Wilson's Disease: A Case Study
Original Editor -Yuka Abe
Top Contributors - Courtney Lim, Jocelyn Chung
Abstract[edit | edit source]
Introduction[edit | edit source]
Client Characteristics[edit | edit source]
Examination Findings[edit | edit source]
Outcome Measures[edit | edit source]
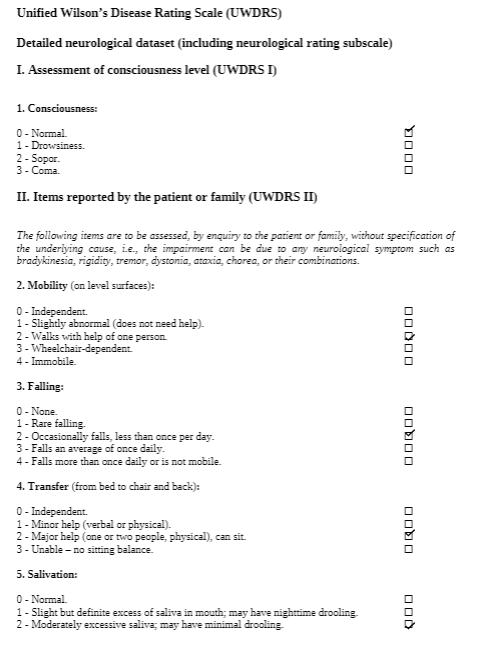
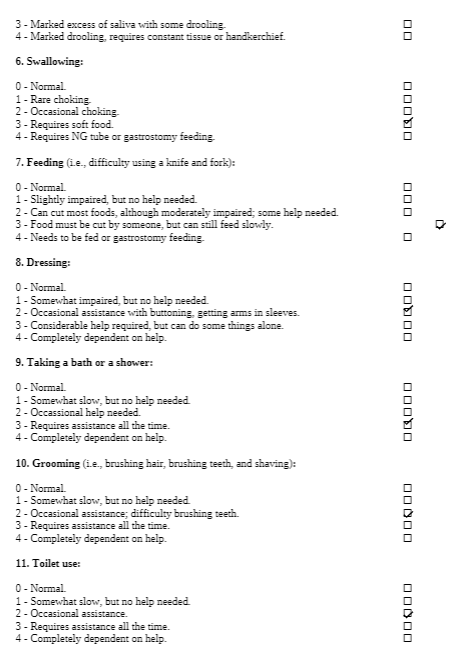
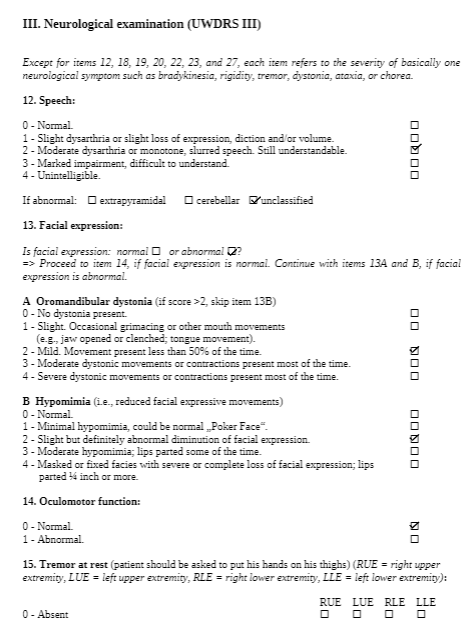
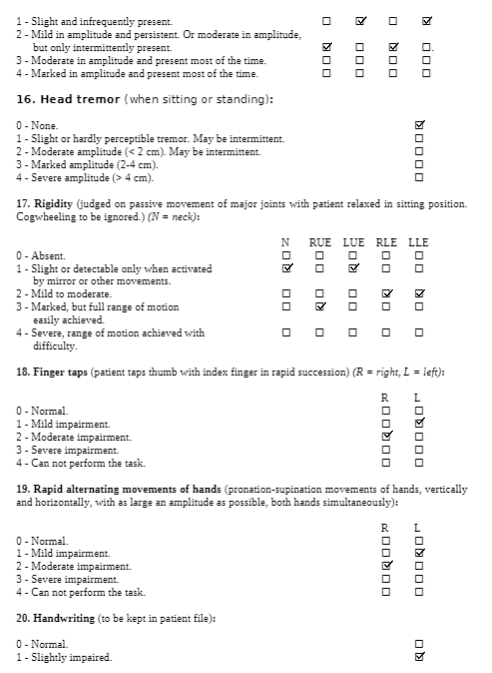
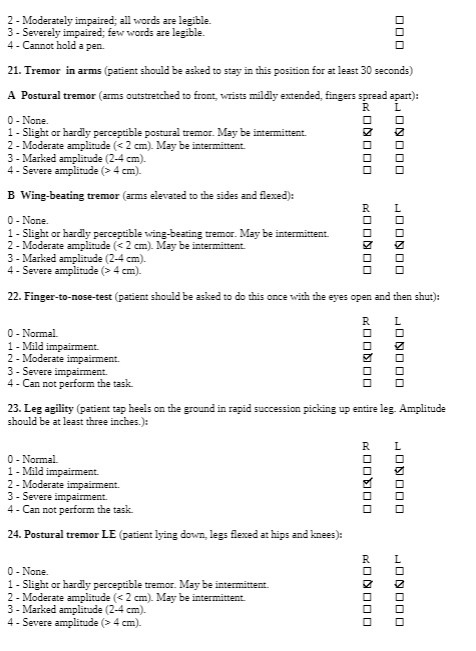
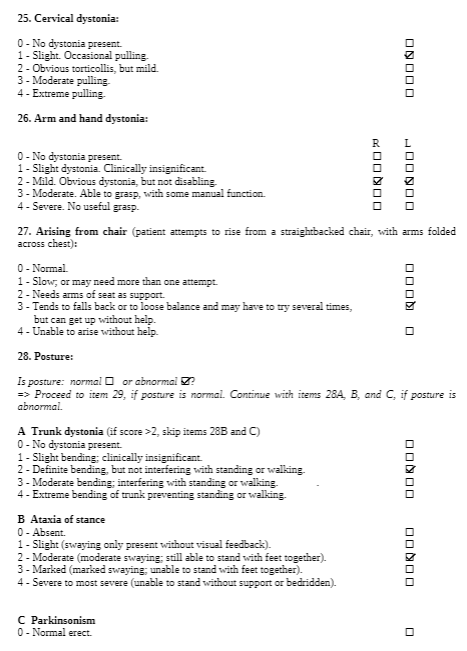
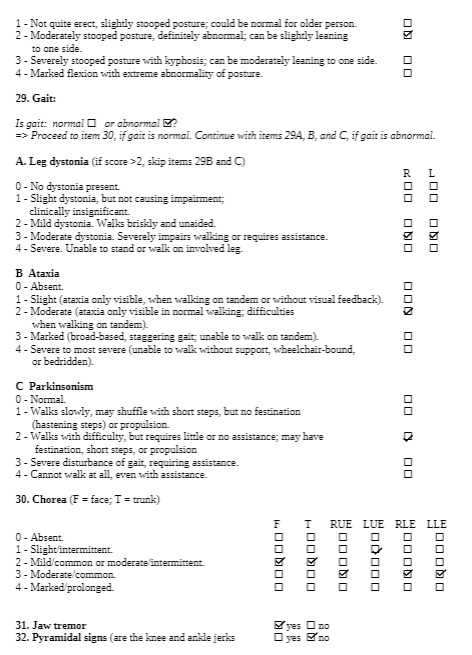
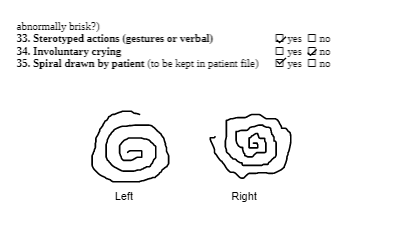
The Unified Wilson’s Disease Rating Scale (UWDRS) would be appropriate for this patient in measuring the body structure and function limitations. The UWDRS consists of 3 subscales – neurological, hepatic, and psychiatric. The neurological subscale consists of items including rigidity, chorea, tremors, as well as facial expression and oromandibular dystonia. The UWDRS has been shown to be a reliable and valid tool to monitor disease progression in patients with Wilson’s disease [1]. Items on the UWDRS were adapted from scales that have already been established in measuring neurological impairments, including the Unified Parkinson’s Disease Rating Scale (UPDRS), Barthel index, and the Unified Huntington’s Disease Rating Scale, which suggests a high degree of content validity[1].
To evaluate the activity limitation, the 2 Minute Walk Test (2MWT) can be used. The 2MWT measures the distance walked in 2 minutes, and can be used to quantify walking limitations and fatigue. This measure has been proven to be reliable and valid in patients with various neuromuscular diseases[2]. In addition, the 2MWT is well correlated with the 6 Minute Walk Test, which is a widely used and validated tool in measuring walking capability. For this case, the patient is currently unable to walk without assistance, so the 2MWT would be administered when the patient is able to walk independently.
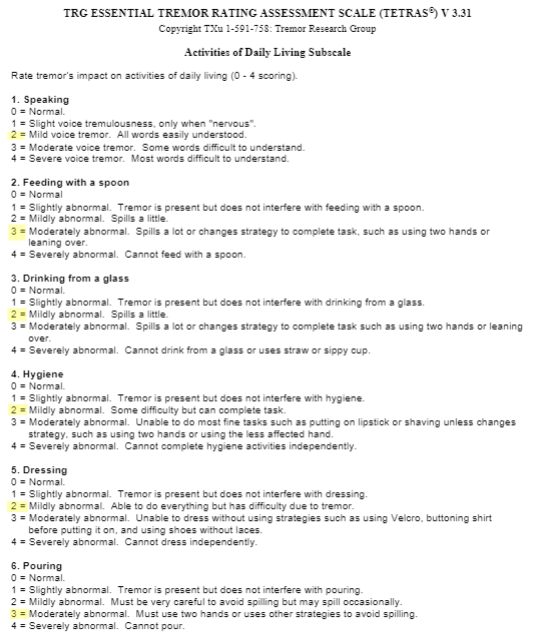
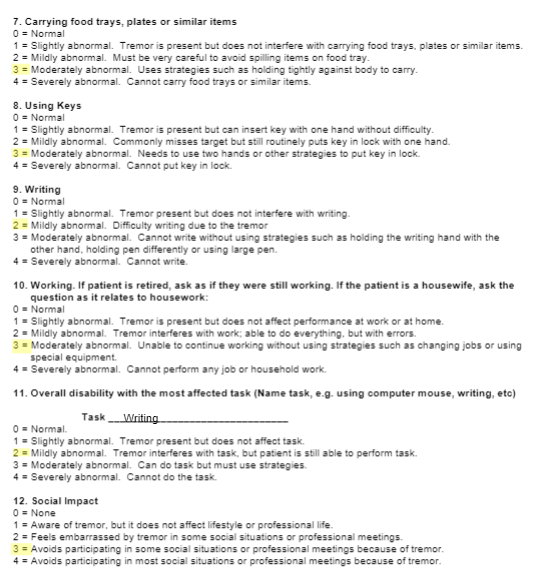
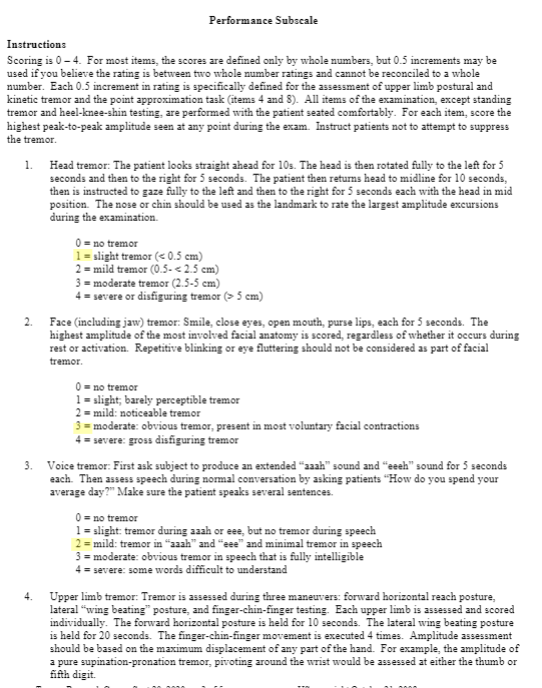
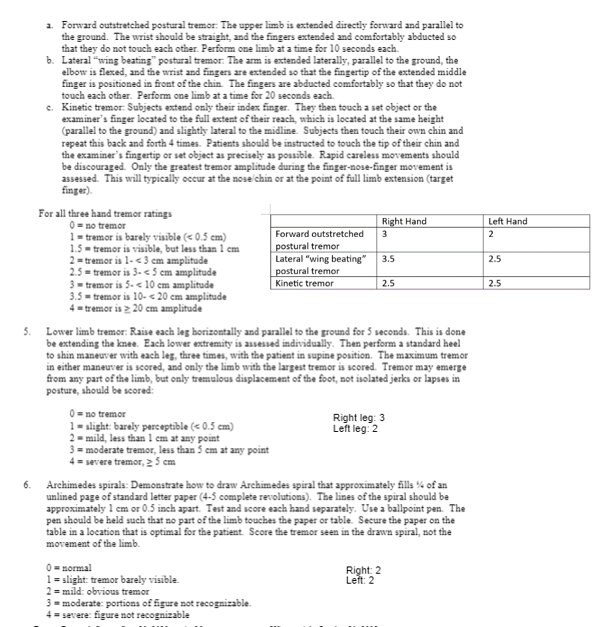
For participation limitations, the Tremor Research Group Essential Tremor Rating Scale (TETRAS) can be used to measure essential tremors. The TETRAS consists of ADL (12 items) and performance (9 items) sections[3]. Each item is scored on a scale of 0 to 4, where a higher score indicates more severe tremors. It is a well-validated and reliable tool to assess the severity of essential tremors, which is commonly present in those with Wilson’s Disease[4][5] . Furthermore, the TETRAS assesses wing-beating tremors which is characteristic of Wilson’s Disease.
Common Comorbidity to Screen For[edit | edit source]
Psychiatric disorders, specifically depression, is a common comorbidity that should be screened in patients with Wilson’s Disease (WD). Evidence shows that there is a higher prevalence of depression in those with WD as compared to those with other chronic diseases that live with a similar level of disability[6]. Psychiatric disorders as a comorbidity have a poorer prognosis as these complicate the course of WD with significant impact on quality of life[7]. Therefore, it is necessary to screen depression in patients with WD. Physiotherapists (PT) can use many assessments, such as Beck’s Depression Inventory, a self-reported scale, to which the PT can refer on if necessary.
Clinical Hypothesis[edit | edit source]
Intervention[edit | edit source]
Virtual reality (VR) is a new and upcoming innovative technology that has been shown to help facilitate and improve the rehabilitation process. Virtual reality uses principles of neuroplasticity and motor learning and utilizes computer algorithms to make decisions towards progressing the difficulty of a task. It has the ability to track neuroplastic changes and can be used to track recovery. Studies have shown VR to have great ecological validity and researchers have been steadily improving its technology (e.g higher resolution 3D systems are more prevalent). For instance, new research has worked to improve head mounted displays, allowing these displays to produce realistic, high resolution augmented visual feedback. This visual feedback can help with sensorimotor integration and thus help the patient improve their gait. Our patient, Chris Brown, presents with gait impairments. VR technology can be used to help in the treatment process of our patient’s gait patterning. Another applicable example is that VR can be used to improve upper extremity functioning and fine motor control by providing hepatic feedback to the patient. This can also help to facilitate Chris Brown's rehabilitation process. VR is a fresh new rehabilitation approach that can be engaging for patients and could help with motivation.
Despite the benefits that VR can bring, it does come with a few challenges. Two of the most pressing issues include accessibility issues due to expensive equipment costs and safety issues and considerations.
To mitigate costs barriers associated with VR systems, facilities/clinicians can work with researchers in pilot programs. This is a great way for the clinician and facilities to see if VR is suitable for their patient population while assessing if VR would be a reasonable investment that ultimately will save money in the long-term. Cost barriers can also be addressed by using alternative materials such as a cardboard headset. Some VR training content could also be used in a more accessible form such as on a desktop or mobile device.
To mitigate issues with safety, proper clinician training and education would be appropriate. To use VR, there could be requirements such as completion of a training course or passing a specific exam. The patient also needs to be given proper comprehensive education and informed consent. Side effects of VR can include cybersickness, perceptuomotor after-effects, headaches and eye-strain. The patient is also at risk for addiction to VR-based technologies. The patient should be informed of both benefits and drawbacks of the treatment, as well as alternative solutions. This can help to ensure safety and proper usage of VR systems by both patient and practitioner.
Goals[edit | edit source]
Problem 1: Unable to achieve optimal flexion in the lower extremity, especially dorsiflexion of the ankle
- Short term goal: In 2 weeks, Chris will be able to increase dorsiflexion at the ankle to 10 degrees as measured by goniometry
- Long term goal: Chris will be able to heel strike in his gait cycle without an AFO for discharge
Problem 2: Dyskinesia, affecting his ability to use his face and mouth muscles voluntarily
- Short term goal: In 2 weeks, Chris will have voluntary control of his face muscles as shown by a smile on his face
- Long term goal: Chris will have voluntary control of his mouth muscles as he will be able to chew solid foods for two meals a day for discharge
Problem 3: Hypertonia, specifically rigidity, chorea and tremors
- Short term goal: In 2 weeks, Chris will be able to pick up a glass of water with minimal tremors as measured by minimal spillage of water
- Long term goal: Chris will be able to feed himself independently for discharge
Problem 4: Unable to walk without moderate amount of assistance due to muscle fatigue and lack of balance and coordination
- Short term goal: In 2 weeks, Chris will improve standing balance as measured with improvement on the BERG balance scale
- Long term goal: Chris will be able to walk 30 meters independent with a gait aid for discharge
Problem 5: Unable to golf with his friends on the weekends due to essential tremors
- Short term goal: In 2 weeks, Chris will be able to put a golf ball 1 meter away from the putter
- Long term goal: Chris will be able to perform a golf swing with a golf club for discharge
Discharge date: projected 6 months from admission to outpatient rehabilitation – will be dependent on trajectory of patient progression.
Outcome[edit | edit source]
UWDRS Outcome:
UWDRS Score Part I: 0
UWDRS Score Part II: 23
UWDRS Score Part III:
2MWT: Unable to complete at this time as patient requires assistance when walking
TETRAS Outcome:
TETRAS Score ADLs: 30
TETRAS Score Performance: 39.5
Referrals[edit | edit source]
3 other healthcare professionals/services that can be involved in the client’s care include:
-speech language pathology
-occupational therapy
-psychiatric care and counseling
Speech language therapy would be the priority recommendation for Chris Brown as they address problems regarding communication, swallowing, and eating. The most pressing issue would be swallowing and eating as these skills are crucial for survival and it is important to know the patient’s functional level to provide adequate support and mitigate risks such as aspiration or choking. The speech language therapist can assess oral muscle functioning and strength for speaking and swallowing. Based off this information, they can make recommendations for an appropriate diet and can create a treatment plan to help improve independence with eating and swallowing. The speech language therapist can help with verbal and non-verbal communication, recovery of speech, language, and memory skills. These skills are essential for daily living and improving these skills will contribute to an overall improved quality of life and well-being. Working on these skills will be instrumental in success with other therapies (physical therapy, occupational therapy, psychiatric care and counseling).
Discussion[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Leinweber, B., Möller, J. C., Scherag, A., Reuner, U., Günther, P., Lang, C. J. G., Schmidt, H. H. J., Schrader, C., Bandmann, O., Czlonkowska, A., Oertel, W. H., & Hefter, H. (2008). Evaluation of the Unified Wilson’s Disease Rating Scale (UWDRS) in German patients with treated Wilson’s disease. Movement Disorders, 23(1), 54–62. https://doi.org/10.1002/mds.21761
- ↑ Andersen, L. K., Knak, K. L., Witting, N., & Vissing, J. (2016). Two- and 6-minute walk tests assess walking capability equally in neuromuscular diseases. Neurology, 86(5), 442–445. https://doi.org/10.1212/WNL.0000000000002332
- ↑ Elble, R. J. (2016). The Essential Tremor Rating Assessment Scale. Journal of Neurology & Neuromedicine, 1(4). https://www.jneurology.com/articles/the-essential-tremor-rating-assessment-scale.html
- ↑ Ondo, W., Hashem, V., LeWitt, P. A., Pahwa, R., Shih, L., Tarsy, D., Zesiewicz, T., & Elble, R. (2018). Comparison of the Fahn-Tolosa-Marin Clinical Rating Scale and the Essential Tremor Rating Assessment Scale. Movement Disorders Clinical Practice, 5(1), 60–65. https://doi.org/10.1002/mdc3.12560
- ↑ Ortiz, J. F., Morillo Cox, Á., Tambo, W., Eskander, N., Wirth, M., Valdez, M., & Niño, M. (n.d.). Neurological Manifestations of Wilson’s Disease: Pathophysiology and Localization of Each Component. Cureus, 12(11), e11509. https://doi.org/10.7759/cureus.11509
- ↑ Ehmann, T.S., Beninger, R.J., Gawel, M.J., & Riopelle, R.J. (1990). Depressive symptoms in Parkinson's disease: A comparison with disabled control subjects. Journal of Geriatric Psychiatry and Neurology, 3, 3–9. doi:10.1177/ 089198879000300102
- ↑ Carta, M.G., Mura, G., Sorbello, O., Farina, G., & Demelia, L. (2012). Quality of life and psychiatric symptoms in Wilson's Disease: The Relevance of Bipolar Disorders. Clinical Practice & Epidemiology in Mental Health, 8, 102–109