Cervicitis: Difference between revisions
No edit summary |
No edit summary |
||
| (3 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Elaine Lonnemann|Elaine Lonnemann]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== Introduction == | |||
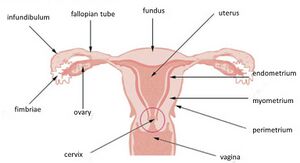
[[File:Cervix.jpeg|right|frameless]] | |||
Cervicitis is inflammation of the cervix, the donut-shaped opening that connects the vagina to the uterus. It can be acute or chronic; with chronic occurring due to inadequate treatment or recurrent inflammation<ref name="Singh">Singh N, Arora A. An Extreme Case of Chronic Cervicitis Mimicking Cervical Cancer and Causing Third-Degree Prolapse. Journal Of Gynecologic Surgery [serial online]. December 2014;30(6):380-382. Available from: Academic Search Complete, Ipswich, MA. Accessed February 23, 2017.</ref> Non-specific cervicitis is the most common; meaning that it is unrelated to an STI like chlamydia or gonorrhea <ref name="Pollett et al">Pollett S, Calderon M, Heitzinger K, Solari V, Montano S, Zunt J. Prevalence and predictors of cervicitis in female sex workers in Peru: an observational study. BMC Infectious Diseases [serial online]. April 30, 2013;13:195. Available from: MEDLINE, Ipswich, MA. Accessed February 23, 2017.</ref> A single instance or acute cervicitis is usually due to an infection like chlamydia or gonorrhea, while chronic is typically due to a non-infectious source<ref name="Efosa et al">Efosa O, Uwadiegwu A. Cytopathological Examination and Epidemiological Study of Cervicitis in Commercial Sex Workers (Csws) in Coal City (Enugu), Nigeria. Ethiopian Journal Of Health Sciences [serial online]. July 2015;25(3):225-230. Available from: Academic Search Complete, Ipswich, MA. Accessed April 4, 2017.</ref> If left untreated cervicitis can lead to pelvic inflammatory disease<ref name="Pollett et al" /> | |||
== Etiology == | |||
The etiology is broadly classified into infectious and non-infectious. | |||
== | |||
= | # Infectious agents include Neisseria gonorrhea, Chlamydia trachomatis, and less commonly, herpes simplex, Trichomonas vaginalis, and Mycoplasma genitalium. | ||
# Non-infectious causes include mechanical and chemical irritants. Surgical instruments or foreign objects like pessaries, condoms, diaphragms, cervical caps, or tampons can cause mechanical trauma. Chemical irritants cause allergic reactions and include soaps, laundry products, spermicides, latex, vaginal douches, and contraceptive creams.<ref name=":0">Iqbal U, Wills C. Cervicitis. [Updated 2022 Jan 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK562193/ (accessed 12.5.2022)</ref> | |||
== Epidemiology == | |||
The exact prevalence of cervicitis is difficult to determine as there is a lack of a standard definition and variation by population. Sexual activity is the main risk factor for the infectious causes with it possibly affecting about 30%-40% of the patients seen in sexually transmitted infection (STI) clinics. | |||
* | * The highest incidence is in sexually active women aged 15 to 24. | ||
* It is more common in human immunodeficiency virus (HIV) positive women, with an estimate of 7400 per 100,000 women diagnosed with HIV<ref name=":0" />.<br> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
| Line 23: | Line 22: | ||
*If symptomatic, person may experience vaginal discharge, dyspareunia, intermenstrual bleeding, or postcoital bleeding <ref name="Singh" /> | *If symptomatic, person may experience vaginal discharge, dyspareunia, intermenstrual bleeding, or postcoital bleeding <ref name="Singh" /> | ||
*Occasionally will present in an abnormal fashion, such as a cervical growth or uterovaginal prolapse, but that is rare and usually due to delayed or no treatment <ref name="Singh" / | *Occasionally will present in an abnormal fashion, such as a cervical growth or uterovaginal prolapse, but that is rare and usually due to delayed or no treatment <ref name="Singh" /> | ||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
In many cases, Mycoplasma Genitalium bacteria occurs simultaneously with cervicitis | In many cases, Mycoplasma Genitalium bacteria occurs simultaneously with cervicitis. Gonorrhea and chlamydia is also commonly found in correlation with cervicitis <ref name="Taylor">Taylor S, Lensing S, Lee J, et al. Prevalence and treatment outcome of cervicitis of unknown etiology. Sexually Transmitted Diseases [serial online]. May 2013;40(5):379-385. Available from: CINAHL with Full Text, Ipswich, MA. Accessed February 23, 2017.</ref><ref name="Sheeder et al">Sheeder J, Stevens-Simon C, Lezotte D, Glazner J, Scott S. Cervicitis: To Treat or Not To Treat? The Role of Patient Preferences and Decision Analysis. Journal Of Adolescent Health [serial online]. December 2006;39(6):887-892. Available from: PsycINFO, Ipswich, MA. Accessed March 22, 2017</ref> Untreated, cervicitis can lead to pelvic inflammatory disease (PID) <ref name="Sheeder et al" /> | ||
== Diagnostic Tests/Lab Tests/Lab Values == | == Diagnostic Tests/Lab Tests/Lab Values == | ||
In order to diagnose a culture is taken to look for mucopurulent discharge <ref name="Lusk et al">Lusk M, Garden F, Rawlinson W, Naing Z, Cumming R, Konecny P. Cervicitis aetiology and case definition: a study in Australian women attending sexually transmitted infection clinics. Sexually Transmitted Infections [serial online]. May 2016;92(3):175-181. Available from: MEDLINE, Ipswich, MA. Accessed February 23, 2017.</ref> | In order to diagnose a culture is taken to look for mucopurulent discharge <ref name="Lusk et al">Lusk M, Garden F, Rawlinson W, Naing Z, Cumming R, Konecny P. Cervicitis aetiology and case definition: a study in Australian women attending sexually transmitted infection clinics. Sexually Transmitted Infections [serial online]. May 2016;92(3):175-181. Available from: MEDLINE, Ipswich, MA. Accessed February 23, 2017.</ref> A culture is taken to look for specific bacteria like chlamydia, gonorrhea, or mycoplasma genitalium <ref name="Lusk et al" /> | ||
== Treatment == | |||
Treatment may not be needed for cervicitis if a sexually transmitted infection is not the cause. | |||
== | |||
If an infection is suspected, the main goal of treatment is to eliminate the infection and prevent it from spreading to the uterus and fallopian tubes, or if pregnant, to the baby. Depending on what organism is causing the infection the following may be prescribed: | |||
* | * [[Antibiotics]] | ||
* Antifungal medications | |||
* Antiviral medications | |||
The partner may be treated to make sure client does not get infected again. Sex should not be resumed till client and partner have finished treatment. Cervicitis increases the amount of virus that is shed from the cervix, increasing the chances of infecting a partner. | |||
Nondrug treatments like douches or yogurt-based therapy do not work for cervicitis and may actually worsen symptoms. They are not recommended<ref>Web md Cervicitis Available:https://www.webmd.com/women/guide/cervicitis (accessed 12.5.2022)</ref>. | |||
== References == | |||
== References | |||
<references /> | <references /> | ||
| Line 101: | Line 50: | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
[[Category:Womens Health]] | |||
[[Category:Global Health]] | |||
[[Category:Communicable Diseases]] | |||
Latest revision as of 23:44, 13 May 2022
Introduction[edit | edit source]
Cervicitis is inflammation of the cervix, the donut-shaped opening that connects the vagina to the uterus. It can be acute or chronic; with chronic occurring due to inadequate treatment or recurrent inflammation[1] Non-specific cervicitis is the most common; meaning that it is unrelated to an STI like chlamydia or gonorrhea [2] A single instance or acute cervicitis is usually due to an infection like chlamydia or gonorrhea, while chronic is typically due to a non-infectious source[3] If left untreated cervicitis can lead to pelvic inflammatory disease[2]
Etiology[edit | edit source]
The etiology is broadly classified into infectious and non-infectious.
- Infectious agents include Neisseria gonorrhea, Chlamydia trachomatis, and less commonly, herpes simplex, Trichomonas vaginalis, and Mycoplasma genitalium.
- Non-infectious causes include mechanical and chemical irritants. Surgical instruments or foreign objects like pessaries, condoms, diaphragms, cervical caps, or tampons can cause mechanical trauma. Chemical irritants cause allergic reactions and include soaps, laundry products, spermicides, latex, vaginal douches, and contraceptive creams.[4]
Epidemiology[edit | edit source]
The exact prevalence of cervicitis is difficult to determine as there is a lack of a standard definition and variation by population. Sexual activity is the main risk factor for the infectious causes with it possibly affecting about 30%-40% of the patients seen in sexually transmitted infection (STI) clinics.
- The highest incidence is in sexually active women aged 15 to 24.
- It is more common in human immunodeficiency virus (HIV) positive women, with an estimate of 7400 per 100,000 women diagnosed with HIV[4].
Characteristics/Clinical Presentation[edit | edit source]
In many case cervicitis remains asymptomatic
- If symptomatic, person may experience vaginal discharge, dyspareunia, intermenstrual bleeding, or postcoital bleeding [1]
- Occasionally will present in an abnormal fashion, such as a cervical growth or uterovaginal prolapse, but that is rare and usually due to delayed or no treatment [1]
Associated Co-morbidities[edit | edit source]
In many cases, Mycoplasma Genitalium bacteria occurs simultaneously with cervicitis. Gonorrhea and chlamydia is also commonly found in correlation with cervicitis [5][6] Untreated, cervicitis can lead to pelvic inflammatory disease (PID) [6]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
In order to diagnose a culture is taken to look for mucopurulent discharge [7] A culture is taken to look for specific bacteria like chlamydia, gonorrhea, or mycoplasma genitalium [7]
Treatment[edit | edit source]
Treatment may not be needed for cervicitis if a sexually transmitted infection is not the cause.
If an infection is suspected, the main goal of treatment is to eliminate the infection and prevent it from spreading to the uterus and fallopian tubes, or if pregnant, to the baby. Depending on what organism is causing the infection the following may be prescribed:
- Antibiotics
- Antifungal medications
- Antiviral medications
The partner may be treated to make sure client does not get infected again. Sex should not be resumed till client and partner have finished treatment. Cervicitis increases the amount of virus that is shed from the cervix, increasing the chances of infecting a partner.
Nondrug treatments like douches or yogurt-based therapy do not work for cervicitis and may actually worsen symptoms. They are not recommended[8].
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Singh N, Arora A. An Extreme Case of Chronic Cervicitis Mimicking Cervical Cancer and Causing Third-Degree Prolapse. Journal Of Gynecologic Surgery [serial online]. December 2014;30(6):380-382. Available from: Academic Search Complete, Ipswich, MA. Accessed February 23, 2017.
- ↑ 2.0 2.1 Pollett S, Calderon M, Heitzinger K, Solari V, Montano S, Zunt J. Prevalence and predictors of cervicitis in female sex workers in Peru: an observational study. BMC Infectious Diseases [serial online]. April 30, 2013;13:195. Available from: MEDLINE, Ipswich, MA. Accessed February 23, 2017.
- ↑ Efosa O, Uwadiegwu A. Cytopathological Examination and Epidemiological Study of Cervicitis in Commercial Sex Workers (Csws) in Coal City (Enugu), Nigeria. Ethiopian Journal Of Health Sciences [serial online]. July 2015;25(3):225-230. Available from: Academic Search Complete, Ipswich, MA. Accessed April 4, 2017.
- ↑ 4.0 4.1 Iqbal U, Wills C. Cervicitis. [Updated 2022 Jan 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK562193/ (accessed 12.5.2022)
- ↑ Taylor S, Lensing S, Lee J, et al. Prevalence and treatment outcome of cervicitis of unknown etiology. Sexually Transmitted Diseases [serial online]. May 2013;40(5):379-385. Available from: CINAHL with Full Text, Ipswich, MA. Accessed February 23, 2017.
- ↑ 6.0 6.1 Sheeder J, Stevens-Simon C, Lezotte D, Glazner J, Scott S. Cervicitis: To Treat or Not To Treat? The Role of Patient Preferences and Decision Analysis. Journal Of Adolescent Health [serial online]. December 2006;39(6):887-892. Available from: PsycINFO, Ipswich, MA. Accessed March 22, 2017
- ↑ 7.0 7.1 Lusk M, Garden F, Rawlinson W, Naing Z, Cumming R, Konecny P. Cervicitis aetiology and case definition: a study in Australian women attending sexually transmitted infection clinics. Sexually Transmitted Infections [serial online]. May 2016;92(3):175-181. Available from: MEDLINE, Ipswich, MA. Accessed February 23, 2017.
- ↑ Web md Cervicitis Available:https://www.webmd.com/women/guide/cervicitis (accessed 12.5.2022)