Case Study - Rehabilitation of Post Concussion Syndrome
Abstract[edit | edit source]
Introduction[edit | edit source]
As a condition that has become increasingly researched and well-understood in recent years, post-concussion syndrome is something that all physiotherapists should be familiar with and prepared to treat. Post-concussion syndrome describes persistent cognitive and physical symptoms beyond the typical 1-3 month period during which most concussions recover[1]. As the literature has developed, it has become recognized that 10-30% of mild head trauma may result in symptoms that last for months to years[2]. With this in mind, physiotherapists must be vigilant in recognizing when a patient is likely experiencing the condition.
This page outlines a case study of a 19-year old female athlete experiencing concussion, and subsequently post-concussion syndrome. The patient presents in a complex manner as she has experienced several recent concussions prior to the one in question. During the case, she develops persistent symptoms and psychosocial comorbidities that – as suggested in the literature[2][3] – make diagnosis and treatment more complicated. The purpose of this case study is to provide an overview of the condition and its broad range of possible symptoms, describe a unique presentation of the condition, discuss assessment methods, and present relevant treatment approaches used to achieve the patient’s goal of returning to school and sport.
Client Characteristics[edit | edit source]
A 19-year old female playing for Team Ontario ringette suffered a contre-coup blow to the head during a scrimmage in practice. The patient collided with another teammate, crashing head-first into the ice. Initially, she did not feel any different other than experiencing some dizziness, but reported that she began experiencing extreme nausea, vomiting, headache, dizziness and double vision the following day. Over the next two weeks, she was closely monitored by doctors while attempting to continue living in residence at university, however she was sent home following an increase of 10 points in her SCAT5 symptom score from day 1 post-injury to day 14. Once at home, she was dark roomed for long periods of time until deemed stable to return to school. She experienced several relapses in her recovery and often experienced fainting spells lasting as long as one hour from continuous studying and attempts at physical activity.
She reported that she had previously suffered three concussions in the last 8 months. She noted that her recovery time has increased from the first concussion (1 week) to the third concussion (1 month), however each time she followed a return to play protocol set out by her coaches. Since her concussion symptoms have been present and persisting for over 3 months prior to the initial assessment with the author, she was therefore diagnosed with Post-Concussion Syndrome (PCS) by her sports medicine doctor. She has decided to attempt physiotherapy upon request from her doctor to see if she can reduce her symptoms and increase her quality of life.
Examination Findings[edit | edit source]
On examination, she subjectively spoke about the pain that she was experiencing. She explained that in the absence of light and activity, she had dull, achy headaches resulting in a 4/10 on the NPRS scale. However, with increased light, noise, reading and neck pain, her headaches become sharp and shooting from the base of her neck into her skull, resulting in a 8/10 on the NPRS scale. Sleep was not affected, and she often described it as being her only moments of relief. It was also very apparent that she was experiencing an identity crisis as her lifelong athletic career was suddenly over, characterized by emotional responses[4] such as depression, loss of sense of self and anger. She often mentioned that she did not know who she was without her sport, and was very angry towards her situation and the girl who injured her. Her family also noted changes in her personality including introvertedness, depression, anxiety, and loss of emotional control.
She had been a highly functioning young woman previously, a competitive ringette player who practiced at least 5 times per week in addition to completing her degree in Kinesiology. Her main objective was to continue to pursue her degree while also continuing to play top-level ringette, with the hope of medaling at the National Ringette Championships. With this most recent injury, her chief concern is to be able to return to school with strategies to minimize aggravating factors/symptoms while attempting to complete her degree. She was able to study for moderate amounts of time (20-30 minutes with breaks) however long-term studying needed for exams caused major PCS symptoms such as dizziness, nausea, vomiting and fainting. She was still able to manage independently in residence, and would only have moderate trouble taking transportation (cars, buses, etc.).
Objective Assessment:[edit | edit source]
Sport Concussion Assessment Tool 5th Edition (SCAT-5)
SCAT 5 was completed by the Team Ontario Trainers immediately following the impact and a copy of the results were given to the physiotherapist for reference. The SCAT-5 is the most current version of the SCAT assessment tool used to screen for presence of concussions in sport settings. The SCAT-5 addresses the following subtopics:
1) Athlete Background
2) Symptom Evaluation
3) Cognitive Screening (Orientation, Immediate Memory, Concentration)
4) Neurological Screen & Balance Examination
5) Delayed Recall
6) Decision
- Nystagmus detected when testing visual tracking in both eyes (stare at finger moving in an H pattern)
- Romberg Test: +’ve with eyes closed, 30s bilaterally with eyes open
- Tandem Gait was VERY hard
- Short-term memory impairment
- Poor delayed recall
During the initial assessment, the physiotherapist chose several other outcome measures as a baseline to track progress over time.
Community Balance and Mobility Scale (CBMS)
was chosen as a suitable outcome measure to track progress over time as the patient is a young, high functioning and ambulatory individual that is having balance impairments as a result of her concussions.
Score: 42/96 where MCID = 8[5]
PHQ-9 is a screening questionnaire to measure the severity of depression pertaining to an individual's status. the PHQ-9 was indicated for this patient due to her apparent psychological distress and relative depression she reported as a result of the injury.
Score: 11; Moderate. The physiotherapist should use their clinical judgement and be aware of a considerable psychological impact on treatment and recovery.
Scan Exam Cleared
Cranial Nerve testing: Within Normal Limits bilaterally for all cranial nerves
Upper Motor Neuron Testing: Negative
Palpation: suboccipitals, paraspinals, sternocleidomastoid, and upper fiber trapezius were tender on palpation
Clinical Hypothesis/Impression[edit | edit source]
A major problem that the patient faced during rehabilitation was the inability to gradually return to school due to the high demand of a bachelor of science program. This was affecting her progression as she would often relapse when studying for exams or attempting to complete assignments. Furthermore, the forward head posture often demonstrated by students while studying was aggravating already strained neck muscles (whiplash during injury), further contributing to her daily headaches. The combination of an incessant workload at school and the severity of her symptoms due to repeated impacts to her head (4 concussions in 8 months) was having negative psychological effects, adding to her already altered/heightened psychological state as she was working through her identity crisis. The pain, nausea, vomiting, dizziness, diplopia and fainting that she would often experience as a result of exertion was not only disabling but was also very unnerving for a student living alone and away from home.
Patient is a previously high functioning athlete and 19 y/o university student with her 4th concussion in 8 months who presents with pain, nausea, dizziness, fainting, nystagmus, poor balance, poor memory recall, decreased movement of the neck and personality changes.
Due to the number of concussions in a short period of time and the severity of the patients persisting symptoms, the focus will be on return to school as return to sport is not foreseen, nor advised.
Excellent candidate for physiotherapy activities aimed at increasing balance, range, VOR and proprioception; functional mobility, and optimizing participation in activities suitable for the patients return to school protocol.
Problem List:
- Pain, nausea, vomiting, dizziness, fainting, diplopia
- Balance and postural control problems
- Decreased range of motion of neck muscles
- Reduced level of cognition (memory and recall)
Intervention[edit | edit source]
The treatment program was designed based on the patients assessment findings and will be completed to the patients level of tolerance, following a similar protocol to Fowler-Kennedy Guidelines[1]. These should not exceed patients limitations and should not cause the reproduction of the patients symptoms or fatigue in the first few sessions.
1) Range of Motion Exercises – unidirectional and/or combined movements
- AROM flexion, extension, rotation and side flexion, chin tucks
- Progress to isometric exercises
2) Mobilizations – as per assessment findings
3) Deep Neck Flexor (DNF) training Can be performed in multiple positions
1. sitting (with/without head support)
2. supine
3. 4-point kneeling.
- Can be progressed to involve DNE recruitment
4) Deep Neck Extensor (DNE) training; can also be performed in multiple position and in combination with DNF recruitment
5) Muscle Extensibility Exercises
- Stretching: deep neck flexor stretching
- Muscle energy techniques
6) Postural correction
- Upper and lower cervical spine motor control, strength and endurance
- Cervicoscapulothoracic muscles motor control, strength and endurance
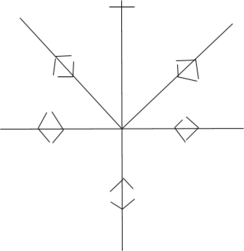
1. Joint position sense
- Ex. move head towards a stimulus and relocate back to neutral (eyes open, eyes closed)
2. Cervical movement sense
- Ex. trace patterns mounted on a wall with a laser
3. Gaze stability
4. Saccades
5. Smooth pursuit
6. Head-eye coordination
- Ex. eyes follow a stimulus, head remains in neutral position
7. Balance
Cervical Movement Control
These exercises can be progressed by altering the base of support (width, stable vs unstable surface) and adding perturbations, internal to begin followed by external.
8) Acupuncture
- Points in cervical and cranial regions
- Found to have longer-lasting therapeutic effects for PCS symptoms such as headaches, neck pain and nausea[6].
TREATMENT FOR BALANCE & VISUAL PROCESSING
A component of the treatment plan will include interventions to address the limitations in balance, postural control and dizziness/associated visual tracking limitations, following a similar protocol to the Fowler-Kennedy guidelines.
The balance limitations will be addressed first working on basic balance exercises as follows:
1) 2 feet to one foot,
2) changing the surface (firm to foam surfaces),
3) eyes opened and closed
These exercises will address the basic systems contributing to balance. We can progress these basic exercises as follows:
- Inclination of the surface may be changed
- Add internal perturbations such as moving other limbs, changing BOS – i.e tandem stance
- Add a dual task component (adding cognitive tasks while maintaining balance)
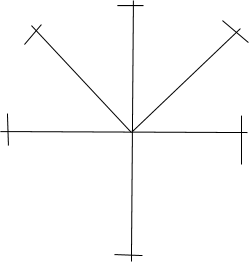
The visual tracking/dizziness limitations will be addresses through vestibulo-ocular reflex (VOR) exercises which may include the following:
1) Substitution exercises – move eyes to a target and then head
2) VOR exercises: keep focused on target while shaking head back and forth - do it by moving head side to side, up and down.
Once balance and VOR factors have been addressed they can actually be combined in order to increase the level of difficulty within the tolerance of the patient. For example, standing on a bosu-ball (challenging balance) while keeping eyes focused on a target while moving head back and forth.
Outcome[edit | edit source]
After a month of treatment by her physiotherapist, the patient has seen significant improvements in her status since starting treatment.
Her SCAT5 score was routinely re-assessed to monitor changes on a weekly basis and overall has significantly improved including a marked increase in time score for the Rhomberg test as well as improvements in convergence, Vestibulo-Occular Reflex, balance and an overall reduction in severity as well as prevalence of symptoms (nystagmus, diplopia, dizziness, nausea etc).
The patient’s limited cervical range of motion and myofascial tone was addressed in treatment through the use of soft tissue release, motor control exercises, postural correction, and neck proprioception training. As a result, the patient’s neck range of motion in all directions has improved to within normal limits since her initial assessment. The patient’s NPRS score at the time of reassessment was also reduced to 0/10 during rest and at 2/10 at its worst.
Cognitive improvements were also subjectively noted. However, memory and cognition was not a direct focus of the physical therapy intervention and therefore it cannot be inferred that improvements were a direct result of the treatment.
The patient’s balance and proprioception was also challenged by use of numerous different techniques in her treatment plan.
After 1 month of treatment and home exercise prescription, the patient was able to demonstrate her ability to balance 30 seconds with eyes open, closed, and on various surfaces and inclines. Tandem balance was still challenging, however, her time increased from 3 seconds, showing an improvement in overall performance.
The patient has also been diligently following the Return to play and Return to school Protocol, requiring a Licensed Healthcare professional (physiotherapist) to sign off on each stage of the graded programs.
Due to the degree of psychological distress the patient was dealing with as a result of her concussions and her inability to return to sports, she was referred to counsellor for mental health consultation.
Discussion[edit | edit source]
Self-Study Questions[edit | edit source]
1) What are typical signs and symptoms of post-concussion syndrome?
- Nausea
- Dizziness
- Headache
- Memory Deficits
- All of the Above
2) What is the minimum time that symptoms must persist to be diagnosed with Post-concussion Syndrome?
- 2 weeks
- 1-3 months
- 6 months
- 1 year
3) Which of the following is/are commonly used as an intervention for Post-concussion Syndrome:
- Balance Training
- Acupuncture
- Cervical Motor Control
- A & B
- All of the Above
References[edit | edit source]
- ↑ 1.0 1.1 Fowler Kennedy Sport Medicine. Post-Concussion Syndrome Management Guidelines. Available from: https://www.fowlerkennedy.com/wp-content/uploads/2017/02/Post-Concussion-Treatment-Guidelines.pdf (Accessed 7 May 2019)
- ↑ 2.0 2.1 Hugentobler JA, Vegh M, Janiszewski B, Quatman‐Yates C. Physical therapy intervention strategies for patients with prolonged mild traumatic brain injury symptoms: a case series. International journal of sports physical therapy. 2015 Oct;10(5):676.
- ↑ Ontario Neurotrauma Foundation. Guideline For Concussion/Mild Traumatic Brain Injury & Persistent Symptoms, 3rd Edition, For Adults Over 18 Years Of Age. Available from: https://braininjuryguidelines.org/concussion/fileadmin/media/adult-concussion-guidelines-3rd-edition.pdf (Accessed 7 May 2019).
- ↑ Green SL, Weinberg RS. Relationships among athletic identity, coping skills, social support and the psychological impact of injury in recreational participants. J Appl Psychol [Internet]. 2001 Fall [cited 2007 Oct 24];13(1):40-59. Available from:https://www.tandfonline.com/doi/abs/10.1080/10413200109339003#aHR0cHM6Ly93d3cudGFuZGZvbmxpbmUuY29tL2RvaS9wZGYvMTAuMTA4MC8xMDQxMzIwMDEwOTMzOTAwMz9uZWVkQWNjZXNzPXRydWVAQEAw
- ↑ Howe J, Inness E, Wright V. The Community Balance and Mobility Scale [Internet]. Tbims.org. 2011 [cited 5 May 2018]. Available from: http://www.tbims.org/cbm/index.html
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4685187/