Aetiology, Symptoms and Clinical Classifications of Temporomandibular Disorders
Top Contributors - Jess Bell, Wanda van Niekerk, Kim Jackson and Olajumoke Ogunleye
Introduction[edit | edit source]
The temporomandibular joint (TMJ) is considered one of the most complex joints in the body. It plays a significant role in dental occlusion and the neuromuscular system.[1]
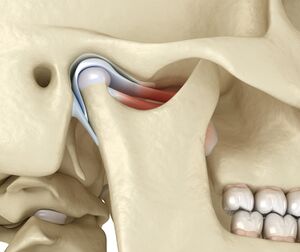
It has been classified as both a compound joint and a double joint. Compound joints typically consist of three or more bones, but the TMJ only has two bones. Instead of a third bone, an articular disc sits between the mandibular fossa and the condyle (Figure 1).[1]
The anatomy, biomechanics and physiology of the TMJ are discussed in detail here and here.
Causes of Facial Pain[edit | edit source]
Temporomandibular disorders (TMDs) are the most common non-dental cause of facial pain. Other acute causes of facial pain are:[2]
- Dental and oral causes
- Maxillary sinusitis
- Salivary gland disorders
- Neuropathic pain (trigeminal nerve region), such as:
- Trigeminal post-herpetic neuralgia
- Post-traumatic trigeminal pain / trigeminal neuropathic pain / atypical odontalgia
- Burning mouth syndrome
- Trigeminal neuralgia and its variants etc
- Vascular causes
- Giant cell arteritis should be considered in individuals aged over 50 years who present with temporal pain that mimics TMD
Chronic orofacial pain can be bilateral or unilateral.[2] The following article discusses specific causes of continuous or episodic orofacial pain:
Temporomandibular Disorders[edit | edit source]
Laplanche defines TMD as a muscular and articular disorder.[3] TMD encompasses various anatomical, histological and functional abnormalities, which affect the muscular and / or articular components of the TMJ and have variable clinical features.[4][5]
Epidemiology[edit | edit source]
The number of patients presenting to physiotherapy departments with TMJ pain is increasing.[6]
- Individuals aged 20 to 40 years report TMD more frequently[7]
- Women are more likely to experience TMD than men (with a ratio of around 3:1)[6]
While it is recognised that case numbers are rising, the reported prevalence of TMDs varies considerably in the literature. This variation is likely due to differences in:[7]
- Data collection methods
- Descriptive terminology
- Analytic methods
- Individual factors
A review by Manfredini and colleagues[8] found that:
- 45 percent of TMD patients have muscular pain
- 41 percent have disc derangement
- 34 percent have joint pain
In the general population:[8]
- 9.7 percent of individuals had muscular pain associated with TMD
- 11.4 percent had disc displacement
- 2.6 percent had TMJ joint disorders
35 percent of individuals may have asymptomatic TMD[7] and up to 75 percent of the adult population may be affected by TMJ pain.[6] However, it has been estimated that only 3.6 to 7.0 percent of people with TMD will require treatment.[7] People are most likely to seek treatment for pain (90 percent) and acoustic phenomena (65 percent).[6]
Symptoms[edit | edit source]
The following symptoms are associated with TMD:[1]
- Pain
- Usually in the preauricular area and / or the masticatory muscles
- NB pain is the most common emerging symptom
- Limited range of mandibular movement
- Presence of TMJ sounds, such as popping, clicking, grating or crepitus
- Earache, headache, jaw ache and facial pain
- Hypertrophy of masticatory muscles (not painful)
- Abnormal occlusal wear which is associated with oral parafunction (this may be related to tooth grinding and jaw clenching)
Internal Derangement of the Temporomandibular Joint[edit | edit source]
One of the most common intracapsular disorders associated with the TMJ occurs when the articular disc is positioned anteriorly in the joint (i.e. anterior subluxation / dislocation):[9]
- In severe cases, range of motion may be limited by luxation of the disc / condyle, which causes locking (this may or may not be painful)
- When locking occurs, the joint is no longer able to function according to the “rules” of a synovial joint - i.e pain-free, friction-free, good range of motion
- The click associated with TMD indicates that the joint is not free of friction[9]
Anterior disc displacement may be caused by a loss of normal arthrokinematics (i.e. joint movement pattern). In a normal joint, the following occurs during mouth opening:[9]
- Rotation of the joint occurs during the initial or middle range of motion
- This rotation occurs at the condyle surface, the inferior joint surface and the inferior joint surface of the disc
- For functional range of motion (35 to 40 mm) and effective mouth opening to occur, rotation is followed by a short anterior translatory glide (between the disc’s superior joint surface and the articular eminence)
- If this movement sequence is altered and there is a large anterior translatory glide of the mandible, the connective tissue posterior to the disc tends to overstretch
NB: Connective tissue usually enables the disc to return to its original position. However, if it remains stretched (i.e does not return to its usual position), the connective tissue will gradually give way and will no longer be able to return to its normal length. This might occur when an extreme range of motion places excessive demand on the ligaments or the joint capsule.[4]
While connective tissue is mainly non-elastic, it has the ability to “give” due to its wavy shape - this “give” resembles elasticity. The length of time required for the tissue to permanently lose its “elasticity” has not been documented. However, when elasticity is reduced in the TMJ, the disc starts to adopt an anterior position.[4]
This position leads to constant microtrauma and over time, the joint becomes unstable or hypermobile. Patients might experience clinical signs such as clicking or other joint sounds. Locking occurs when the disc finally adopts a position of complete anterior luxation. Some authors describe this as a “locked joint”.[4]
When a disc moves into this position, treatment is necessary to restore the normal functional relationship between the condyle, disc, and articular eminence.[9]
Causes of TMD[edit | edit source]
Navrátil and colleagues[6] propose a multifactorial theory to explain the causes of TMD. These causes can be divided into the following groups:[4][6]
- Inflammatory diseases
- Degenerative disease of the articular cartilage
- Changes in the position of the articular disc (i.e. dislocation)
- Extra-capsular area affected by extra-articular structures, along with masticatory muscles and ligaments
- Movement disorders such as hypermobility (see below)
- Changes in the cervical spine associated with cervical muscle spasm
- Accidents and / or injury
A joint might become overloaded for a number of reasons including:[4]
- Missing teeth
- Articulatory constraints
- Inappropriately sized prosthetics
- Faults in the mouth
Chang and colleagues propose the following specific causes of internal derangement of the TMJ:[7]
- Direct trauma
- Microtrauma
- Occlusal relationship
- Derangement of the TMJ extracellular matrix
- Synovial fluid
Classifying TMD[edit | edit source]
TMD can be classified into articular and non-articular disorders.[10]
Articular disorders such as:
- Osteoarthritis
- Trauma
- Infectious arthritis
- Prior surgery (iatrogenic)
- Gout / pseudogout (crystal arthropathies)
- Rheumatoid arthritis (RA) / juvenile RA
- Psoriatic arthritis
- Axial spondyloarthropathy (i.e. ankylosis spondylitis)
Articular disorders are usually classified based on the Wilkes’ Staging Classification for Internal Derangement of the TMJ:[10]
- Early stage
- Early / intermediate stage
- Intermediate stage
- Intermediate / late stage
- Late stage
The full classification is available here:
Non-articular disorders include:[10]
- Myofascial pain
- Acute muscle strain
- Muscle spasm
- Fibromyalgia
- Chronic pain conditions
- Myotonic dystrophy
Relationship between Malocclusion, Benign Joint Hypermobility Syndrome, Condylar Position and TMJ Symptoms[edit | edit source]
Barrera-Mora[11] examined the association between TMD, malocclusion, benign joint hypermobility syndrome (BJHS) and initial condylar position. They found that:[11][12]
- There is no “well-defined” initial position for the condyle in formal occlusion or malocclusion patterns
- There is no statistically significant relationship between BJHS, degree of condylar displacement or TMD
- There is, however, a relationship between malocclusion patterns (particularly malocclusion class II and open bite)
- Anterior crossbite may be a risk factor for TMJ symptoms
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Chang CL, Wang DH, Yang MC, Hsu WE, Hsu ML. Functional disorders of the temporomandibular joints: Internal derangement of the temporomandibular joint. Kaohsiung J Med Sci. 2018;34(4):223-30.
- ↑ 2.0 2.1 Zakrzewska JM. Differential diagnosis of facial pain and guidelines for management. Br J Anaesth. 2013;111(1):95-104.
- ↑ Laplanche O, Ehrmann E, Pedeutour P, Duminil G. TMD clinical diagnostic classification (Temporo Mandibular Disorders). J Dentofacial Anom Orthod. 2012;15(2):202.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Reboredo V. Aetiology, Causes, Symptoms, and Clinical Classifications of Temporomandibular Disorders Course. Physioplus, 2021.
- ↑ Calil BC, da Cunha DV, Vieira MF, de Oliveira Andrade A, Furtado DA, Bellomo Junior DP et al. Identification of arthropathy and myopathy of the temporomandibular syndrome by biomechanical facial features. Biomed Eng Online. 2020;19(1):22.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Navrátil L, Navratil V, Hajkova S, Hlinakova P, Dostalova T, Vranová J. Comprehensive treatment of temporomandibular joint disorders. CRANIO®. 2014;32(1):24-30.
- ↑ 7.0 7.1 7.2 7.3 7.4 Chang CL, Wang DH, Yang MC, Hsu WE, Hsu ML. Functional disorders of the temporomandibular joints: Internal derangement of the temporomandibular joint. Kaohsiung J Med Sci. 2018;34(4):223-30.
- ↑ 8.0 8.1 Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(4):453-62.
- ↑ 9.0 9.1 9.2 9.3 Rocabado M. Joint distraction with a functional maxillomandibular orthopedic appliance. J Craniomandibular Pract. 1984;2(4):358-63.
- ↑ 10.0 10.1 10.2 Liu F, Steinkeler A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin North Am. 2013;57(3):465-79.
- ↑ 11.0 11.1 Barrera-Mora JM, Espinar Escalona E, Abalos Labruzzi C, Llamas Carrera JM, Ballesteros EJ, Solano Reina E et al. The relationship between malocclusion, benign joint hypermobility syndrome, condylar position and TMD symptoms. Cranio. 2012;30(2):121-30.
- ↑ Cincinnati Children's Hospital Medical Center. Evidence-based clinical care guideline for Identification and Management of Pediatric Joint Hypermobility. CCHMC EBDM Website Guideline 43. 22 p.