Acute Respiratory Distress Syndrome (ARDS): Difference between revisions
No edit summary |
No edit summary |
||
| Line 86: | Line 86: | ||
Added breath sounds on auscultation such as crackling. | Added breath sounds on auscultation such as crackling. | ||
Auscultation of the heart | Auscultation of the heart | ||
Cyanosis | Cyanosis | ||
| Line 94: | Line 92: | ||
Arterial Blood Gases | Arterial Blood Gases | ||
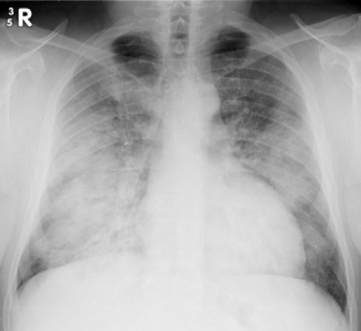
Chest X-Ray | Chest X-Ray | ||
Blood Tests | Blood Tests | ||
Sputum Culture | Sputum Culture | ||
CT Scan | CT Scan | ||
Heart Failure Examination | Heart Failure Examination | ||
| Line 112: | Line 105: | ||
· Suctioning (Open / Closed) | · Suctioning (Open / Closed) | ||
· Ventilator Hyperinflation (VHI) | · Ventilator Hyperinflation (VHI) | ||
· Positioning (see below). | · Positioning (see below). | ||
{{#ev:youtube|iMKybCBUzqM}} | |||
[/www.youtube.com/watch%3Fv%3DiMKybCBUzqM https://www.youtube.com/watch?v=iMKybCBUzqM] | [/www.youtube.com/watch%3Fv%3DiMKybCBUzqM https://www.youtube.com/watch?v=iMKybCBUzqM] | ||
| Line 141: | Line 133: | ||
This form of mechanical ventilation involves the delivery of CPAP with an intermittent release phase. Delivering CPAP over long periods is thought to maintain adequate lung volume and alveolar recruitment where the release is designed to aid the removal of CO2. Inspiration starts from a more benefical pressure-volume relationship thus helping oxygentation (reference). | This form of mechanical ventilation involves the delivery of CPAP with an intermittent release phase. Delivering CPAP over long periods is thought to maintain adequate lung volume and alveolar recruitment where the release is designed to aid the removal of CO2. Inspiration starts from a more benefical pressure-volume relationship thus helping oxygentation (reference). | ||
{{#ev:youtube|rgrBtILMmg}} | |||
<nowiki>https://www.youtube.com/watch?v=-rgrBtILMmg</nowiki> | <nowiki>https://www.youtube.com/watch?v=-rgrBtILMmg</nowiki> | ||
| Line 147: | Line 140: | ||
With HFO, a continuous distending pressure (CDP) is set and small tidal volumes are delivered at high frequencies with an oscillatory pump. Like the others previously described, this is another form of lung protective ventilation with constant lung recruitment. While a systematic review ([/www.bmj.com/content/bmj/340/bmj.c2327.full.pdf) https://www.bmj.com/content/bmj/340/bmj.c2327.full.pdf)] found that HFO may improve survival and is unlikely to cause harm, only 8 studies were analysed with few patients and wide confidence intervals. There was also no reports of blinding outcome assessors putting trials at risk of bias. | With HFO, a continuous distending pressure (CDP) is set and small tidal volumes are delivered at high frequencies with an oscillatory pump. Like the others previously described, this is another form of lung protective ventilation with constant lung recruitment. While a systematic review ([/www.bmj.com/content/bmj/340/bmj.c2327.full.pdf) https://www.bmj.com/content/bmj/340/bmj.c2327.full.pdf)] found that HFO may improve survival and is unlikely to cause harm, only 8 studies were analysed with few patients and wide confidence intervals. There was also no reports of blinding outcome assessors putting trials at risk of bias. | ||
{{#ev:youtube|IrTAo5GAVrw}} | |||
<nowiki>https://www.youtube.com/watch?v=IrTAo5GAVrw</nowiki> | <nowiki>https://www.youtube.com/watch?v=IrTAo5GAVrw</nowiki> | ||
| Line 170: | Line 164: | ||
ECMO consists of an extracorporeal blood circuit formed via an oxygenator and a pump. Two vascular accesses are established, one removes the venous blood and one infuses the oxygenated blood. After the blood has been removed from a major vein, it is pumped through a circuit that contains an oxygenator which oxygenates the blood and removes the carbon dioxide. The blood is then returned via the other cannula. | ECMO consists of an extracorporeal blood circuit formed via an oxygenator and a pump. Two vascular accesses are established, one removes the venous blood and one infuses the oxygenated blood. After the blood has been removed from a major vein, it is pumped through a circuit that contains an oxygenator which oxygenates the blood and removes the carbon dioxide. The blood is then returned via the other cannula. | ||
{{#ev:youtube|rmGM984aVKU}} | |||
== Clinical Manifestations == | == Clinical Manifestations == | ||
Revision as of 16:55, 26 July 2018
Original Editors - Students from Glasgow Caledonian University's Cardiorespiratory Therapeutics Project.
Top Contributors - Geoff Boudreau, Matt Ross, Lucinda hampton, Kim Jackson, Chrysolite Jyothi Kommu, Adam Vallely Farrell, Mohit Chand, Hugh Collins, Vidya Acharya, Admin and Michelle Lee
Definition[edit | edit source]
Acute respiratory distress syndrome (ARDS), is a life-threatening condition which is characterized by the sudden onset of severe dyspnea and hypoxemia[1].
In 1994, the American-European Consensus Conference defined ARDS as:
‘The acute onset of hypoxemia (arterial partial pressure of oxygen to fraction of inspired oxygen [PaO2/FiO2] less than or equal to 200mm Hg) with bilateral infiltrates on frontal chest radiograph, with no evidence of left atrial hypertension' [2]
Acute Lung Injury (ALI) was also described using similar criteria but with less severe hypoxemia (PaO2/FiO2 less than or equal to 300mm Hg)
More recently, the European Society of Intensive Care Medicine with endorsement from the American Thoracic Society and Society of Critical Care Medicine organized an expert panel to address the limitations of the AECC definition. As a result, the Berlin Definition[3] was created and is shown below:
ARDS is typically a secondary condition and is induced by the inflammation of the alveolar-capillary interface, which results in protein and fluid entering the interstitial space and alveoli. This pulmonary infiltrate and can lead to respiratory failure or, in approximately 20-30% of ARDS cases, death[4].
Although the lungs are the primary site of dysfunction for an individual with ARDS, many of the other systems will be compromised due to the decrease in blood oxygen levels[5]. Because ARDS can occur in an individual of any age, the systemic impact of the condition may also result in serious complications later in life for the individual.
Pathological Process[edit | edit source]
| Direct | Indirect |
|---|---|
| Pneumonia | Non-pulmonary sepsis |
| Aspiration of gastric contents | Multiple trauma |
| Lung contusion | Massive transfusion |
| Fat embolism | Pancreatitis |
| Near drowning | Cardiopulmonary Bypass |
| Inhalation injury | |
| Reperfusion Injury |
The exact mechanism of pathogenesis of ARDS are unknown, although it is well accepted that there is diffuse alveolar damage with:
- Damage of the alveolocapillary barrier leading to pulmonary oedema.
- A complex system of inflammatory infiltrates
- Surfactant Dysfunction.
Prior to these changes, surfactant turnover is significantly increased and the fluid that lines the epithelium also highlights fibrosing alveolitis early in the course of lung damage.
Once the alveolocapillary membrane is damaged, there is bidirectional leakage of fluids and proteins into the alveolus and as well as surfactant proteins and alveolar cytokines into the plasma. The epithelial barrier becomes disrupted with a proliferation of type 2 alveolar cells leading to surfactant dysfunction.
Cellular Involvement in ARDS[edit | edit source]
- Neutrophils: Most abundant in both the epithelial lining and alveolar histological specimens. Although the chemotaxic nature of neutrophils crossing the epithelium does not cause damage, their pro-inflammatory nature release reactive oxygen species, cytokines and a number of inflammatory mediators which contribute to the basement membrane damage.
- Alveolar Macrophages: These are the most common cell type and with interstitial macrophages play an important role in defence. In ARDS patients there is a progressive increase in alveolar macrophage number.
- Epithelium: Contained within the alveolar epithelial tissue are the highly metabolically active type 2 alveolar cells. Damaged epithelium leads to dysfunctional surfactant
The prevalence of people suffering from ARDS differs greatly between geographical areas. Although the reason for the differences are unclear, some have speculated that it may stem from the differences in healthcare systems[6]. The ability to diagnose and to differentiate the secondary condition is required to properly record and treat the patient. Future studies must be conducted in order to improve the ability to accurately diagnose the ARDS.
In Scotland, the incidence of ARDS is estimated at 16 cases/100,000 people per year. Because the onset of ARDS is brought on by another condition or traumatic event, the majority of the condition is seen within intensive care-unit (ICU) patients. During an 8-month long study, researchers have found that 8.1% of ICU patients were suffering from ARDS.
Clinical Presentation[edit | edit source]
- Acute Inflammatory Phase: Lasts 3 – 10 days and results in hypoxaemia and multi organ failure. Patients typically present with progressive dyspnoea, tachypnoea, cyanosis, hypoxic confusion and lung crepitations.
- Healing, Proliferative Phase: During this phase, lung scarring and pneumothoracies are common.
It is worth noting that in both phases, secondary systemic and chest infections are can occur.
Diagnostic Procedures[edit | edit source]
According to the National Heart, Lung and Blood Institute [7] a diagnosis will be made via the examination of your medical history, physical exam and test results.
Medical History[edit | edit source]
History of heart failure (which may be the reason for pulmonary oedema).
Has the patient had any of the direct or indirect clinical risk factors for ARDS.
Physical Exam[edit | edit source]
Added breath sounds on auscultation such as crackling. Auscultation of the heart Cyanosis
Test Results[edit | edit source]
Arterial Blood Gases Chest X-Ray Blood Tests Sputum Culture CT Scan Heart Failure Examination
Management / Interventions[edit | edit source]
Physiotherapy[edit | edit source]
For this type of patient you have to consider the risk vs reward of your intervention, particularly when the lungs are as fragile as they are. However, possible interventions for the ARDS patient may include:
· Suctioning (Open / Closed) · Ventilator Hyperinflation (VHI) · Positioning (see below).
[/www.youtube.com/watch%3Fv%3DiMKybCBUzqM https://www.youtube.com/watch?v=iMKybCBUzqM]
Medical
Mechanical Ventilation
As a result of the acute onset of hypoxaemic respiratory failure with an increased work of breathing, mechanical ventilation is commonplace. The pathophysiology of ARDS, and in particular the fibrosing aspect means that the method and delivery of support requires careful consideration to ensure that ventilator induced lung injury (VLII) does not occur.
Study
In the ARDS patient, the PEEP and tidal volume has to be reduced to reflect the available parts of the lung that are available for aeration. If not, this can lead to an overstretching of the lung, known as volutrauma due to decreased lung compliance. Repeated open and closing of the alveoli during tidal inflation can also cause injury to the lung tissue, known as alectotrauma. If the mechanical support is not titrated to the patient, both alectotrauma and volutrauma can increased the cytokines within the lung tissue which then may enter the systemic circulation and potentially lead to multiple organ failure.
Although perhaps oversimplified, the graph below attempts to highlight the optimal area for ventilation of the ARDS patient. The lower inflection point (LIP) is thought to be the pressure at which lung tissue is recruited. The upper inflection point (UIP) is the approximate pressure at which the alveoli become over distended which can potentially lead to damage. Therefore, the most optiumum poition to ventillatted would be between the two inflection points, on the steepest most complicant aspect of the curve.
Inverse Ratio Ventilation (IRV)
This mode of ventilation requires the alteration in the normal inspiratory / expiratory ratio of 1:2 to either 1:1 or 2:1. While this mode of ventilation aims to increase the aeration and collateral ventillatio of the poorly compliant lung, decreased expiration time may result in an increase in the PCO2. However, if hypercapnic acidosis occurs slowly then the intracellular acidosis will be well compensated, however any form of hypercapnia should be avoided in this with or those at risk of developing raised intracranial pressures. This is known as permissive hypercapnia.
A recent although small study by [/www.ncbi.nlm.nih.gov/pmc/articles/PMC4908089/pdf/40064%202016%20Article%202440.pdf https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4908089/pdf/40064_2016_Article_2440.pdf] showed that IRV provided acceptable gas exchange without complications for 13 people with ARDS.
Airway Pressure Release Ventillation (APRV)
This form of mechanical ventilation involves the delivery of CPAP with an intermittent release phase. Delivering CPAP over long periods is thought to maintain adequate lung volume and alveolar recruitment where the release is designed to aid the removal of CO2. Inspiration starts from a more benefical pressure-volume relationship thus helping oxygentation (reference).
https://www.youtube.com/watch?v=-rgrBtILMmg
High Frequency Oscillation (HFO)
With HFO, a continuous distending pressure (CDP) is set and small tidal volumes are delivered at high frequencies with an oscillatory pump. Like the others previously described, this is another form of lung protective ventilation with constant lung recruitment. While a systematic review ([/www.bmj.com/content/bmj/340/bmj.c2327.full.pdf) https://www.bmj.com/content/bmj/340/bmj.c2327.full.pdf)] found that HFO may improve survival and is unlikely to cause harm, only 8 studies were analysed with few patients and wide confidence intervals. There was also no reports of blinding outcome assessors putting trials at risk of bias.
https://www.youtube.com/watch?v=IrTAo5GAVrw
Prone Positioning
Placing the ARDS patient into prone will result in a significant increase in PaO2 for approximately 70% of the patients. By placing the patient into prone, there is an improvement in the recruitment of the dorsal aspect of the lung resulting in a more evenly distributed perfusion and improving V/Q matching.
Evidence has shown that prone positioning is benefial particularly those who are serverely hypoaemic / severe ARDS, with reductions in ICU mortality without increased airway complications.
- Explain to the patient, with reassurance, that they will be safe and obtain consent if they are able to communicate.
- Close eyes and protect with gel or pad.
- Place the patient's palms against their thighs, thumbs upwards, elbows straight and shoulders neutral.
- Slide the patient to the edge using a gliding sheet.
- Roll patient into the lateral position using the underneath sheet.
- Roll patient into prone.
- 'Swimmers position' (Fig. 1.1) - elbow in which the head is semi-rotated should be flexed to no more than 90° to avoid ulnar nerve stretch, and the other arm internally rotated by the side.
- Ensure that women's breasts or men's genitals are not compressed.
- Place two pillows under each shin to prevent peroneal nerve stretch, positioning them to avoid knee and toe pressure from mattress.
Extracorporeal Membrane Oxygenation (ECMO)
ECMO can be used for those patients who have severe respiratory failure and is used when conventional therapy cannot maintain adequate oxygenation. ECMO can fully replace the function of the lungs, however due to various compications there needs to be consideration of the risk vs benefit.
ECMO consists of an extracorporeal blood circuit formed via an oxygenator and a pump. Two vascular accesses are established, one removes the venous blood and one infuses the oxygenated blood. After the blood has been removed from a major vein, it is pumped through a circuit that contains an oxygenator which oxygenates the blood and removes the carbon dioxide. The blood is then returned via the other cannula.
Clinical Manifestations[edit | edit source]
The signs and symptoms of ARDS are characterized by severe defects in oxygenation requiring the use of mechanial ventilation and pulmonary edema with no underlying elevated left atrial pressures that ould explain the presentaton[8]. Because ARDS is used as an umbrella term to describe pulmonary dysfunction after a direct trauma or immune disorder, the clinical manifestations vary between professionals.
Physiotherapy [edit | edit source]
When treating a patient with ARDS, it is important to keep in mind that there will be both a physiological and psychological compenent to take into account. Because people suffering from ARDS will experience a difficult time to catch their beath, they will become highly anxious and stressed, which could exacerbate the condition. This is where physiotherapists play a key role in limiting the individual's psychological distress by educating the patient in regards to what they are going through as well as trying to keep the patient as calm as possible. With regards to the physiological management of the condition, there are several interventions that can be used to limit the negative effects of ARDS, which can include: positioning of the patient, suctioning, and the rehabilitation of muscle strength once the patient has recovered from the condition and are now focusing on returning to their original state.
Prevention Because ARDS is considered as a secondary condition, the way to prevent the onset is to prevent the primary condition from occurring. Based on the presenting risk factors of each patient, a score is given to identify those who are more at risk of developping ARDS, which can help to properly manage the progression of the condition[9]. Although it is difficult or imposibble to prevent some of the risk factors that may precipitate ARDS, such as genetic predisposition or direct trauma, some studies have analyzed ways to decrease the risk of developping ARDS. There is still little evidence to show the efficacy of physiotherapy interventions, there is more evidence which supports the use of pharmacological interventions to manage the pathogenic virulence factors.
Resources
[edit | edit source]
NHS - Acute Respiratory Distress Syndrome
Scholarly Article: Acute Respiratory Distress Syndrome Treatment & Management
Video: https://www.youtube.com/watch?v=ndrXtRmVkmE
References
[edit | edit source]
- ↑ Gibbons, C. Acute Respiratory Distress Syndrome. Radiologic Technology 2015; 86(4): 419-436
- ↑ Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994; 149(3 pt 1):818-824.
- ↑ Force, A.D.T., Ranieri, V.M. and Rubenfeld, G.D., 2012. Acute respiratory distress syndrome. Jama, 307(23), pp.2526-2533.
- ↑ Hough, A. 2014. Physiotherapy in respiratory and cardiac care: an evidence-based approach. Cengage Learning. 4th Edn.
- ↑ National Institutes of Health Services. ARDS. Available from http://www.nhlbi.nih.gov/health/health-topics/topics/ards
- ↑ Walkey, A., Summer, R., Vu. H., Alkana, P. Acute respiratory distress syndrome: epidemiology and management approaches. Clinical Epidemiology 2012; 4: 159-169
- ↑ National Heart, Lung and Blood Institute (2018). ARDS. Available at: https://www.nhlbi.nih.gov/health-topics/ards [Accessed 25th July 2018].
- ↑ Brochard, L. Does my patient really have acute respiratory distress syndrome (ARDS)?. Quarterly Medical Review 2011; 40(12): 541-542
- ↑ de Haro, C., Martin-Loeches, I., Torrents, A., Artigas, A. Acute respiratory distress syndrome: prevention and early recognition. Annals of Intensive Care 2013; 3(11)