking or swimming, and some strength training as well (NHS choices 2014).
Physiotherapy along with occupational therapy should be started at the onset of symptoms. Contact your GP to get information on local physiotherapists who are experienced in neurological conditions. Starting physiotherapy early on can be beneficial because muscle weakness and sensory loss will be at a minimum. The physiotherapist will work to form a treatment plan that will work best for each individual’s needs (CMT United Kingdom 2013 Physio).
The physiotherapist will also be involved in assessing for the need for any additional aids or equipment. Many people with CMT may require high-top shoes or boots in order to provide more stability to the ankles and prevent injury. Others may need braces known as ankle-foot-orthoses (AFOs) which act similar to a cast, but they are removable. An AFO is a plastic brace, custom made for each individual to provide the necessary support and prevent tripping as a result of foot-drop. If individuals have more muscle weakness proximally or higher up the leg, then knee-ankle-foot orthoses are available. The majority of individuals with CMT do not require to use of a wheelchair, however in later stages of the disease some may choose to use one when going longer distances to reduce fatigue and the amount of stress on joints. The physiotherapist will work in conjunction with the occupational therapist and help with referrals to a podiatrist to ensure that all necessary equipment has been provided (Muscular Dystrophy Association 2009). More information on different types of adaptive equipment can be found below.
Hydrotherapy
Hydrotherapy is a highly beneficial option as exercise for individuals with CMT. Essentially, it is just structured exercise lead by a physiotherapist that takes place in a pool. Hydrotherapy pools are not always easily accessible, but have many benefits especially for those individuals with CMT. Some of the benefits include reducing the amount of stress on joints due to the buoyancy of the water but still adds some light resistance to exercises in order to help maintain muscle strength (CMT United Kingdom). More Information on hydrotherapy can be found below.
Aerobic Exercise
Exercise can also be carried out in a gym or at home. Walking, cycling, swimming and mild weight-training are all appropriate exercises that are safe to carry out with CMT. Overall, any type of general exercise will be beneficial for individuals with CMT. As long as that person is comfortable and working at low-moderate intensity, research shows that aerobic exercise can help to reduce fatigue, improve mood, and increase a person’s endurance. The goal is to help keep your child as independent as possible for as long as possible (CMT United Kingdom Physio). However, it is important to avoid overworking and exhaustion. When carrying out any type of exercising, fatigue and weakness should not be caused within 30 minutes of exercises and neither should any form of excessive muscle soreness or cramping. These are things that are strongly discouraged when exercising with CMT (Grandis and Shy 2005).
Stretching
Stretching is also a key part of physiotherapy. As noted above, individuals with CMT are at risk for muscle contractures and stretching assists in maintaining muscle length. When this is done slowly and gently it can provide comfort for individuals and reduce stiffness in the joints (Grandis and Shy 2005).
Balance and Posture
Balance is an extremely important ability in order to carry out daily tasks. It involves gathering sensory input from the body and its surroundings in order to accurately orientate itself with gravity and the environment. With CMT, sensation may be altered which will affect a person’s ability to balance and ultimately completely normal activities of daily living (Nardone et el. 2010). Tai Chi, Yoga, and Pilates are all very useful exercises for improving both balance and posture.
What can you do?
[edit | edit source]
CMT is a life long progressive condition. However, making a few lifestyle changes can be extremely beneficial and improve a child’s ability to remain as independent as possible. Attending physiotherapy and keeping active are two key components that can help manage symptoms of CMT as well as slow down their progression. It is also very important that individuals with CMT maintain a healthy weight. Additional weight will only cause more stress on the joints and can further limit a person’s mobility (Poutney 2009). It is also very beneficial to do some research on CMT. Find out more about it or what support groups are available. Many individuals with CMT and their families have found it comforting to talk and listen to other people going through the same things. CMT is such a variable disease that many have found it frustrating and even scary that the progression of CMT can be so unpredictable so talking and relating with others can help take away the feeling of isolation and going through the disease alone (Lafarge et al. 2014). When looking for support networks, keep in mind that CMT is a classification of Muscular Dystrophy so the Muscular Dystrophy Association may be a good resource to check out (Muscular Dystrophy Association 2009). Other support networks and resources can be found below.
Spina Bifida[edit | edit source]
Overview[edit | edit source]
What is it?
Spina Bifida occurs when there is a problem in the formation of the spine and spinal cord in the developing embryo. It is also known as “split spine” as this developmental fault creates a gap where the spinal column fails to close and protect the spinal cord and associated nerves. This can happen at any level of the spine but most commonly occurs in the lower back or lumbar region The degree of spinal closure and the structures involved can vary in spina bifida and it can therefore be divided into 3 different types .
1. Spina Bifida Occulta
Spina Bifida Occulta or Spina Bifida Aperta is the least severe form of spina bifida, where only the bony parts of the spine are affected. A small gap remains in the spine which is covered with skin. This can be identified after birth by a small area covered by a tuft of hair or an area of darker skin along the midline of the back. This form of spina bifida can go undetected as it is not associated with significant problems. It is also thought to be present in many healthy adults.
2. Meningocoele
This is the rarest form of spina bifida where the bones of the spine are affected along with the coverings of the spinal cord: the meninges. These can protrude through the gap in the spine to form a cyst, while the spinal cord and nerves remain in place within the spinal canal.
3. Myelomeningocoele
Myelomeningocoele or Spina Bifida Cystica is the most severe form of spina bifida, affecting 1 in 1000 births in the UK. Again, there is absence of closure of the vertebrae, however, this causes leaking of the meninges as well as the spinal cord outside the gap in the spinal column. As a result, a portion of the spinal cord, along with the spinal nerves, protrudes through the gap forming a cyst or sac that lies outside the body.
The exact cause of spina bifida is unknown but there may be associated genetic, environmental and dietary factors that can predispose development of the condition in certain individuals. The most commonly researched factor is the association of low levels of maternal folic acid. Folic acid is a vitamin present in many foods and is often added to breakfast cereals. It can also be found as a supplement in the pharmacy. It is thought to be involved in the development and formation of fetal cells and tissues, therefore, it is advised that folic acid should be taken daily in the upcoming months before conceiving and also during pregnancy (Ray et al., 2002).
Signs and Symptoms
Children with Spina Bifida can have a variety of symptoms which can vary from mild to severe. The main symptoms include:
1. Cognitive symptoms
- As spina bifida occurs due to problems with the developing spine and spinal cord, this can have an associated effect on development of the brain. Specifically areas of the brain involved in memory, learning, as well as concentration, understanding and the processing of language. Children may have difficulty with complex motor tasks such as tying laces where good visual and physical coordination is required (Barf et al., 2003).
- 6 out of 10 children born with spina bifida will have normal intelligence levels, although around half of these will have some form of learning disability (Hinderer et al., 2006)
2. Mobility Symptoms
- The spinal cord allows information to travel up and down to brain in order to control movements made by muscles and joints. As the spinal cord and nerves can be compromised in certain types of Spina Bifida, there are often problems with muscle control and joint movement. In some cases, there may be paralysis of certain muscles which can result in the development of misshapen bones, particularly the feet, and abnormal curving of the spine known as Scoliosis (Park Brown., 2001). Those with severe mobility restrictions may also develop thin bones or osteoporosis due to the lack of use of the limbs (Ausili et al., 2008)
- The spinal cord and nerves also provide the brain with sensory information through touch. As the spinal nerves can be damaged in some forms of Spina Bifida, there may be associated loss of sensation and feeling in the pelvic region and legs (Hunt et al., 1999). This can cause problems with pressure sores and skin breakdown in infants who are unable to feel the need to change position (Tappit-Emas, 2008).
3. Incontinence (Urinary and Bowel)
- The nerves travelling through the spinal cord also supply the bladder and bowel, ensuring the muscles within these organs can contract to contain urine and stools within the body. As a result, most children born with Spina Bifida will experience some degree of urinary and bowel incontinence (Sandler., 2010)
Management
[edit | edit source]
Medical Management
Medical management of the newly born child with Spina Bifida varies according to the severity of their condition. Those with Spina Bifida Occulta do not ususally require any specific treatment. Some people with Spina Bifida Occulta do not exhibit any symptoms and may only discover they have the condition when they are older after having an XRAY. Children born with myelocoele or myelomeningocoele will require surgery normally within 2-3 days of birth in order to close the gap in the spine and return the spinal cord and nerves to their original place within the spinal column (Tappit-Emas, 2008). This aims to prevent infection and further damage to the exposed spinal cord and spinal nerves. Following surgery, the child will be monitored closely for signs of common post-operative problems associated with this type of surgery, namely hydrocephalus and leaking of cerebrospinal fluid (Sandler., 2010).
As the infant gets older, management of incontinence will be an important role of the medical team. Effective management strategies include the use of Clean Intermittent Catheterisation (CIC) and certain drugs which can increase the storage volume of the bladder (Lapides et al., 1972). Children can also develop constipation due to lack of bowel movements and will require development of a bowel programme which may involve assisted evacuation of stools. However, this will be based on an individualised assessment of the child and may involve educating the family in order to ensure the programme is effectively integrated into the child’s daily routine (Leibold et al., 2008). Effective strategies in managing incontinence in children with spina bifida are extremely important in allowing them to socially integrate themselves as they get older and attend school (Sandler., 2010).
Physiotherapy management
The role of the physiotherapist in early management of children with spina bifida is extremely important as it helps the child to develop efficient and purposeful movement that can be incorporated into every day tasks (Swank & Diaz., 1992). By optimising and maintaining mobility, this can eventually help children to become more independent as they get older. The physiotherapist will perform an initial assessment of the infants muscle strength and range of movement available at certain joints. This will allow the physiotherapist to determine which muscles are working properly and which ones are weak. This will give them a baseline measurement to use as a comparison as the child grows. This will also allow the physiotherapist to consider what problems the infant may have as they get older and what type of assistive devices or splints they may require when they begin to mobilise (Sandler., 2010). The physiotherapist will specifically be involved in:
1. Joint Range of Motion
In the early stages following surgery, the physiotherapist will begin passive range of motion exercises on the infant’s legs (Tappit-Emas., 2008). This will normally be performed 2-3 times a day. They will also demonstrate this technique to parents or carers so that they may continue to do these exercises as a home exercise programme when the infant is discharged. They may progress these exercises to mimic more functional movements which are related to normal everyday movement patterns. For example, whilst bending the left knee and hip, the right side will be kept straight as would happen in a normal walking pattern. These gentle exercises will help to maintain and may help increase the available range of motion available in joints where the movement restriction is mild. In those who have more pronounced restriction, the physiotherapist may advise that the number of exercise repetitions is increased and the movement is held for longer.
The ultimate aim of range of motion exercises is to enable the child to learn and perform them independently as they grow up. It is important for the child to continue with these exercises because when they are moving independently, the functioning muscles may not be working through full range of motion. Passive range of motion exercises will therefore help to maintain flexibility and avoid the development of muscle tightenings known as contractures (Tappit-Emas., 2008).
2. Muscle strength
Altered muscle tone is a common symptom of spina bifida therefore physiotherapists use resistance training in order to strengthen these muscles that have been weakened. This is normally introduced when the infant is old enough to self mobilise. The physiotherapist can develop a programme of strength and endurance training which has been seen to improve functional abilities in children with spina bifida (O’Connell & Barnhart, 1995). These training programmes may involve a variety of exercises for the upper and lower limbs, as well as muscles of the trunk and can help improve upper limb strength and cardiovascular fitness (Andrade et al., 1991).
3. Positioning and Handling
Following the first few days after surgery, the infant will normally be placed in side or stomach lying. As the infant begins to stabilise and recover from surgery, the physiotherapist will offer advice as to how to hold the new born child safely. This is incredibly important as the infant will have undergone major surgery which requires careful handling and positioning at all times. It may be advised that parents or carers hold the child underneath the stomach and across their forearm due to the surgical wound that will be present on the infant’s back. This handling technique may be used when sitting or walking around. When advised, parents or carers may take the infant for a walk around the hospital resting over the shoulder. This can encourage the child to begin to lift his or her head and begin to develop head and neck control (Tappit-Emas., 2008).
4. Mobility and Ambulation
Mobility problems in children with spina bifida can vary according to the level of the spine that has been affected during development (Thompson., 2009). A child with a lesion in the lower back (Lumbar or Sacral levels), is more likely to be able to independently mobilise than one with a lesion in the upper thoracic spine. This can determine whether the child will require a wheelchair, orthotics or assistive devices (Seitzberg et al., 2009).
Parents and carers are often discouraged from using assistive devices such as infant walkers, jumpers and bouncer chairs as these can delay motor development. Infants require active movement and sensory information from the surrounding environment in order to learn how to move efficiently against gravity and maintain erect sitting and standing postures. This is no different for children with Spina Bifida. Infants with spina bifida benefit from movements that challenge control of the head, neck and torso, rather than the use of passive sitting devices or chairs. Active movement allows them participate in the learning process. For example, rather than using a walker, parents are advised to physically hold their child in the standing position with as little support as possible to promote the necessary control of the legs and torso. This also allows the child to receive feedback from the floor and the surrounding environment (Tappit-Emas., 2008).
As the child begins to mobilise and ambulate more independently, he or she may be fitted for braces or splints to address any deformities caused by muscle imbalance or joint limitations. Orthoses such as braces and splints, are supportive devices aimed at optimising existing muscle function and giving support where the child requires it. The earlier these are fitted and provided, the earlier the child will be prepared for the upright position require of standing and walking (Cuddeford et al., 1997). It therefore also enhances normal developmental progression and will eventually help the child take part in normal activities of their age group (Tappit-Emas., 2008). Children with Spina Bifida lesions in the upper thoracic regions of the spine may require bracing or splinting of the whole leg up to the level of the hip and chest. This is known as a Hip-Knee-Ankle-Foot Orthoses (HKAFO). Others may require orthotics aimed at stabilising the knee, ankle and foot. These are known as Knee-Ankle-Foot orthoses (KAFO) and Ankle-Foot Orthoses (AFO) (Park Brown., 2001). Reciprocal Gait Orthoses (RGO) may be also provided in order to promote a normal rhythmic walking pattern in the child (Yngve et al., 1986; Cuddeford et al., 1997). Children may require the additional use of crutches along with orthoses in order to take some stress off the legs (Mazur & Kyle., 2004) and standing frames are also used to help children with more severe limitations bear weight through their legs and maintain full range of motion at all lower limb joints (Tappit-Emas., 2008). Furthermore, some children may require casting as a way of treating and preventing contractures. Casting aims to develop a gradual increase in the range of motion available at a certain joint and is a very effective method of improving range of motion at tight joints without the use of surgery (Al-Oraibi., 2014). Other children may benefit from the use of a wheelchair, as it can give them more freedom of movement if their walking is limited and strenuous. This can be alternated with the use of orthosis for shorter distances. A wheelchair can also help children keep pace with other able bodied people, and enable them to participate in recreational activities at school (Tappit-Emas., 2008).
5. Parent/carer education
Physiotherapy management will eventually be handed over to the parents or carers of the infant. Initially they will be encouraged to observe the physiotherapist carrying out range of motion exercises and handling and positioning strategies before being asked to duplicate these treatments independently. Following these teaching sessions, certain roles will then be handed over to the parents and carers. Following discharge home and as the child begins to mobilise more independently the parents and carers should actively become involved in assessing their child’s progression through observations at home when playing, sitting, crawling etc. This can help with early identification of any differences in the child’s movements or sitting postures between the home and the hospital. It may also allow other possible problems to be identified early on so that a management strategy may be developed. This is essential particularly later on when the child becomes more medically stable, as they will not receive as much medical input and interaction as when the child was a new born infant in hospital (Tappit-Emas., 2008).
The physiotherapist, along with other members of the healthcare team, will be able to offer advice and help parents and carers build confidence in their ability to manage their child’s daily routine (Sawin et al., 2003).
What can you do?
[edit | edit source]
In the infant with spina bifida it is important to observe their movement patterns in the home and to report any change in posture, balance or movement. As your child gets older, encouraging them to continue to perform their range of motion exercises will help to maintain their flexibility and avoid the development of contractures (Tappit-Emas., 2008). Encouraging active and regular exercise participation in children with spina bifida is also extremely important, as they are at a greater risk of becoming overweight due to the fact they are unable to move as much as other children (Park Brown., 2001). As a result, children with spina bifida are more likely to develop high blood pressure as they get older and may be at a higher risk of developing other forms of cardiovascular disease such as stroke, coronary artery disease and kidney disease (Buffart et al., 2008; Stepanzuk et al., 2014). Children with spina bifida should be encouraged to take part in regular sporting or recreational activites that target cardiovascular fitness, muscle strengthening and coordination (Tappit-Emas., 2008; Oliveira et al., 2014). Not only will this have physical benefits, but it can also provide the child with social interaction and important life experiences. Activities designed for wheelchair users are becoming increasingly popular and include basketball and tennis (Park Brown., 2001).
Swimming and aquatic physiotherapy are also extremely effective ways of encouraging activity in children with spina bifida. This can begin at young age with the use of flotation devices, and can help the child move with greater ease than when out with the water. This can make it very enjoyable for both the child and their parents or carers. Swimming also targets cardiovascular fitness and muscle strengthening of the legs, arms and torso through the resistance created as the child moves through the water (Tappit-Emas., 2008). The physiotherapist can assist and give advice as to the level of activity a child may require and when it is appropriate to begin activities such as swimming. They may also work along side school staff involved in physical education to help identify activities that a child may particularly enjoy, or to discuss ways of modifying and adapting existing recreational activities that the school provides (Tappit-Emas., 2008).
Erbs Palsy[edit | edit source]
Overview
[edit | edit source]
Also known as Obstetric Brachial Plexus Injury/Erbs Palsy and includes Erb’s Palsy, Klumpke’s Palsy and Erb-Klumpke Palsy. ???? occurs through damage to the brachial plexus , a grouping of nerves , in the shoulder during birth. Nerves coming from the brachial plexus supply the muscles, skin and other tissue of the arm and shoulder. Injuries to the brachial plexus disrupt communication from the arm to the spine and therefore the brain. This can result in loss/altered sensation, loss of muscle function. One of the most common presentations of brachial plexus injury is of an arm brought in to and rotated towards the body.
Birth Brachial Plexus Palsy occurs in between 0.38-3 per 1000 live births in developed countries (Zafeirou, DI and Psychogiou K 2008).
Birth Brachial Plexus Injury is sometimes associated with Horner’s Syndrome and Shoulder dystocia .
The earlier the signs of recovery the better the prognosis with returning biceps function a key indicator. 95% of infants born with a birth brachial plexus palsy recover complete function with physiotherapy (U.S. Department of Health, Education and Welfare). However it is important to understand that lasting disability is a possibility.
Predictors of poor outcome: lack of elbow function at 3 months; Complete C5 to T1 injury; Presence of Horner’s Syndrome.
http://www.erbpalsy.org/infographic.html
Management
[edit | edit source]
Physiotherapy Management
Key aspects of physiotherapy for Birth Brachial Plexus Injury:
- Movement at the joints – Ensuring that the joints of the affected limb, especially the shoulder, keep their full range of movement and avoid excessive shortening of the muscles . This will include both passive, assisted and active exercises (Lorna, RE and Zell JP)
- Increasing the strength of muscles in the affected limb
- Increasing the child’s awareness of the arm through tactile touch and contact
- Teaching parents, carers and the child how to handle the affected limb and how to position it for both comfort, prevention of complications and practicality
The use of Constraint Induced Movement Therapy (CIMT) and bimanual/bilateral therapy are sometimes considered by Physiotherapists.
Positioning
- On back or side lying with affected limb up – avoid compression of injured limb
- Do not pick child up by the arm or from under the arm pit – Cause compression/stretch of brachial plexus and further injury
- In sitting?
- During the day?
Medical Management
Surgical intervention is a possible treatment option and will be considered by the medical team after appropriate assessment. Surgery is only considered when conservative treatment (such as physiotherapy) is deemed unlikely to affect outcome.
Surgery for ???? could involve nerve transplants or tendon transfer . If the medical team believe that surgery would be the best option for your child they will discuss this, in-depth, with you. The team will look to provide you with all the information possible on why they believe surgery is the right option, what it will involve and what the potential risks are. You and your child should be central to the decision making process and you should seek to discuss all your concerns/queries with the team providing healthcare to you and your child.
What can you do?[edit | edit source]
Your Physiotherapist will most likely give you a Home Exercise Programme to carry out with your child. This should be the focus of your child’s treatment and you should carry out the ‘exercises’ regularly with your child. Your child should be encouraged to be as active as possible and it is important not to let the diagnosis of ???? impact on your child’s quality of life. Children need to be active and research shows that they should be enjoying 60 minutes of activity a day between the ages of ????. An active lifestyle has many benefits for individuals no matter what their age! See our Keeping Active section for more information.
A number of individuals diagnosed with ???? went on to have successful careers in their chosen field, Martin Sheen was diagnosed with ???? as was Adrain Clayborn, an American Football player who was drafted 20th overall in the 2011 Draft by the Tampa Bay Buccaneers.
There are also other inspiring individuals out there, including Emily Langridge, a young woman with ???? who create a documentary following families, adults and children with the condition. You can watch the film on the website of the Brachial Plexus Palsy Project.
Dina Shafer, who also has a lasting disability affecting her ?? arm after being diagnosed with ????, has a Youtube channel showing how she goes about carrying out her activities of daily living which include driving her car, curling her hair and going to the gym where she performs deadlifts and trains in martial arts.
Other Useful links include the Erbs Palsy Group, the United Brachial Palsy Network, the Brachial Plexus Palsy page on Facebook,
Microcephaly and Hydrocephaly
[edit | edit source]
Staying Active[edit | edit source]
Keeping fit[edit | edit source]
Playing Sport[edit | edit source]
This is a test [3]
Paralympics[edit | edit source]
Respite and Special Schools[edit | edit source]
Edinburgh and the Lothians[edit | edit source]
Support Networks[edit | edit source]
Financial Support[edit | edit source]
Parents Stories[edit | edit source]
Equipment and Aids
[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.