Acute Care Assessment
Acute Care Assessment[edit | edit source]
Introduction[edit | edit source]
Physical Therapists or Physiotherapists (PTs) play an important role within the acute care hospital setting as core members of the multi-disciplinary teams that many hospitals utilize.
PTs in the acute care setting have several aims including the facilitation of discharge planning, safety and fall prevention, promotion of recovery, and reduction of length of stay through methods such as early mobilization.
As such, a Physical Therapy Assessment performed in the acute care setting includes some components that differ from other care settings.
Assessment Components[edit | edit source]
A Physical Therapy assessment in the acute care setting should follow the same basic structure as a physical therapy assessment in any other setting. There are many models of how best to approach a Physical Therapy assessment in general, but for the purposes here, focus will be kept on some of the components unique to the acute care setting.
Medical Record Review[edit | edit source]
PTs in acute care setting often have access to a significant amount of information about the current and past medical status of a given patient, thanks to the widespread use of electronic medical records.
Some of the most relevant information to collect can include:[1]
- Chief complaint/reason for hospitalization
- Surgical/procedure notes if applicable
- Recent nursing notes
- Specific physician or nursing orders that might impact assessment.
- Isolation precautions if applicable
- Movement precautions (sternal precautions, spinal precautions, etc.) if applicable
- Weight-bearing status if applicable
- Lab values
- Medications that might impact assessment
Interview[edit | edit source]
Ascertaining a patient’s prior level of function, before they entered the hospital, is very important. A patient’s prior level of function should be heavily taken into account when establishing appropriate goals for treatment.
Prior level of function information to collect can include:
- Durable medical equipment usage
- Independence level for ambulation
- Independence level for transfers
- Independence level for bed mobility
- Independence level for activities of daily living
Although not all patient’s will be appropriate to discharge from the hospital to home, it is still important to collect home environment information for all patients.
Note: home environment is not always the patient’s personal home, but the home that they plan to discharge to, if appropriate. This could be a friend or family member’s home.
Home environment information to collect can include:
- Type of home (single story, multi-story, apartment, mobile home, etc)
- Number of steps to get into home
- Number of steps inside home
- Position of handrails for any steps
- Type of bed
- Type of shower
- Available durable medical equipment
- Who will live with the patient upon discharge and their ability to assist if needed
- If living along, who will be available to assist if needed
Physical Exam[edit | edit source]
This is not an exhaustive list of physical exam components, but simply components particularly relevant to acute care.
Musculoskeletal: Strength and Range of Motion Screening[edit | edit source]
Important areas that can be examined:
- Hip flexion and extension[2]
- Knee flexion and extension[2]
- Ankle flexion and extension[2]
- Elbow and shoulder flexion and extension (ability to pull up and or support self with or without AD)[2]
It may not always be possible to assess all of these motions, but the goal is to ascertain if there are any limitations that might impact the patient’s ability to mobilize.
- Example one: If the patient only has trace contraction for right knee extension, they will only be able to bear a small amount of body weight through that leg and will need to compensate when ambulating.
- Example two: If the patient does not have range of motion of the left ankle, at least to neutral, it will reduce their ability to fully extend the left leg into a straight position to stand and the patient will have to compensate when ambulating.
Neurologic Screen[edit | edit source]
Specific neurological tests should be performed as clinically indicated.[2]
Coordination screening[edit | edit source]
Sensation screening[edit | edit source]
- Light touch at selected dermatomes[2]
Pain[edit | edit source]
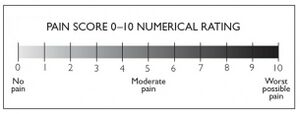
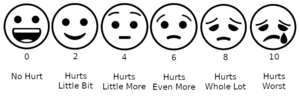
Baseline pain levels and those during activity should always be recorded.
Cardiovascular Screen[edit | edit source]
Many patients in the acute setting are often hemodynamically unstable. Therefore, obtaining baseline vital signs can help the PT to determine a patient's risk for abnormal cardiovascular events.[3] Blood pressure, respiration rate, and pulse rate should be recorded and monitored for every patient every time they are seen.[2] Oxygen saturation may also be obtained, especially for patients with cardiac or respiratory involvement.
Note: Physicians will sometimes provide vital sign ranges that the patient needs to remain within. It is important to be aware of these throughout the assessment.
Integument Screen[edit | edit source]
Patient’s in the acute care setting have often have surgical incisions and or invasive lines or tubes. Prior to movement, it is important to visually inspect any incision sites or entry/exit sites for lines or tubes. Following movement, these same sites should be reinspected for any changes. If any changes are noted, nursing staff should be notified.
Current level of function[edit | edit source]
Important areas that can be assessed:
- Supine to sit transfer
- Sit to stand transfer
- Stand to sit transfer
- Sit to supine transfer
- Toilet transfer
- Bed to chair transfer
- Ambulation ability
It is important to maintain any movement precautions that the patient may be under. At the time of initial assessment, the patient may require significant cueing to maintain these precautions.
Note: Remember that not every patient will be able to perform all of the above transfers or may not be to the point of being able to ambulate.
During transfers and ambulation, be sure to let the patient perform as much as they can without assistance. If the patient is unable to perform a movement by themselves, assistance should be given, but only as much as is needed to complete the movement. Be sure to record the level of assistance given for each transfer and for ambulation as applicable.
The patients performance constitutes current level of function and should be combined with prior level of function for goal setting.
Outcome Measures[edit | edit source]
Functional[edit | edit source]
- Barthel Index
- Elderly Mobility Scale
- Rivermead Mobility Index
- AM-PAC 6 Clicks Score (see materials and methods section for description)
Mobility[edit | edit source]
Balance[edit | edit source]
Role of PT globally[edit | edit source]
Various studies have reported similarities in the structure and role of physical therapy in acute care internationally across health systems in the United States, the United Kingdom and Europe, Canada, South Africa, South America (particularly Brazil), India, Singapore, Hong Kong, Japan, and Australia and New Zealand, with ongoing evolution of the role across Asia.[4]
United States[edit | edit source]
In the United States, aside from promoting recovery and mobility through various forms of PT intervention (gait training, muscular strengthening, durable medical equipment training, etc), one of the main roles of PTs in the acute care setting is the facilitation of discharge planning and preparation.[1] This means making a recommendation on the most appropriate discharge setting based on the patient’s unique situation and characteristics as well as the therapist’s clinical judgement. Then providing treatment to ensure that the patient is functionally ready for the ultimately decided upon discharge setting.
Discharge setting recommendations often include inpatient rehabilitation (at a dedicated rehabilitation hospital), short-term rehabilitation (often at a skilled nursing facility), assisted living/long term care, or home.[1]
If the patient is discharging home, PTs in the acute setting are also often tasked with making recommendations as to the need for additional Physical Therapy services post discharge. These can include home health physical therapy, outpatient physical therapy, home environment evaluations, and/or cardiopulmonary rehabilitation.
For patients discharging home, PTs are also often responsible for making recommendation for appropriate durable medical equipment such as walkers, wheelchairs, bedside commodes, shower chairs, etc.
England[edit | edit source]
In England from the 21st of August 2020 all NHS hospitals are working towards a new Discharge to Assess Model (D2A). For those admitted to an acute hospital, 95% are expected to be discharged home as default. The Discharge to Assess Model sets out 4 pathways:
- 50% of people are expected to be discharged home with the same level of support on admission or with voluntary and community support, Pathway 0.
- 45% of people are expected to be discharged home with up to six weeks recovery support from health and social care services, to maximise their independence and stay home for longer, Pathway 1.
- 4% of people are expected to be discharged to bedded rehabilitation settings to support their return home, Pathway 2.
- 1% of people are expected to be discharged into long-term care settings, such as a care home, Pathway 3.[5]
The aim of the new D2A process is to begin discharge planning from the point of hospital admission where appropriate, including the identification of immediate needs of the individual at home following discharge. Information about the home circumstances for people should be collected at the point of admission. If further home assessment is required this should be undertaken in good time, coordinated between health and social care and should include equipment and reablement support.
Funding (England)[edit | edit source]
Additional care (more than needed on admission) and support needs for all individuals on discharge from hospital (where required) will be provided free of charge for up to six weeks to allow for post- discharge recovery and support services, and any assessments of ongoing care needs and financial eligibility determinations to be made.
The role of an Acute Therapists (England)[edit | edit source]
Acute Therapist are considered PTs, Occupational Therapists and Therapy Practitioners and Assistants
- A significant part of the role will be in non-acute settings (mainly in people’s homes)
- Complete limited assessments for discharge during admission.
- Telephone the following day after discharge to check and offer reassurance/advice.
Roles may include:
- Taking on the case management role and undertake the first assessment at home of a person.
- Acute therapists will assess people in their own home/usual place of residence at the request of the single coordinator and agree a recovery and support plan with the person including reablement support and/or equipment.
- This will be a trusted assessment which will be accepted by the receiving care provider (agreement as to universal document to be used across acute and community services).
- Working much more fluidly between community settings, people’s homes and within the acute trust, depending on the capacity demands.
- A 7 day service will be required to achieve the D2A's goals.[6]
Resources[edit | edit source]
- NICE; Transition between inpatient hospital settings and community or care horme settings for adults with social care needs
- QUICK GUIDE: DISCHARGE TO ASSESS
- Why not home? Why not Today?
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Avers D, Wong R. editors. Guccione’s Geriatric Physical Therapy. Fourth Edition. St. Louis, Missouri: Elsevier, 2020.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Fruth S. Fundamentals of Physical Therapy Examination. Second Edition. Burlington, Massachusetts: Jones & Bartlett Learning, 2018.
- ↑ Levenhagen k, Norris T, Fick A, Albeyta Campbell A, Frese E, Lopker M, Poole A. APTA Academy of Cardiovascular and Pulmonary Physical Therapy. ADULT VITAL SIGN INTERPRETATION IN ACUTE CARE GUIDE 2021. Pittsburgh, PA: APTA, 2021.
- ↑ Lau B, Skinner EH, Lo K, Bearman M. Experiences of physical therapists working in the acute hospital setting: systematic review. Physical therapy. 2016 Sep 1;96(9):1317-32.
- ↑ https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/912199/Hospital_Discharge_Policy_1.pdf
- ↑ Hospital Discharge Service Requirements https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/911214/Hospital_discharge_service_requirements_action_cards.pdf