Hill Sachs Lesion
Original Editors - Lien Hennebel
Top Contributors - Jelle Van Hemelryck, Lien Hennebel, Leana Louw, Pauline Bouten, Simisola Ajeyalemi, Uchechukwu Chukwuemeka, Lucinda hampton, Shreya Pavaskar, Admin, Kim Jackson, Rachael Lowe, Fasuba Ayobami, Wanda van Niekerk, Nupur Smit Shah, 127.0.0.1 and Claire Knott
Clinically Relevant Anatomy
[edit | edit source]
The term 'Hill-Sachs Lesion', refers to the glenohumeral joint [link to: http://www.physio-pedia.com/Glenohumeral_Joint], which is a synovial ball-and-socket diarthroidal joint. It is the articulation between the fossa glenoidalis of the scapula and the caput humeri. It’s common known that the shoulder joint has a real loose capsule and that therefore the risk for dislocation is severely high. [4][5]
* The bony part: the scapula with his glenoid and the humeral head from the humerus; The humerus is the “ball” of the ball-and-socket joint. This one is located in the “socket” (glenoid) which forms the shoulder joint. The scapula is a triangular shaped bone that forms the “socket” in the joint. [6] [7]
* The fibro cartilaginous structure surrounding the glenoid, namely the labrum; The labrum makes sure there is enough contact between the surface of the glenoid and the humeral head. There is a concavity compression mechanism which plays an important role in the stability of the shoulder. The less contact there is, the more chance there is for dislocations.[8]
* The capsule and ligamentous structures: Glenohumeral Ligaments (pars superior, media and inferior), which are meant for the strengthen of the capsule. Coracohumeral Ligament: is also meant for the strengthen of the capsule. [2] Transversal humeral ligament: is meant for M. Biceps Brachii [5]
* Muscles: Abductors: M. deltoideus and M. Supraspinatus Adductors: M. Pectoralis Major Flexors: M. Deltoid Rotator Cuff (very important for the stability of the art humeri): M. supraspinatus, M. infraspinatus, M. Teres Minor, M. Subscapularis Extensors: M. Deltoid, M. Triceps Brachii, M. Teres Major, M. Latissimus Dorsi Internal Rotators: M. Teres Major, M. latissimus dorsi, M. Subscapularis, M. Pectoralis Major External Rotators: M. Teres Minor and M. Infraspinatus. [9]
* Bursae: There are eight bursae in the shoulder complex. [4] This is because of the high amount of muscles on the shoulder. They make sure there is a smooth contact between the muscle and the underlying structure. The biggest one in the body is the subacromial
Mechanism of Injury / Pathological Process
[edit | edit source]
The glenohumeral joint is the most commonly dislocated joint in the human body and 90% of shoulder dislocations are anterior. The reason for this is that the scapula is oriented about 30 degrees anterior and this to the coronal plane of the body. Because of this the glenohumeral joint with the humerus is orienting anterior to the glenoid.[1]
When a trauma takes place, an anterior shoulder dislocation can cause a head impression fracture what we call a Hill sachs lesion. The posterolateral aspect of the humeral head impacts on the anterior glenoid in the dislocated position, what makes the glenohumeral joint unstable (Shoulder_Instability). [2][3][4]
90% of shoulder dislocations are anterior, so in some cases there could be a posterior dislocation what can cause a reverse Hill sachs lesion. This lesion may be present on the anterior aspect of the humeral head. [4]
Clinical Presentation[edit | edit source]
Shoulder dislocation don’t occur isolated. It causes damage to different tissues surrounding the glenohumeral joint like shoulder ligaments, rotator cuff tendons and the joint capsule. But the bone and cartilage of the humeral head can also be affected. This occurs when the round humeral head is forcibly impacted on the edge of the glenoid, which causes compression fractures in the humeral head. This forms a dimple structure on the articular surface of the humerus, and is called a Hill-Sachs lesion. It can be seen on MRI, CT-scan, but is difficult to see on an x-ray. [13][14][15]
We can order this humeral head compression fractures according to the percentage of humeral head involvement [11]
• minor defect: less than 20% of the humeral head is involved;
• moderate defect: between 20% and 45% of the head is involved;
• severe defect: more than 45% of the head is involved.
The size of the lesion is in most cases related to the amount of times a dislocation took place[16]
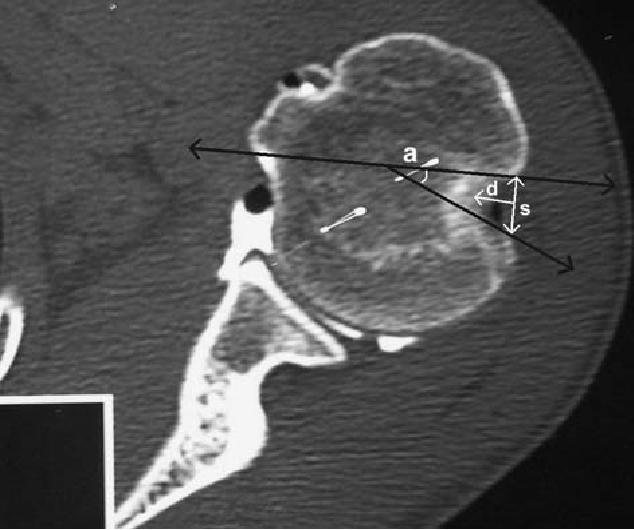
Figure 1 illustrates how the percentage of the humeral head, which is involved, is calculated. Next to this percentage, a Hill-Sachs lesion is also characterized by its depth ('d' on figure 1) and its size ('s' on figure 1).
Figure 1: preoperative double contrast CT arthrography of a 20 year old patient. [11]When we diagnose a Hill-Sachs defect, we can be sure that there was a complete dislocation of the humeral head out of the socket, and that it was not just a subluxation. [13]
A Hill-Sachs lesion occurs in about 50 percent of the first-time shoulder dislocations. For people with a shoulders dislocations’ history (= shoulder instability) you can almost always see these humeral head compression fractures. [15] There is a link between bone loss on either the glenoid side or the humeral side and recurrent shoulder instability during activities. [16]
Diagnostic Procedures[edit | edit source]
When a patient whit Hill sachs lesion knocks on the door of a physiotherapist, the physiotherapist can ask some questions to his patient (history), looking to both shoulders (atrophy, asymmetry, surgical scars...), implements some passive movements (forward flexion and elevation, abduction, internal and external rotation) after which the patient is doing this movements active... Classicaly the patient with recurrent dislocation has a normal range of motion, but at some degree you will see a 'risk position'. Now, the physiotherapist know there is some instability, but there is no sign that the patient has an Hill sachs lesion. [1]
For the identification of a Hill sachs lesion, you need specific views to demonstrate the lesion. When the use of MRI (Magnetich Resonance imaging) an CT arthrography increased, for the diagnosis of a Hill sachs lesion, a higher incidence has been reported. It's important that a physiotherapist knows that there could be some concomitants which are only visible through MRI...[3]
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
When patients have a small or moderate defect of the humeral head, it tends to be neglected. Surgical treatment is no necessity. So, there is no need of surgical treatment, but important is handle the result, the unstability.[3]
The non-operative rehabilitation of the unstable shoulder consists about seven key factors: [4]
- Onset of pathology (in this case: traumatic event)
- Degree of instability (in this case: dislocation)
- Frequency of dislocation (in this case acute)
- Direction of instability (in this case: anterior)
- concomitant pathologies (in this case: Hill sachs lesion)
- Neuromuscular control
- Activity level
In the non-operative rehabilitation program of the traumatic dislocation of the shoulder, it's important to consider all these seven factors and thus also with the concomitant 'Hill sachs lesion': rehabilitation program of the shoulder
Some studies say that: 'there is no relationship between the number of dislocations and Hill sachs lesion'. But several studies have shown that when the number of dislocations increases, the incidence and size of Hill sachs lesion also increases. It can be a cause of instability and in this case surgical treatment is considered. Frequently, authors consider that surgical treatment of recurrent shoulder dislocation is indicated when someone had more than five shoulder dislocations. [3][5]
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
Resources
[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 Cite error: Invalid
<ref>tag; no text was provided for refs namedNepola - ↑ W.T. Gooding, B., M. Geoghegan, J., A. Manning, P., 'The management of acute traumatic primary anterior shoulder dislocation in young adults', Jornal compilation: British elbow and shoulder society, 2010, p. 141-146 (Level of evidence 1A)
- ↑ 3.0 3.1 3.2 3.3 Cetik, O., Uslu, M., K. Ozsar, B., 'The relationship between Hill sachs lesion and recurrent anterior shoulder dislocation', Acta orthopaedica Belgica, VOL. 73 (2007), p. 175-178
- ↑ 4.0 4.1 4.2 E. Wilk, K., C. Macrina, L., M. Reinold, M., 'Non-operative rehabilitation for traumatic and atraumatic glenohumeral instability', North american journal of sports physical therapy, VOL. 1 (2006), februari, nr. 1, p. 16-31
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedCutts