Clinical Reasoning and Pathologies of the Thoracic Spine
Top Contributors - Jess Bell, Lucinda hampton, Kim Jackson, Carin Hunter, Rucha Gadgil and Olajumoke Ogunleye
Introduction[edit | edit source]
The thoracic spine is a complex area that has been largely overlooked in research.[1] While only 13 percent of individuals specifically report thoracic pain each year,[2] it is now recognised that the thorax can be a silent contributor to a number of distal and proximal conditions.[1] Moreover, a number of non-mechanical pathologies can masquerade as musculoskeletal thoracic pain. All of these conditions must be considered when assessing patients who have thorax pain. This page discusses key muscles that are often implicated in thoracic dysfunction and explores specific pathologies which affect the thorax.
Muscles of the Thorax[edit | edit source]
There are 112 muscle attachments in the thorax. This page looks at major muscle groups that can have a significant impact on the thorax. Additional information on thoracic spine musculature is available here.
Intercostals[edit | edit source]
There are 11 pairs of intercostal muscles, each consisting of three layers arranged from superficial to deep:[3]
- External
- Internal
- Innermost
The intercostal nerves mostly come from the anterior rami of the T1 to T 11 spinal nerves.[3] Along with the intercostal artery and vein, these nerves run between the intermediate and deep layers of the intercostal muscles. The T7 to T11 intercostal nerves leave the thoracic wall and enter the abdominal wall to innervate the abdominal peritoneum.[4] They supply:[4]
- Ribs and costal cartilages
- Intercostal muscles (all layers)
- Parietal pleura, which lines the inner surface of the thoracic cavity, including the diaphragm, pericardium and thoracic aorta
Because of this shared innervation, diseases of the thoracic wall or cavity may masquerade as dermatomal pain arising from the thoracic spine.[4] Thus, it is essential to constantly assess a patient for red flags, including a poor response to treatment, as this may indicate a more serious pathology.[4][5]
Iliocostalis[edit | edit source]
Iliocostalis is the most lateral of the erector spinae muscles. It is divided into three parts:[6]
- Iliocostalis cervicis
- Iliocostalis thoracis
- Iliocostalis lumborum
Iliocostalis lumborum originates at the iliac crest and inserts into the L1 to L4 lumbar transverse processes, the angle of ribs 4 to 12, and the thoracolumbar fascia. Iliocostalis cervicis and thoracis have attachments as high as the upper 6 ribs and the transverse processes of C4.[6] Iliocostalis, therefore, links lumbo-pelvic dysfunction with thoracic dysfunction and hypertonicity in this muscle can potentially have an impact on the thoracic rings.[4]
Pectoralis Major[edit | edit source]
The pectoralis major makes up the bulk of the chest muscles. It is a thick, fan-shaped muscle that originates at the:[7]
- Anterior sternum (down to the xiphoid process)
- Clavicle
- 6th rib (sternal end)
- Upper 6 costal cartilages
- Aponeurosis of the external oblique
It inserts into the lateral lip of the bicipital groove on the humerus.[7]
Overactivity of pectoralis major is associated with thoracic kyphosis and anterior translation of the humerus.[4]
- Bodybuilders, for example, often have overactive pectoralis major muscles and thoracic dysfunction
- Horizontal clavicles can indicate an individual has overactive pectoralis major muscles
- Pectoralis stretching can help to reduce kyphosis (and forward head position / rounded shoulder position)[8][9]
NB: pectoralis major also has fascial links with latissimus dorsi (see below).[4][10]
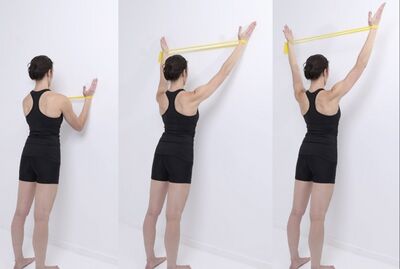
The exercise shown in Figure 1 can be beneficial to improve thoracic and scapula motor control. It can also reduce thoracic kyphosis by increasing the activity of middle and lower trapezius and reducing overactivity in upper fibres of trapezius.[4]
NB: activating lower trapezius plays a key role in addressing an increased thoracic kyphosis. The cue “down and out” should be given during exercises, rather than “down and in”.[4]
Rhomboid Major and Minor[edit | edit source]
The rhomboids consist of two muscles:[11]
- Rhomboid major
- A quadrangular muscle
- Inferior to rhomboid minor
- Originates at the T1 to T4 spinous processes
- Inserts into the medial margin of the scapula below the root of the inferior angle[4]
- Rhomboid minor
- A cylindrical muscle
- Originates at the ligamentum nuchae and C7 and T1 vertebra
- Inserts into the medial margin at the root of the spine of the scapula
Overactivity in these muscles leads to:[4]
- Inverted thoracic spine with facet compression forces
- Scapula held in downward rotation with resultant cervical spine loading
- Dural irritation
Serratus Anterior[edit | edit source]
Serratus anterior is a fan-shaped muscle. It lies deep to the scapula and pectoral muscles:[12]
- It originates on the superolateral surfaces of the upper 8 or 9 ribs
- It runs backwards and inserts along the superior angle, medial border, and inferior angle of the scapula
This muscle is a powerful protractor (abductor). It is also involved in upward rotation (which allows for overhead activity), posterior tilt and external rotation of the scapula. It holds the scapula flat against the rib cage and can mobilise the thoracic spine into kyphosis.[4][12]
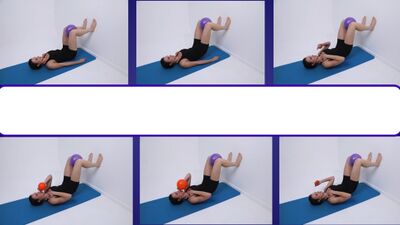
The exercises shown in Figure 2 are useful for:[4]
- Inverted thoracic spine
- Possible dural pain
- Targeting the various digitations of serratus anterior
External Oblique vs Serratus Anterior[edit | edit source]
External oblique, along with the internal oblique and transversus abdominis make up the three anterolateral abdominal wall muscles. The external oblique is the most superficial, the largest and thickest of these three muscles:[4][13]
- It attaches to the lower 6 or 7 ribs (and, therefore, can affect the activity of the diaphragm)[4]
- It runs obliquely from superior / lateral to inferior / medial
- It inserts on the iliac crest
The external oblique and serratus anterior interdigitate from the 5th to the 9th ribs.[4] The opposing actions of these muscles (e.g. during actions such as rowing or coughing) create a stress reaction, and are a major contributor to stress fractures.[14]
The Diaphragm[edit | edit source]
The diaphragm is a dome-shaped muscle of respiration that is innervated by the phrenic nerve (C3-5). The superior portion of the diaphragm originates at the:[15]
- Xiphoid process anteriorly
- The lower 6 costal cartilages of the thorax laterally via digitations that cross those of transversus abdominis[16]
- The first two lumbar vertebrae posteriorly
It converges into a central tendon which forms the dome’s crest. The peripheral segment attaches to the chest wall and abdominal cavity.[15]
The diaphragm is connected via fascia to the:[4]
- Aortic system
- Inferior vena cava
- Liver
- Psoas muscles
- Quadratus lumborum
- Transversus abdominis
- Pelvic floor
- Cardiac system (pleura and pericardium)
- Deep and median neck fascia
- Occiput
- Dura
- Phrenic-oesophageal ligaments
- Kidneys
The diaphragm and intercostals are the only muscles that are active during quiet inspiration.[17] During quiet exhalation, the diaphragm, rib cage and chest wall relax and return to their original position, which expels the air from the lungs.[15]
The diaphragm is, therefore, essential for optimal respiratory physiology. It also affects many other systems as well, including the nervous system, muscle and postural systems, as well as the lymphatic system.[4][17]
The Effect of Diaphragmatic Bracing on the Thoracic Spine[edit | edit source]
Diaphragmatic bracing in low load situations can occur in:[4]
- Chronic low back pain[18]
- PTSD
- Panic attacks
- COVID-19
Patients who engage this bracing strategy may present with back, thoracic, neck and rib pain. Bracing fixes the thoracic wall and reduces thoracic mobility. It can lead to:[4]
- Hypocapnia (i.e. decrease in carbon dioxide levels)
- Increased respiratory rate
- Apical breathing
- Irregular respiratory rate
Normally, ribs 1 to 7 posteriorly rotate during full inspiration and anteriorly rotate during full expiration.[19][20] It is important to teach patients correct respiration as optimal breathing mechanics promote synchronous movement of the ribs.
The 90/90 bridge with ball and balloon exercise (see Figure 3) was created to enhance function and breathing, improve posture and stability and to reduce pain.[21]
Pathologies[edit | edit source]
Spinal Masqueraders[edit | edit source]
In some instances, thoracic pain may have non-mechanical origins. Visceral or systemic conditions that present as thoracic pain are known as spinal masqueraders. Examples of thoracic spinal masqueraders include:[4]
- Pneumothorax
- Pleuritic pain
- Coronary heart disease
- Oesophageal pain
- Tumours (e.g. lung)
- Liver and spleen conditions
- Herpes zoster
- Seronegative arthritis
- Ankylosing spondylitis
- Pneumonia
- Malignant lymphoma
- Stomach ulcers
Thoracic Outlet Syndrome[edit | edit source]
Thoracic outlet syndrome (TOS) is a group of disorders that cause compression of the nerves, arteries or veins as they exit the thoracic outlet. TOS typically occurs in three places:[4]
- Scalene triangle
- Costoclavicular space
- Retropectoral space
Postural / thoracic kyphosis, tight bra straps, overactive subclavius, and the presence of a cervical rib can narrow the costoclavicular space and create neurovascular symptoms.[4] Structures usually affected in TOS are the:[22]
- Subclavian artery and vein
- Axillary artery and vein
- Brachial plexus
There are three types of TOS:[22][23]
- Neurogenic (i.e. brachial plexus)
- Most common type (approximately 95 percent of cases[24])
- Symptoms include:
- Pain
- Weakness
- Heaviness in the arm
- Paraesthesia
- Neurogenic symptoms tend to be worse with overhead activities or when the patient's arm is dangling at his / her side
- Venous (i.e. subclavian vein) - also known as Paget–von Schroetter syndrome[24]
- Symptoms include:
- Swelling
- Pain
- Bluish discoloration
- Symptoms include:
- Arterial (i.e. subclavian artery)
- Least common type
- Symptoms include:
- Pain
- Coldness
- Paleness in the arm
TOS is often missed by clinicians - the average time to diagnosis is 60 months. TOS may be mistaken for carpal tunnel, cervical nerve root compression, psychosocial issues, complex regional pain syndrome, fibromyalgia, MS etc.[4]
TOS can be diagnosed using the following tests and investigations:[25]
- Adson’s test
- Elevated arm stress test (Roos test)
- It has been found that using the Adson and Roos tests as a cluster results in higher specificity than using these tests on their own[24]
- Upper limb tension test
- Nerve conduction study
- MRI in elevation
- Doppler / duplex ultrasound
- Scalene blocks can be used as a diagnostic tool[23]
- Warm and cold thermal detection also has good reliability[26]
Stress Fracture of the Ribs[edit | edit source]
Stress fractures of the ribs are typically associated with sports that have:[4]
- High strain magnitudes (e.g. weightlifting)
- High load repetitions (e.g. golf, rowing, throwing, overtraining)
They tend to occur when the opposing actions of serratus anterior and external oblique generate pulling forces and, consequently, a stress reaction (see above).[14]
Rowing:
- The incidence of rib stress fractures in rowing is between 6 and 12 percent:[27]
- Occurs most often in ribs 5 to 9
- Typically antero-lateral, but can be postero-lateral[14]
Golf:[28]
- Most commonly occurs on the lead-side (i.e. non-dominant) and affects the postero-lateral ribs
- Ribs 4 to 6 are most often affected
Rib stress fractures are diagnosed based on history and bone scans, CT or MRI.[4] Patients tend to require 3/4 to 9 weeks off sports.[4][29][30]Patients tend to present with:[29]
- History of insidious onset (overload) with sudden pain
- Pain with deep breathing, coughing, sneezing, turning in bed
- Patients complain they are unable to sleep on the affected side
- Severe, specific, palpable pain on examination
- Positive rib spring
- Altered breathing mechanics
- Pain with push-up and with resisted serratus anterior testing
- Pain with sit-up, including with oblique bias
Manubriosternal Joint Pain[edit | edit source]
Manubriosternal joint pain often occurs as a result of an acceleration / deceleration injury[31] (e.g. throwing, serving). Sclerosis of this joint is seen in various types of arthritis, including:[4]
- Axial spondyloarthritis / ankylosing spondylitis
- Reactive arthritis / Reiters
- Psoriatic arthritis
- Rheumatoid arthritis
Costochondritis[edit | edit source]
Costochondritis is inflammation of the costochondral or chondrosternal joints. It is more common in adults aged over 40 years. In 90 percent of patients, more than one rib is affected. The ribs most frequently affected are ribs 2 to 5.[32]
- Mild to severe localised pain, but may refer to the shoulder, neck and arms[4]
- Can be mistaken for Tietze syndrome, but this condition is characterised by swelling of a single costal cartilage, usually in ribs 2 or 3 and is more common in younger patients[32]
- It is important to rule out seronegative arthritis, pneumonia, cardiovascular and malignant disorders[4]
- It is treated with NSAIDs and it can take weeks or months to resolve[32]
Cervical Facet Pain[edit | edit source]
It is well established that cervical discs, as well as cervical facet joints refer pain to the upper thorax.[4]
Thoracic Disc Pathology[edit | edit source]
Thoracic disc pathology is rare and individuals are often asymptomatic. In 75 percent of cases it occurs at T8 or below (and is more likely to occur around T11 to T12).[33] Only 1 percent of prolapses with severe myelopathy occur in the thoracic spine.[4]
- The thoracic disc is thinner than in other regions
- The ratio of the thoracic disc to the vertebral body is 1:5 (vs 2:5 in the cervical spine and 1:3 in the lumbar spine)[4]
- Central thoracic pain (myelopathic):[4]
- Leg paralysis and spinal cord compression
- Bladder and bowel impairment
- Dermatomal unilateral pain (radicular), which compresses the nerve root[4]
Summary[edit | edit source]
- It is beneficial to restore a neutral thoracic spine
- Serratus anterior is key to restoring an optimal thoracic kyphosis (i.e. neutral spine) from a dysfunctional inverted position
- Teaching correct respiration is important as good breathing mechanics prompt synchronous movement of the ribs
- As there are many thoracic spinal masqueraders, red flags should be constantly assessed:
- The biggest red flag is a poor response to treatment
References[edit | edit source]
- ↑ 1.0 1.1 Bell-Jenje T. The Thorax Simplified - Anatomy, Biomechanics and Regional Interdependence Course. Physioplus, 2021.
- ↑ Leboeuf-Yde C, Nielsen J, Kyvik KO, Fejer R, Hartvigsen J. Pain in the lumbar, thoracic or cervical regions: do age and gender matter? A population-based study of 34,902 Danish twins 20–71 years of age. BMC Musculoskelet Disord. 2009;10(39).
- ↑ 3.0 3.1 Tang A, Bordoni B. Anatomy, Thorax, Muscles. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538321/
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 4.24 4.25 4.26 4.27 4.28 4.29 4.30 4.31 4.32 4.33 4.34 Bell-Jenje T. Assessment and Treatment of the Thoracic Spine Course. Physioplus, 2021.
- ↑ Finucane LM, Downie A, Mercer C, Greenhalgh SM, Boissonnault WG, Pool-Goudzwaard AL et al. International framework for red flags for potential serious spinal pathologies. J Orthop Sports Phys Ther. 2020;50(7):350-72.
- ↑ 6.0 6.1 Henson B, Kadiyala B, Edens MA. Anatomy, Back, Muscles. [Updated 2021 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537074/
- ↑ 7.0 7.1 Solari F, Burns B. Anatomy, Thorax, Pectoralis Major Major. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525991/
- ↑ Roddey TS, Olson SL, Grant SE. The effect of pectoralis muscle stretching on the resting position of the scapula in persons with varying degrees of forward head/rounded shoulder posture, Journal of Manual & Manipulative Therapy. 2002;10(3):124-8.
- ↑ Kim MK, Lee JC, Yoo KT. The effects of shoulder stabilization exercises and pectoralis minor stretching on balance and maximal shoulder muscle strength of healthy young adults with round shoulder posture. J Phys Ther Sci. 2018;30(3):373-80.
- ↑ Pandya R. Upper Extremity Myofascial Chains Course. Physioplus, 2021.
- ↑ Farrell C, Kiel J. Anatomy, Back, Rhomboid Muscles. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534856/
- ↑ 12.0 12.1 Lung K, St Lucia K, Lui F. Anatomy, Thorax, Serratus Anterior Muscles. [Updated 2020 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531457/
- ↑ Seeras K, Qasawa RN, Ju R, et al. Anatomy, Abdomen and Pelvis, Anterolateral Abdominal Wall. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525975/
- ↑ 14.0 14.1 14.2 Karlson KA. Rib stress fractures in elite rowers. A case series and proposed mechanism. Am J Sports Med. 1998;26(4):516-9.
- ↑ 15.0 15.1 15.2 Bains KNS, Kashyap S, Lappin SL. Anatomy, Thorax, Diaphragm. [Updated 2020 Apr 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519558/
- ↑ Bordoni B, Zanier E. Anatomic connections of the diaphragm: influence of respiration on the body system. J Multidiscip Healthc. 2013 Jul 25;6:281-91. doi: 10.2147/JMDH.S45443. PMID: 23940419; PMCID: PMC3731110. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3731110/
- ↑ 17.0 17.1 Clifton-Smith T. How We Breathe Course. Physioplus, 2020.
- ↑ Kolar P, Sulc J, Kyncl M, Sanda J, Cakrt O, Andel R, Kumagai K, Kobesova A. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012 Apr;42(4):352-62. doi: 10.2519/jospt.2012.3830. Epub 2011 Dec 21. PMID: 22236541. https://www.jospt.org/doi/full/10.2519/jospt.2012.3830
- ↑ Beyer B, Sholukha V, Dugailly PM, Rooze M, Moiseev F, Feipel V et al. In vivo thorax 3D modelling from costovertebral joint complex kinematics. Clin Biomech (Bristol, Avon). 2014;29(4):434-8.
- ↑ Lee DG. Biomechanics of the thorax - research evidence and clinical expertise. J Man Manip Ther. 2015;23(3):128-38.
- ↑ Boyle KL, Olinick J, Lewis C. The value of blowing up a balloon. N Am J Sports Phys Ther. 2010;5(3):179-88.
- ↑ 22.0 22.1 Li N, Dierks G, Vervaeke HE, Jumonville A, Kaye AD, Myrcik D et al. Thoracic outlet syndrome: a narrative review. J Clin Med. 2021;10(5):962.
- ↑ 23.0 23.1 Illig KA, Donahue D, Duncan A, Freischlag J, Gelabert H, Johansen K et al. Reporting standards of the Society for Vascular Surgery for thoracic outlet syndrome. J Vasc Surg. 2016;64(3):e23-35.
- ↑ 24.0 24.1 24.2 Jones MR, Prabhakar A, Viswanath O, Urits I, Green JB, Kendrick JB et al. Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis, and treatment. Pain Ther. 2019;8(1):5-18.
- ↑ Povlsen S, Povlsen B. Diagnosing thoracic outlet syndrome: current approaches and future directions. Diagnostics (Basel). 2018;8(1):21.
- ↑ Ridehalgh C, Sandy-Hindmarch OP, Schmid AB. Validity of clinical small-fiber sensory testing to detect small-nerve fiber degeneration. J Orthop Sports Phys Ther. 2018;48(10):767-74.
- ↑ Warden SJ, Gutschlag FR, Wajswelner H, Crossley KM. Aetiology of rib stress fractures in rowers. Sports Med. 2002;32(13):819-36.
- ↑ Lee AD. Golf-related stress fractures: a structured review of the literature. J Can Chiropr Assoc. 2009;53(4):290-99.
- ↑ 29.0 29.1 Evans G, Redgrave A. Great Britain Rowing Team guideline for diagnosis and management of rib stress injury: part 2 - the guideline itself. Br J Sports Med. 2016;50(5):270-2.
- ↑ McDonnell LK, Hume PA, Nolte V. Rib stress fractures among rowers: definition, epidemiology, mechanisms, risk factors and effectiveness of injury prevention strategies. Sports Med. 2011;41(11):883-901.
- ↑ Bar-Haim R, Shtarker H, Biswas S, Waksman I, Altman E. Case report: surgical management of painful manubriosternal pseudoarthrosis. Front Surg. 2021;8:640089.
- ↑ 32.0 32.1 32.2 Proulx AM, Zryd TW. Costochondritis: diagnosis and treatment. Am Fam Physician. 2009;80(6):617-20.
- ↑ Fogwe DT, Petrone B, Mesfin FB. Thoracic Discogenic Syndrome. [Updated 2020 Nov 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470388/