Bladder Considerations with Spinal Cord Injury
Original Editor - Wendy Oelofse
Top Contributors - Ewa Jaraczewska, Jess Bell and Kim Jackson
Introduction[edit | edit source]
The bladder becomes neurogenic when it no longer receives an input from the brain to empty or store urine. This interruption in communication can occur after a spinal cord injury (SCI) as the brain is not able to send or receive signals to and from the organs below the level of injury. Urologic complications can be severe and life threatening. This article supplies additional information on managing bladder dysfunction after spinal cord injury for the Plus course: Bladder and Bowel Considerations with Spinal Cord Injury.
Bladder Dysfunction in Spinal Cord Injury[edit | edit source]
The location of the spinal cord lesion defines bladder dysfunction.
Spastic Bladder[edit | edit source]
- Observed in people with a spinal cord injury above T12 (upper motor neuron SCI)
- Limited/no ability to feel bladder fullness
- Limited/no control of the sphincter muscle to hold urine.
- Spastic/overactive bladder causing involuntary reflex voiding and incontinence – the voiding reflex is intact between the spinal cord and bladder.
- Detrusor sphincter dyssenergia (DSD) may also be present
- this is when the bladder contracts to void but the sphincter remains tight
- this causes increased pressure in the bladder which can result in urine being forced back up the ureters to the kidney, which can result in kidney damage.
- May experience incomplete bladder emptying.
Flaccid Bladder[edit | edit source]
- Observed in people with a SCI below T12 (Lower motor neuron SCI)
- Limited/no ability to feel bladder fullness
- The bladder muscle cannot contract to empty the bladder resulting in the bladder overfilling( urinary retention)
- Voiding reflex is not intact between the bladder and spinal cord
- The sphincter muscle can also be relaxed causing urine to leak out of the bladder when it overfills or during some activities such as transfers, sneezing coughing etc.
- Unable to empty bladder voluntarily
Table 1 summarises storage and voiding dysfunction in relation to the level of the spinal cord lesion.
| Spinal Cord Lesion | Bladder dysfunction |
|---|---|
| Suprasacral (Upper Motor Neuron Injury) |
|
| Mix (Upper and Lower Motor Neuron Injury) |
|
| Sacral (Lower Motor Neurone Injury) |
|
Management of Bladder Dysfunction[edit | edit source]
Spastic Bladder Management[edit | edit source]
Goals:[2]
- To reduce overactivity in the bladder wall muscle to decrease or eliminate accidents, leaking, and wetness.
- To prevent high detrusor pressure and damage to the upper urinary tract.
Draining the Bladder[edit | edit source]
The following methods can be used to drain the bladder:[3][2]
- Indwelling catheters: [3]
- Indwelling urethral catheter is not recommended unless patient has difficulty self-catheterising. Example: patient with quadriplegia or in the presence of urethral abnormalities.
- Regular follow-up with imaging and cystoscopy is required due to increase the risks of UTI, renal impairment, bladder stone formation, urethral stricture, urethral erosion, and bladder cancer.
- A suprapubic catheter is easier to manage and is a valuable option for patients with quadriplegia.
- Condom catheters
- Use to catch leaks but not for emptying the bladder
- Intermittent catheterisation
- Clean Intermittent Catheterisation (CIC)
- Sterile Intermittent Catheterisation (much higher cost)
- Over 45% of patients who relied on CIC switched to urethral or suprapubic catheters after 11 years of follow-up based on their preference and physician recommendation. [4]
Intermittent catheterisation (CIC)[edit | edit source]
Women: Finding the right hole (meatus) can be difficult when first doing an IC. The meatus is located just below your clitoris and above the vagina. A magnified mirror may help to see the area. If mistakenly the catheter was inserted into the vagina, it should be left there as a landmark when new catheter is being inserted. A clean catheter should be inserted ABOVE the vagina into the meatus.
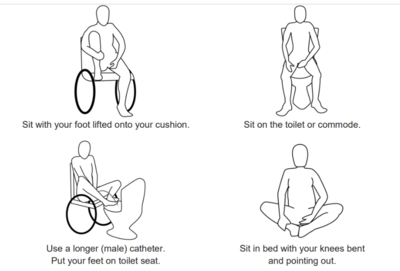
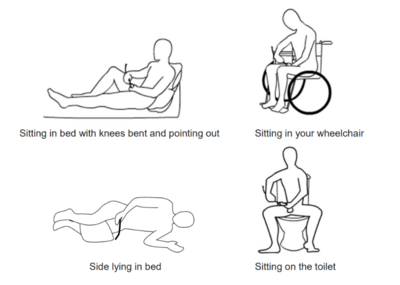
Recommended positions for self-catheterisation for women:
Watch this video to learn about self-catheterisation technique for women with spinal cord injuries. This video shows self-catheterisation performed in bed.
Men: Inserting the catheter can be done in different positions: sitting in bed, sidling, sting in the wheelchair or on the toilet.
Recommended positions for self-catheterisation for men:
Watch the video to learn about tools and technique for intermittent catheterisation for men with spinal cord injuries:
Medications[edit | edit source]
- Anticholinergic medications (sometimes called antimuscarinic medications) may help to relax the bladder muscles.[2]
- This can help to reduce pressure within the bladder, increase the ability of the bladder to hold urine, and help reduce incontinence.Overall it improves compliance and quality of life[3][2]
- Side effects, depending on the choice of the medication, may include memory and cognition impairment, visual blurring, oral dryness, constipation, tachycardias and arrhythmias. [3]
Botulin Injections[edit | edit source]
- Injecting small doses of some strains of botulinum toxin (Botox) into muscles can help to reduce muscle spasms.
- Injections into the bladder wall muscle or the external sphincter muscle can help to relax these muscles to help prevent leaking and incontinence or to improve bladder emptying.
- The effects of these injections can last for 6 to 12 months.
Surgical Management[edit | edit source]
- Bladder augmentation surgery can increase the capacity of the bladder to hold urine. [3]
- Augmentation cystoplasty with a detubularized intestinal segment
- Augmentation cystoplasty with an ileal segment
- Augmentation cystoplasty with a colonic patch
- Incompetent sphincters can be treated with an artificial urinary sphincter (AUS), abdominal slings, or a transobturator tape procedure. [3]
Flaccid Bladder Management[edit | edit source]
Goals:[2]
- To prevent overfilling and increased pressure in the bladder
- To prevent leaking and wetness.
Draining the Bladder[edit | edit source]
- Intermittent catheterization or indwelling catheters
- Condom catheters or pouches may be used to catch leaks but not for emptying
Medication[edit | edit source]
- Alpha-adrenergic blockers are used to encourage the bladder sphincter muscles to relax to allow urine to flow out of the body.
- This can help with bladder emptying and help prevent urinary retention
Botulin Injections[edit | edit source]
See Spastic Bladder Management
Surgical Management[edit | edit source]
- Transurethral sphincterotomy [7]
- Stents
Bladder Irrigation[edit | edit source]
Bladder irrigation is a procedure that flushes the bladder using sterile liquid. Water, saline, acetic acid, or chlorhexidine can be used for this procedure. Watch this video to understand the bladder irrigation technique:
Complications of Bladder Dysfunction[edit | edit source]
The most common primary complications include urinary tract infection (UTI), urinary stones, and renal impairment
- Urinary tract infection is an infection of part of the urinary tract (kidneys, bladder or the connecting tubes
- Bladder or renal stones could cause reoccurring UTI’s[9]
- Renal impairment can be caused by reflux and high pressure bladder
Other primary complications include:
- Incontinence
- Bladder cancer [10]
Secondary complications include the following:
- Skin irritation and skin breakdown due to wetness from bladder complications
- Increased spasticity
- Autonomic dysreflexia characterised by a sudden rise in blood pressure in response to and irritating stimulus below the level of injury. It typically occurs in people with an injury at T6 and above
Resources[edit | edit source]
- Perez NE, Godbole NP, Amin K, Syan R, Gater DR Jr. Neurogenic Bladder Physiology, Pathogenesis, and Management after Spinal Cord Injury. J Pers Med. 2022 Jun 14;12(6):968.
- Chen YC, Ou YC, Hu JC, Yang MH, Lin WY, Huang SW, Lin WY, Lin CC, Lin VC, Chuang YC, Kuo HC; Taiwan Continence Society Spinal Cord Injury Study Group. Bladder Management Strategies for Urological Complications in Patients with Chronic Spinal Cord Injury. J Clin Med. 2022 Nov 20;11(22):6850.
- Spinal Cord Essentials. Handouts
- Decision Aid: Bladder Management After Spinal Cord Injury (SCI)
References[edit | edit source]
- ↑ Perez NE, Godbole NP, Amin K, Syan R, Gater DR Jr. Neurogenic Bladder Physiology, Pathogenesis, and Management after Spinal Cord Injury. J Pers Med. 2022 Jun 14;12(6):968.
- ↑ 2.0 2.1 2.2 2.3 2.4 Oelofse W. Bladder and Bowel Dysfunction in Spinal Cord Injury. Plus Course 2024
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Taweel WA, Seyam R. Neurogenic bladder in spinal cord injury patients. Res Rep Urol. 2015 Jun 10;7:85-99.
- ↑ Wu SY, Jhang JF, Liu HH, Chen JT, Li JR, Chiu B, Chen SL, Kuo HC. Long-Term Surveillance and Management of Urological Complications in Chronic Spinal Cord-Injured Patients. J Clin Med. 2022 Dec 9;11(24):7307.
- ↑ CortreeTV. Self-catheterisation demo in bed | Spinal cord injury neurogenic bladder. Available from: https://www.youtube.com/watch?v=kxybiDtc-u0 [last accessed 19/01/2024]
- ↑ Craig Hospital. Bladder Management Tools for Men with Spinal Cord Injuries. Available from: https://www.youtube.com/watch?v=KxgjU41JVV8 [last accessed 19/01/2024]
- ↑ 7.0 7.1 7.2 7.3 Sphincterotomy, Artificial Sphincters, Stents and Related Approaches for Bladder Emptying. Available from https://scireproject.com/evidence/bladder-management/therapeutic-interventions-for-detrusor-overactivity-with-dsd-in-sci/enhancing-bladder-emptying-non-pharmacologically/sphincterotomy-artificial-sphincters-stents-and-related-approaches-for-bladder-emptying/ [last access 19.01.2024]
- ↑ Craig Hospital. Bladder Irrigation Procedure. Available from: https://www.youtube.com/watch?v=13eHF0BqBmY [last accessed 19/01/2024]
- ↑ Park YI, Linsenmeyer TA. A method to minimize indwelling catheter calcification and bladder stones in individuals with spinal cord injury. J Spinal Cord Med. 2001 Summer;24(2):105-8.
- ↑ Hess MJ, Zhan EH, Foo DK, Yalla SV. Bladder cancer in patients with spinal cord injury. J Spinal Cord Med. 2003;26(4):335–338.