Aetiology, Symptoms and Clinical Classifications of Temporomandibular Disorders: Difference between revisions
No edit summary |
No edit summary |
||
| Line 13: | Line 13: | ||
== Causes of Facial Pain == | == Causes of Facial Pain == | ||
Temporomandibular disorders (TMDs) are the most common non-dental cause of facial pain. Other acute causes of facial pain are:<ref>Zakrzewska JM. [https://onlinelibrary.wiley.com/doi/full/10.1016/j.kjms.2018.01.004 Differential diagnosis of facial pain and guidelines for management]. Br J Anaesth. 2013;111(1):95-104. </ref> | Temporomandibular disorders (TMDs) are the most common non-dental cause of facial pain. Other acute causes of facial pain are:<ref name=":1">Zakrzewska JM. [https://onlinelibrary.wiley.com/doi/full/10.1016/j.kjms.2018.01.004 Differential diagnosis of facial pain and guidelines for management]. Br J Anaesth. 2013;111(1):95-104. </ref> | ||
* Dental and oral causes | * Dental and oral causes | ||
| Line 26: | Line 26: | ||
* Vascular causes | * Vascular causes | ||
** [[Headaches and Dizziness|Giant cell arteritis]] should be considered in individuals aged over 50 years who present with temporal pain that mimics TMD | ** [[Headaches and Dizziness|Giant cell arteritis]] should be considered in individuals aged over 50 years who present with temporal pain that mimics TMD | ||
Chronic orofacial pain can be bilateral or unilateral.<ref name=":1" /> The following article discusses specific causes of continuous or episodic orofacial pain: | |||
* [https://onlinelibrary.wiley.com/doi/full/10.1016/j.kjms.2018.01.004 Differential diagnosis of facial pain and guidelines for management] | |||
== Temporomandibular Disorders == | |||
Laplanche defines TMD as a muscular and articular disorder.<ref>Laplanche O, Ehrmann E, Pedeutour P, Duminil G. TMD clinical diagnostic classification (Temporo Mandibular Disorders). J Dentofacial Anom Orthod. 2012;15(2):202.</ref> TMD encompasses various anatomical, histological and functional abnormalities, which affect the muscular and / or articular components of the TMJ and have variable clinical features.<ref>Reboredo V. Aetiology, Causes, Symptoms, and Clinical Classifications of Temporomandibular Disorders Course. Physioplus, 2021.</ref><ref>Calil BC, da Cunha DV, Vieira MF, de Oliveira Andrade A, Furtado DA, Bellomo Junior DP et al. [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-020-00764-5 Identification of arthropathy and myopathy of the temporomandibular syndrome by biomechanical facial features]. Biomed Eng Online. 2020;19(1):22.</ref> | |||
=== Epidemiology === | |||
The number of patients presenting to physiotherapy departments with TMJ pain is increasing.<ref name=":2">Navrátil L, Navratil V, Hajkova S, Hlinakova P, Dostalova T, Vranová J. Comprehensive treatment of temporomandibular joint disorders. CRANIO®. 2014;32(1):24-30. </ref> | |||
* Individuals aged 20 to 40 years report TMD more frequently<ref name=":3">Chang CL, Wang DH, Yang MC, Hsu WE, Hsu ML. [https://onlinelibrary.wiley.com/doi/full/10.1016/j.kjms.2018.01.004 Functional disorders of the temporomandibular joints: Internal derangement of the temporomandibular joint]. Kaohsiung J Med Sci. 2018;34(4):223-30. </ref> | |||
* Women are more likely to experience TMD than men (with a ratio of around 3:1)<ref name=":2" /> | |||
While it is recognised that case numbers are rising, the reported prevalence of TMDs varies considerably in the literature. This variation is likely due to differences in:<ref name=":3" /> | |||
* Data collection methods | |||
* Descriptive terminology | |||
* Analytic methods | |||
* Individual factors | |||
A review by Manfredini and colleagues<ref name=":4">Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(4):453-62. </ref> found that: | |||
* 45 percent of TMD patients have muscular pain | |||
* 41 percent have disc derangement | |||
* 34 percent have joint pain | |||
In the general population:<ref name=":4" /> | |||
* 9.7 percent of individuals had muscular pain associated with TMD | |||
* 11.4 percent had disc displacement | |||
* 2.6 percent had TMJ joint disorders | |||
35 percent of individuals may have asymptomatic TMD<ref name=":3" /> and up to 75 percent of the adult population may be affected by TMJ pain.<ref name=":2" /> However, it has been estimated that only 3.6 to 7.0 percent of people with TMD will require treatment.<ref name=":3" /> People are most likely to seek treatment for pain (90 percent) and acoustic phenomena (65 percent).<ref name=":2" /> | |||
== References == | == References == | ||
Revision as of 11:44, 19 October 2021
Top Contributors - Jess Bell, Wanda van Niekerk, Kim Jackson and Olajumoke Ogunleye
Introduction[edit | edit source]
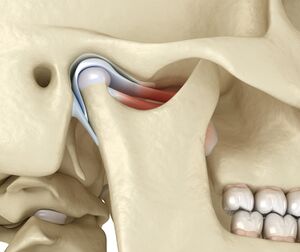
The temporomandibular joint (TMJ) is considered one of the most complex joints in the body. It plays a significant role in dental occlusion and the neuromuscular system.[1]
It has been classified as both a compound joint and a double joint. Compound joints typically consist of three or more bones, but the TMJ only has two bones. Instead of a third bone, an articular disc sits between the mandibular fossa and the condyle (Figure 1).[1]
The anatomy, biomechanics and physiology of the TMJ are discussed in detail here and here.
Causes of Facial Pain[edit | edit source]
Temporomandibular disorders (TMDs) are the most common non-dental cause of facial pain. Other acute causes of facial pain are:[2]
- Dental and oral causes
- Maxillary sinusitis
- Salivary gland disorders
- Neuropathic pain (trigeminal nerve region), such as:
- Trigeminal post-herpetic neuralgia
- Post-traumatic trigeminal pain / trigeminal neuropathic pain / atypical odontalgia
- Burning mouth syndrome
- Trigeminal neuralgia and its variants etc
- Vascular causes
- Giant cell arteritis should be considered in individuals aged over 50 years who present with temporal pain that mimics TMD
Chronic orofacial pain can be bilateral or unilateral.[2] The following article discusses specific causes of continuous or episodic orofacial pain:
Temporomandibular Disorders[edit | edit source]
Laplanche defines TMD as a muscular and articular disorder.[3] TMD encompasses various anatomical, histological and functional abnormalities, which affect the muscular and / or articular components of the TMJ and have variable clinical features.[4][5]
Epidemiology[edit | edit source]
The number of patients presenting to physiotherapy departments with TMJ pain is increasing.[6]
- Individuals aged 20 to 40 years report TMD more frequently[7]
- Women are more likely to experience TMD than men (with a ratio of around 3:1)[6]
While it is recognised that case numbers are rising, the reported prevalence of TMDs varies considerably in the literature. This variation is likely due to differences in:[7]
- Data collection methods
- Descriptive terminology
- Analytic methods
- Individual factors
A review by Manfredini and colleagues[8] found that:
- 45 percent of TMD patients have muscular pain
- 41 percent have disc derangement
- 34 percent have joint pain
In the general population:[8]
- 9.7 percent of individuals had muscular pain associated with TMD
- 11.4 percent had disc displacement
- 2.6 percent had TMJ joint disorders
35 percent of individuals may have asymptomatic TMD[7] and up to 75 percent of the adult population may be affected by TMJ pain.[6] However, it has been estimated that only 3.6 to 7.0 percent of people with TMD will require treatment.[7] People are most likely to seek treatment for pain (90 percent) and acoustic phenomena (65 percent).[6]
References[edit | edit source]
- ↑ 1.0 1.1 Chang CL, Wang DH, Yang MC, Hsu WE, Hsu ML. Functional disorders of the temporomandibular joints: Internal derangement of the temporomandibular joint. Kaohsiung J Med Sci. 2018;34(4):223-30.
- ↑ 2.0 2.1 Zakrzewska JM. Differential diagnosis of facial pain and guidelines for management. Br J Anaesth. 2013;111(1):95-104.
- ↑ Laplanche O, Ehrmann E, Pedeutour P, Duminil G. TMD clinical diagnostic classification (Temporo Mandibular Disorders). J Dentofacial Anom Orthod. 2012;15(2):202.
- ↑ Reboredo V. Aetiology, Causes, Symptoms, and Clinical Classifications of Temporomandibular Disorders Course. Physioplus, 2021.
- ↑ Calil BC, da Cunha DV, Vieira MF, de Oliveira Andrade A, Furtado DA, Bellomo Junior DP et al. Identification of arthropathy and myopathy of the temporomandibular syndrome by biomechanical facial features. Biomed Eng Online. 2020;19(1):22.
- ↑ 6.0 6.1 6.2 6.3 Navrátil L, Navratil V, Hajkova S, Hlinakova P, Dostalova T, Vranová J. Comprehensive treatment of temporomandibular joint disorders. CRANIO®. 2014;32(1):24-30.
- ↑ 7.0 7.1 7.2 7.3 Chang CL, Wang DH, Yang MC, Hsu WE, Hsu ML. Functional disorders of the temporomandibular joints: Internal derangement of the temporomandibular joint. Kaohsiung J Med Sci. 2018;34(4):223-30.
- ↑ 8.0 8.1 Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(4):453-62.